- Department of Orthopedic Surgery, Akita University Graduate School of Medicine, 1-1-1 Hondo, Akita 010-8543, Japan.
DOI:10.25259/SNI_194_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Yoshinori Ishikawa, Naohisa Miyakoshi, Michio Hongo, Yuji Kasukawa, Daisuke Kudo, Yoichi Shimada. Recurrent dysphagia after lower posterior cervical fusion. 16-May-2020;11:114
How to cite this URL: Yoshinori Ishikawa, Naohisa Miyakoshi, Michio Hongo, Yuji Kasukawa, Daisuke Kudo, Yoichi Shimada. Recurrent dysphagia after lower posterior cervical fusion. 16-May-2020;11:114. Available from: https://surgicalneurologyint.com/surgicalint-articles/10030/
Abstract
Background: Although dysphagia following posterior craniocervical fixation is well known, the incidence after mid-lower posterior cervical fixation is not well described. Here, we presented a case of recurrent dysphagia in a 72-year-old male following C3–T3 posterior cervical fixation and discussed its etiology.
Case Description: A 72-year-old male sustained a cervical fracture in a fall; he was neurologically intact. The cervical/thoracic MR and CT studies documented ankylosing spondylitic changes in the cervicothoracic spine, a C5/6 disc herniation, and a C7 vertebral fracture. He underwent posterior cervical C3 to T3 fusion without decompression. For the 1st postoperative day, he complained of dysphagia without hoarseness, and fiberoptic endoscopy revealed poor esophageal mobility. For the next 6 postoperative years, he continued to require repeated attempts at the dilation of the esophageal entrance but remained reliant on a feeding tube.
Conclusion: Posterior cervical fixation restricts cervical motion and may restrict expansion of the esophageal duct leading to permanent postoperative dysphagia requiring continued feeding tube utilization.
Keywords: Ankylosing spine, Cervical motion, Dysphagia, Ossification, Posterior cervical fixation
INTRODUCTION
Dysphagia after posterior spinal fixation has been frequently reported in craniocervical lesions, However, it is rare following mid-lower cervical surgery.[
CASE REPORT
A 72-year-old male with a history of resection of the OALL due to dysphagia (i.e. still able to eat orally) presented with a cervical fracture due to a fall.
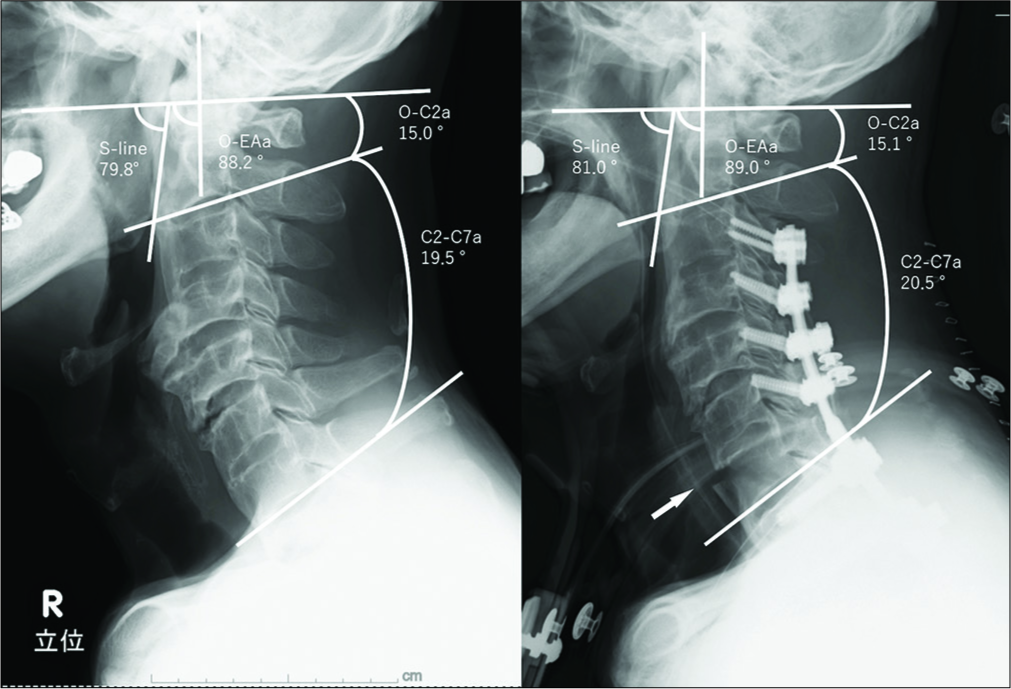
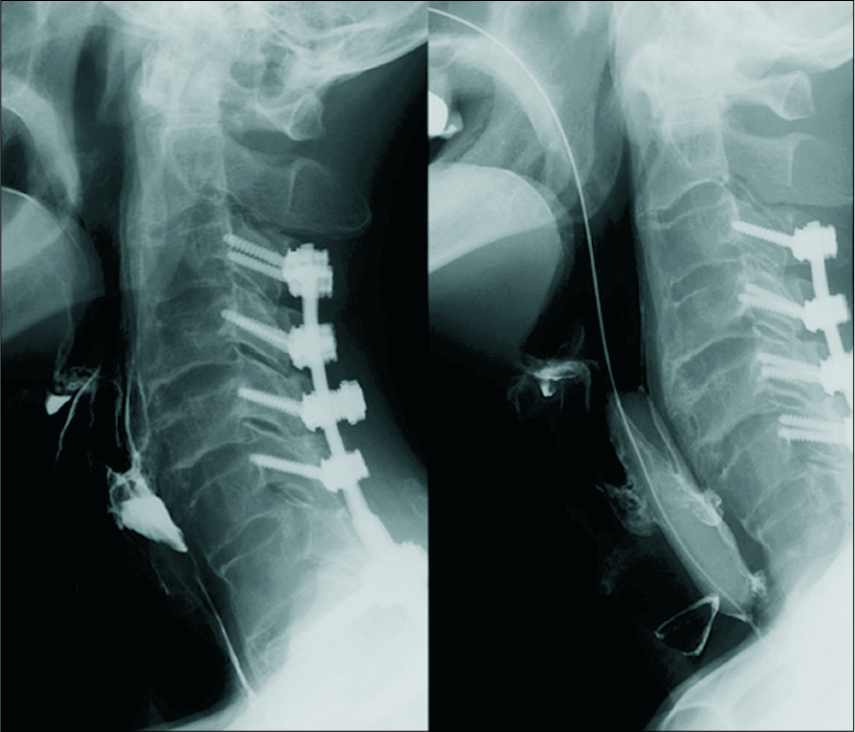
The MR and CT studies documented ankylosis from C2 to C4 and C6 to the thoracic spine, a disc herniation at C5/6, and a C7 vertebral fracture. On the day of admission, the patient underwent an emergent in situ PCF from C3 to T3 without reduction or decompression [
The video fluoroscopic evaluation showed pooling of contrast at the epiglottic vallecula and inflow into the trachea [
DISCUSSION
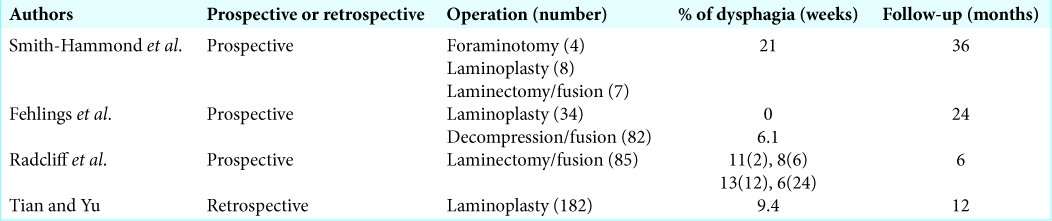
A PubMed search showed a few reports on dysphagia after posterior cervical surgery in the mid-lower cervical spine occurs from 0% to 21% of the time [
Causes of dysphagia following PCF
There are multiple potential causes of dysphagia following PCF. Chen et al. reported that patients with dysphagia had significantly greater C2–C7 lordosis.[
The O-C2 angle (the angle between McGregor’s line and the inferior endplate of C2), S-line (the angle between McGregor’s line and the line that links the center of the C1 anterior arch and the apex of cervical sagittal curvature), and O-EA angle (the angle between McGregor’s line and the line joining the external auditory canal and the middle point of the caudal endplate of C2) have been reported to prevent postoperative dysphagia after occipitocervical (OC) fusion.[
Radcliff et al. reported that PCF might result in dysphagia due to the loss of cervical motion.[
17–28% Incidence of dysphagia with spinal ankylosis
The incidence of dysphagia with ankylosing spinal hyperostosis itself is 17–28%.[
CONCLUSION
Before performing subaxial PCFs in a patient with prior anterior cervical procedures for multilevel OALL, one should carefully assess the extent and severity of dysphagia to avoid a patient permanently reliant on a gastric feeding tube.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We thank Ellen Knapp, PhD, from Edanz Group (www.edanzediting.com/ac) for editing a draft of this manuscript.
References
1. Chen CJ, Saulle D, Fu KM, Smith JS, Shaffrey CI. Dysphagia following combined anterior-posterior cervical spine surgeries. J Neurosurg Spine. 2013. 19: 279-87
2. Fehlings MG, Smith JS, Kopjar B, Arnold PM, Yoon ST, Vaccaro AR. Perioperative and delayed complications associated with the surgical treatment of cervical spondylotic myelopathy based on 302 patients from the AOSpine North America cervical spondylotic myelopathy study. Clinical article. J Neurosurg Spine. 2012. 16: 425-32
3. Kaneyama S, Sumi M, Takabatake M, Kasahara K, Kanemura A, Hirata H. The prediction and prevention of dysphagia after occipitospinal fusion by use of the S-line (swallowing line). Spine (Phila Pa 1976). 2017. 42: 718-25
4. McCafferty RR, Harrison MJ, Tamas LB, Larkins MV. Ossification of the anterior longitudinal ligament and forestier’s disease: An analysis of seven cases. J Neurosurg. 1995. 83: 13-7
5. Radcliff KE, Koyonos L, Clyde C, Sidhu GS, Fickes M, Hilibrand AS. What is the incidence of dysphagia after posterior cervical surgery?. Spine. 2013. 38: 1082-8
6. Smith-Hammond CA, New KC, Pietrobon R, Curtis DJ, Scharver CH, Turner DA. Prospective analysis of incidence and risk factors of dysphagia in spine surgery patients: Comparison of anterior cervical, posterior cervical, and lumbar procedures. Spine (Phila Pa 1976). 2004. 29: 1441-6
7. Tian W, Yu J. The role of C2-C7 and O-C2 angle in the development of dysphagia after cervical spine surgery. Dysphagia. 2013. 28: 131-8
8. Wang LN, Hu BW, Song YM, Liu LM, Zhou CG, Wang L. Predictive abilities of O-C2a and O-EAa for the development of postoperative dysphagia in patients undergoing occipitocervical fusion. Spine J. 2019. p.