- Department of Neurosurgery, Saiseikai Utsunomiya Hospital, Utsunomiya, Japan
Correspondence Address:
Joji Inamasu, Department of Neurosurgery, Saiseikai Utsunomiya Hospital, Utsunomiya, Japan.
DOI:10.25259/SNI_1123_2024
Copyright: © 2025 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Joji Inamasu, Sota Wakahara. Recurrent chronic subdural hematoma with trabeculae converging toward a burr hole. 07-Feb-2025;16:42
How to cite this URL: Joji Inamasu, Sota Wakahara. Recurrent chronic subdural hematoma with trabeculae converging toward a burr hole. 07-Feb-2025;16:42. Available from: https://surgicalneurologyint.com/surgicalint-articles/13366/
Abstract
Background: Radiographically, trabeculae have been observed commonly in chronic subdural hematoma (CSDH) patients. Nevertheless, few authors have focused on how the trabeculae develop. We, herein, report a case of recurrent CSDH in which the evolution of trabeculae was observed with serial brain computed tomography.
Case Description: A 75-year-old man with symptomatic left-sided CSDH who had undergone a burr-hole craniostomy 14 days in our institution earlier came back with a recurrent CSDH with trabeculae within the hematoma cavity. The trabeculae, which had not been present in the first surgery, developed relatively rapidly, converging toward the burr hole. The recurrent CSDH was successfully treated with the middle meningeal artery embolization. During the procedure, a vascular brush was observed around the burr hole, indicating the trabeculae were rich in blood flow.
Conclusion: Surgical manipulation of the outer membrane during the first surgery might likely have elicited local inflammation and subsequent neovasculization of the outer membrane, resulting in trabeculae formation around the burr hole.
Keywords: Burr hole, Chronic subdural hematoma, Middle meningeal artery embolization, Trabecula
INTRODUCTION
Radiographically, trabeculae have been observed commonly in chronic subdural hematoma (CSDH) patients. Nevertheless, few authors have focused on how the trabeculae develop.
CASE DESCRIPTION
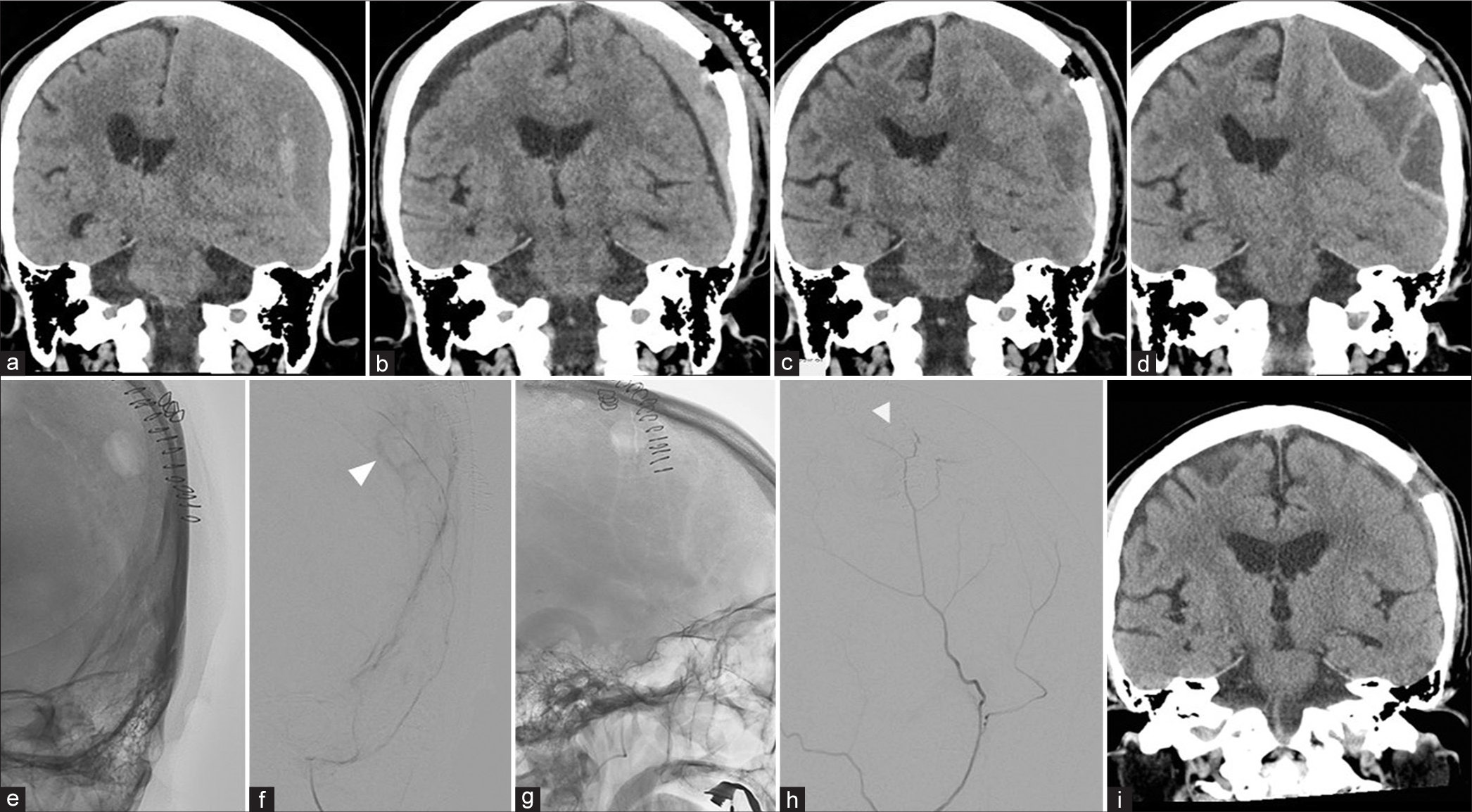
A 75-year-old man presenting with motor aphasia was found to have a left-sided CSDH with heterogenous density compressing the adjacent brain [
Figure 1:
(a) A left-sided chronic subdural hematoma (CSDH) with heterogenous density compressing the adjacent brain. (b) A postoperative day (POD)-1 computed tomography (CT) in a coronal view shows a reduction in the CSDH volume and midline shift. (c) A POD-14 CT shows the formation of a high-density clot-like structure beneath the burr hole. (d) A POD-21 CT showing the convergence of trabeculae toward the burr hole. (e) A selective digital subtraction angiography during the left middle meningeal artery embolization showed vascular staining and MMA branches encircling the burr hole. (f) Lateral scout view (an arrowhead showing the burr-hole). (g) Lateral view, capillary phase. (h) Anteroposterior (AP) scout view (an arrowhead showing the burr-hole). (i) AP view, late arterial phase. A CT 2 months after embolization showed the disappearance of both trabeculae and hematoma.
Radiographically, trabeculae have been observed relatively frequently in CSDH patients. While Wakuta et al. reported that the trabeculae had been associated with a high postoperative recurrence rate,[
CONCLUSION
Surgical manipulation of the outer membrane during the first surgery might likely have elicited local inflammation and subsequent neovasculization of the outer membrane, resulting trabeculae formation around the burr hole.
Ethical approval
Institutional review board (IRB) permission is not required for the study.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Javed Z, Abid M, Shamim SM. Chronic subdural hematoma needs to be named differently. Surg Neurol Int. 2024. 15: 164
2. Takei J, Hirotsu T, Hatano K, Ishibashi T, Inomata T, Noda Y. Modified computed tomography classification for chronic subdural hematoma features good interrater agreement: A single-center retrospective cohort study. World Neurosurg. 2021. 151: e407-17
3. Wakuta N, Abe H, Fukuda K, Nonaka M, Morishita T, Arima H. Feasibility and safety of endoscopic procedure in burr-hole surgery for chronic subdural hematoma in patients of very advanced age. World Neurosurg. 2020. 134: e1037-46