- Department of Neurosurgery, Kurashiki Central Hospital, Kurashiki, Japan.
Correspondence Address:
Ryosuke Kaneko, Department of Neurosurgery, Kurashiki Central Hospital, Kurashiki, Japan.
DOI:10.25259/SNI_1203_2021
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ryosuke Kaneko, Hiroyuki Ikeda, Minami Uezato, Masaki Chin. Removal of a central venous catheter penetrating the vertebral artery: A case report on endovascular treatment for blunt cerebrovascular injury. 11-Mar-2022;13:84
How to cite this URL: Ryosuke Kaneko, Hiroyuki Ikeda, Minami Uezato, Masaki Chin. Removal of a central venous catheter penetrating the vertebral artery: A case report on endovascular treatment for blunt cerebrovascular injury. 11-Mar-2022;13:84. Available from: https://surgicalneurologyint.com/surgicalint-articles/11438/
Abstract
Background: Anticoagulation and endovascular therapy are commonly used treatment methods for blunt cerebrovascular injury (BCVI). However, in certain cases, the perforating objects damaging the blood vessels need to be removed. In such cases, stenting and coil embolization have been reported to be useful. Furthermore, we believe that distal embolization can arrest bleeding at the perforation site when using such treatments. In support of this procedure, we report a case of successful BCVI treatment using distal embolization through contralateral side and proximal protection.
Case Description: A 61-year-old man had an accidental placement of a central venous catheter that resulted in the perforation of the vertebral artery. Endovascular treatment was performed to remove the catheter and prevent bleeding during extraction. For this treatment, we used the method of distal embolization through the contralateral approach and proximal protection with a microballoon catheter followed by removal of the perforating catheter and additional embolization of the bleeding point under controlled blood flow.
Conclusion: Under distal and proximal protections, we were able to successfully remove the perforating catheter without bleeding and ischemic complications. While treating BCVI, which requires the removal of perforating material, attention should be paid to the various protection methods and procedures.
Keywords: Blunt cerebrovascular injury, Central venous catheterization, Endovascular treatment, Vertebral artery injury
INTRODUCTION
Blunt cerebrovascular injury (BCVI) is a trauma associated with stroke.[
CASE DESCRIPTION
A 61-year-old man with pneumonia underwent intubation and placement of a CVC with an outer diameter of 2.5 mm. The intended catheter, inserted into the left internal jugular vein, inadvertently entered the left vertebral artery (V1 segment), with its tip entering the aortic arch through the subclavian artery. Contrast-enhanced computed tomography (CT) revealed that the catheter was not inserted into the internal jugular vein but was incorrectly inserted into the left vertebral artery and caused occlusion of the left vertebral artery [
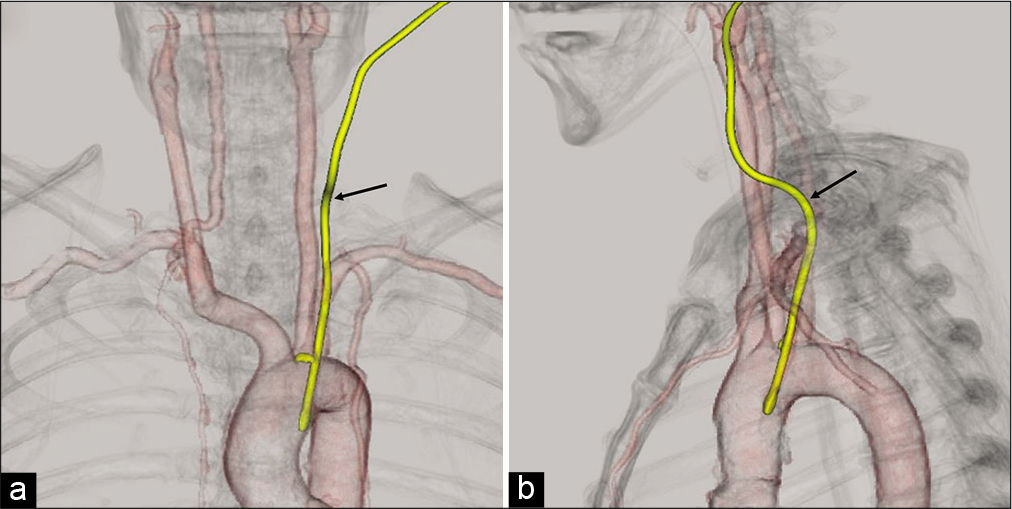
Figure 1:
Preoperative contrast-enhanced computed tomography findings. The yellow line indicates a catheter that was inserted incorrectly, and the arrow indicates the entry site. The catheter tip can be seen reaching the aortic arch. The left vertebral artery was occluded. (a) Frontal view, (b) lateral view.
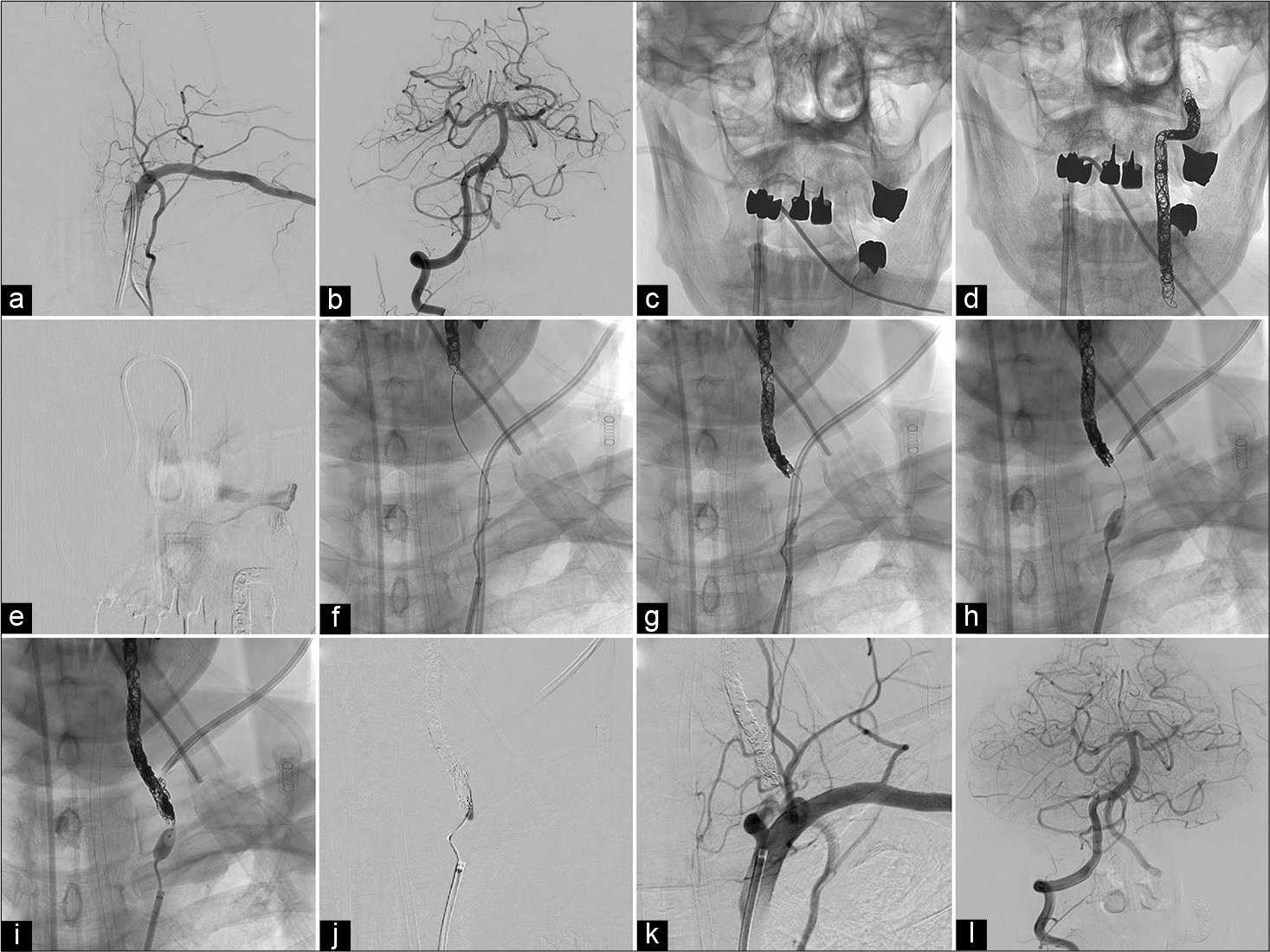
Figure 2:
Pre- and intra-operative angiography. (a) Preoperative left subclavian artery angiography shows occlusion of the main trunk of the left vertebral artery and collateral blood flow in the left V3 segment. (b) Preoperative right vertebral artery angiography shows that the left vertebral artery is retrograde to the V4 segment, and the left posterior inferior cerebellar artery territory shows bilateral dominance. (c) Retrograde approach from the contralateral side. SL-10 was guided to the left vertebral artery through union using TACTICS as a distal access catheter. (d) V2 to V3 segment was embolized by contralateral approach. (e) After embolization of the V2 to V3 segment of the left vertebral artery, subclavian arteriography showed preserved collateral blood flow in the V3 segment. (f) Proximal approach to the affected side. The presence of the distal coil allowed the passage of the perforator site with the Carnelian Marvel microcatheter. (g) Under proximal protection with the Pinnacle balloon, coil embolization was performed up to the perforator site. (h) Under proximal protection, the central venous catheter was removed while the Pinnacle balloon was inflated. (i) The proximal part and perforator site were embolized under balloon dilation. (j) Injection of n-butyl-2-cyanoacrylate. (k) After embolization, subclavian arteriography confirmed complete occlusion of the left vertebral artery. (l) Postembolization right vertebral artery angiography showed no avascular area.
To arrest the remaining extravascular flow, n-butyl-2-cyanoacrylate (NBCA) was injected to obtain complete embolization. This procedure was performed under the deflating Pinnacle Blue 27 considering the adhesion of NBCA to the Pinnacle Blue 27 [
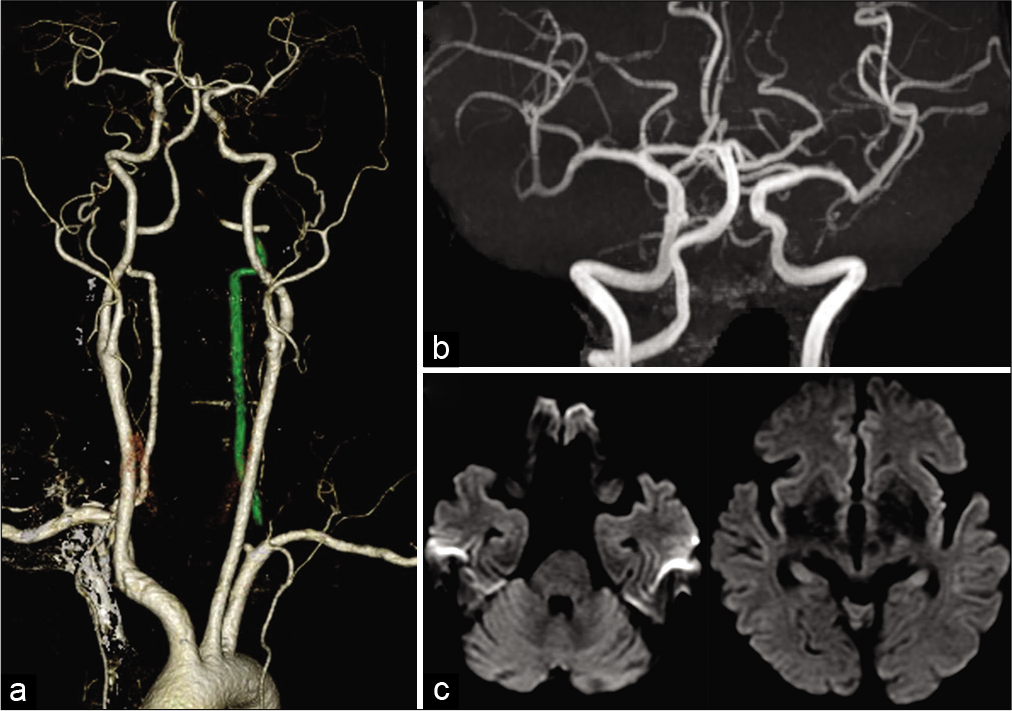
Figure 3:
Postoperative images. (a) Postoperative computed tomography angiography showed complete occlusion of the left vertebral artery. The green line indicates the coil mass. (b) Postoperative magnetic resonance angiography showed occlusion of the left vertebral artery. (c) Postoperative diffusion-weighted image showed no ischemic lesion.
DISCUSSION
Three learning points should be taken from this case. First, the left vertebral artery was occluded. This finding needs to be considered since blood flow to the left vertebral artery was unlikely and thrombus formation occurred in the occlusion site. This indicates a high risk of skipping the clot formed during blood flow resumption following catheter placement in the left vertebral artery and passing through the lesion [
Figure 4:
The schema of strategy. The red lines represent the bilateral vertebral and subclavian artery, and the blue lines represent the catheters that were inserted incorrectly. The catheter entry point corresponds to the point where the blue line extends outside the red line. (a) Assumed condition of the puncture site: we had to assume the presence of a blood clot near the catheter, as shown in the shape outlined in black in the figures. (b) Approaching from the catheter side could have caused distal embolization by thrombus in the direction indicated by an arrow in the figure. In this case, this was because the catheter had to extend beyond the misinsertion point, as shown by the green line. (c) Retrograde embolization for distal embolic protection was performed through the contralateral side. The green line shows the actual part of the microcatheter used for embolization. (d) The green line indicates the catheter passing through the lesion from the proximal side. At this point, the coil is in a position to safely pass the lesion. (e) Coil embolization up to the catheter entry point with the balloon dilated (green). (f) The catheter was not completely removed but has slowly moved to the outside of the vessel (blue), while embolizing the perforation so that it was filled with coils. (g) Completion of embolization while removing the central venous catheter. (h) N-butyl-2-cyanoacrylate injection.
CONCLUSION
We were able to successfully treat a case of BCVI, emphasizing on distal embolization prevention. Considering the limitations discussed in this study, this method may be useful in similar cases of puncture trauma.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Akkan K, Cindil E, Kilic K, Ilgit E, Onal B, Erbas G. Misplaced central venous catheter in the vertebral artery: Endovascular treatment of foreseen hemorrhage during catheter withdrawal. J Vasc Access. 2014. 15: 418-23
2. Al Rayes A, Khattak Y, Qafani A, Anwar M, Al Sibaie A. Acute management of iatrogenic injury to vertebral artery with central venous catheter in a critically ill patient. Cureus. 2020. 12: e9956
3. Burlew CC, Biffl WL, Moore EE, Pieracci FM, Beauchamp KM, Stovall R. Endovascular stenting is rarely necessary for the management of blunt cerebrovascular injuries. J Am Coll Surg. 2014. 218: 1012-7
4. Guilbert M, Elkouri S, Bracco D, Corriveau MM, Beaudoin N, Dubois MJ. Arterial trauma during central venous catheter insertion: Case series, review and proposed algorithm. J Vasc Surg. 2008. 48: 918-25
5. Nagpal P, Policeni BA, Bathla G Khandelwal A, Derdeyn C, Skeete D. Blunt Cerebrovascular injuries: Advances in screening, imaging, and management trends. AJNR Am J Neuroradiol. 2017. 39: 406-14
6. Tasopoulou K, Argyriou C, Mantatzis M, Kantartzi K, Passadakis P, Georgiadis GS. Endovascular repair of an inadvertent right vertebral artery rupture during dialysis catheter insertion. Ann Vasc Surg. 2018. 51: 324.e11-6
7. Uchikawa H, Kai Y, Ohmori Y, Kuratsu JI. Strategy for endovascular coil embolization of a penetrating vertebral artery injury. Surg Neurol Int. 2015. 6: 117
8. Yoon DY, Annambhotla S, Resnick SA, Eskandari MK, Rodriguez HE. Inadvertent arterial placement of central venous catheters: Diagnostic and therapeutic strategies. Ann Vasc Surg. 2015. 29: 1567-74