- Clinical Professor of Neurological Surgery, School of Medicine, State Univeristy of NY at Stony Brook, New York, United States.
DOI:10.25259/SNI_555_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Nancy E. Epstein. Reperfusion Injury (RPI)/White Cord Syndrome (WCS) Due to Cervical Spine Surgery: A Diagnosis of Exclusion. 02-Oct-2020;11:320
How to cite this URL: Nancy E. Epstein. Reperfusion Injury (RPI)/White Cord Syndrome (WCS) Due to Cervical Spine Surgery: A Diagnosis of Exclusion. 02-Oct-2020;11:320. Available from: https://surgicalneurologyint.com/surgicalint-articles/10302/
Abstract
Background: Following acute cervical spinal cord decompression, a subset of patients may develop acute postoperative paralysis due to Reperfusion Injury (RPI)/White Cord Syndrome (WCS). Pathophysiologically, this occurs due to the immediate restoration of normal blood flow to previously markedly compressed, and under-perfused/ischemic cord tissues. On emergent postoperative MR scans, the classical findings for RPI/ WCS include new or expanded, and focal or diffuse intramedullary hyperintense cord signals consistent with edema/ischemia, swelling, and/or intrinsic hematoma. To confirm RPI/WCS, MR studies must exclude extrinsic cord pathology (e.g. extramedullary hematomas, new/residual compressive disease, new graft/vertebral fracture etc.) that may warrant additional cervical surgery to avoid permanent neurological sequelae.
Methods: In the English literature (i.e. excluding 2 Japanese studies), 9 patients were identified with postoperative RPI/WCS following cervical surgical procedures. For 7 patients, new acute postoperative neurological deficits were appropriately attributed to MR-documented RPI/WCS syndromes (i.e. hyperintense cord signals). However, for 2 patients who neurologically worsened, MR studies demonstrated residual extrinsic disease (e.g. stenosis and OPLL) warranting additional surgery; therefore, these 2 patients did not meet the criteria for RPI/WCS.
Results: The diagnosis of RPI/WCS is one of exclusion. It is critical to rule out residual extrinsic cord compression where secondary surgery may improve/resolve neurological deficits.
Conclusions: Patients with acute postoperative neurological deficits following cervical spine surgery must undergo MR studies to rule out extrinsic cord pathology before being diagnosed with RPI/WCS. Notably, 2 of the 9 cases of RPI/WCS reported in the literature required additional surgery to address stenosis and OPLL, and therefore, did not have the RPI/WCS syndromes.
Keywords: Reperfusion Injury (RPI), White Cord Syndrome (WCS), Diagnosis of Exclusion, Cervical Spine Surgery, Myelopathy, Quadriplegia Cord Injury, Residual Cord Compression
INTRODUCTION
Definition, Pathophysiology, and Etiology of Reperfusion Injury (RPI)/White Cord Syndrome (WCS) Following Cervical Spine Surgery
RPI/WCS is typically defined as an acute spinal cord injury that follows cervical spine surgery where postoperative MR studies document intrinsic cord edema/ischemia, swelling, and/or hemorrhage in the absence of significant new/residual extrinsic pathology. Pathophysiologically, this occurs because spinal cord decompression due to cervical surgery acutely restores normal blood flow to previously under-perfused/ischemic cervical spinal cord tissues.[
RPI/WCS A Diagnosis of Exclusion: Classical Postoperative MR Findings for RPI/WCS
RPI/WCS is a diagnosis of exclusion following multiple cervical surgical procedures; anterior cervical discectomy/fusion (ACDF), anterior corpectomy/fusion (ACF), laminectomy with/without fusion, laminoplasty, or other cervical procedures including those for tumor resection. Postoperative MR studies best document the classical intrinsic cord changes diagnostic for RPI/WCS.[
Frequency of Reperfusion Injury (RPI)/White Cord Syndrome (WCS)
Seichi et al. (2014) Frequency of RPI/WCS Following Laminoplasty
In 2004, Seichi et al. evaluated the frequency of RPI/WCS in 114 patients with severe cervical myelopathy undergoing laminoplasty.[
Frequency of RPI/WCS Best Identified by Seven Cases in the Literature
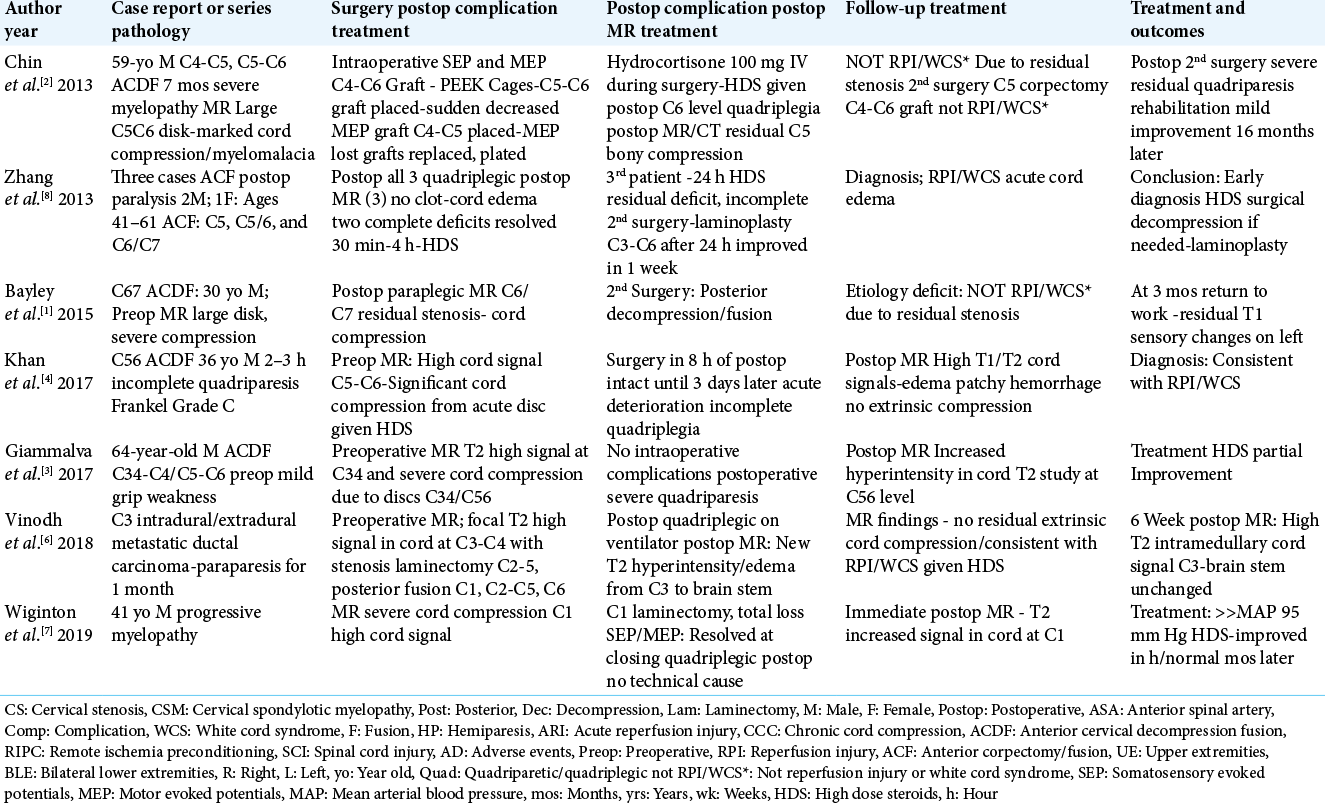
Several authors defined the RPI/WCS syndrome as “rare”, involving only a small number of cases found in the English literature (i.e. omitting Khan et al. 1973 case, and 2 additional Japanese studies) that met the MR-documented inclusion criteria) [Table1].[
Treatment Options for RPI/WCS
Conservative Management
Conservative treatment options for patients with RPI/WCS include; admission to intensive care units for neurological monitoring, elevation of mean arterial pressures (MAP) (i.e. averaging 85-95 mm HG) to perfuse a compromised/ ischemic cord, and the administration of steroids (varying regimens from Decadron to High Dose/Trauma Protocol of Methylprednisolone).
Select Additional Surgical Decompression for RPI/WCS
Zhang et al. offered several explanations as to why RPI/WCS injuries occurred in their 3 OPLL patients [
In one of Zhang et al.’s patients, following a C4-C6 anterior corpectomy/fusion, the patient was immediately quadriplegic. [
Case Summaries
Here, we reviewed each of the 7 patients undergoing 5 anterior and 2 posterior procedures, who developed immediate postoperative MR findings consistent with RPI/ WCS [
Risk of Reperfusion Injury After Posterior Cervical Decompression
Following posterior cervical decompressive surgery, the following two patients developed acute postoperative RPI/ WCS.[
Case #1
In Vinodh et al. (2018), a 51-year-old female presented with 1-month of increasing paraparesis, and urinary dysfunction [
Case #2
A 41-year-old male in the Wiginton et al. study (2019) presented with increasing myelopathy (e.g. 4/5 motor function in the upper and lower extremities accompanied by bilateraal Hoffman’s signs, and diffuse hyperreflexia with clonus) [
Risk of RPI/WCS After Anterior Cervical Surgery
2 Cases of RPI/WCS After Anterior Cervical Diskectomuy and Fusion (ACDF)
In two cases, following ACDF, patients developed RPI/WCS confirmed on postoperative MR studies.
Case #3
In 2017, Kahn et al. evaluated a 36-year-old male who presented with 2 weeks of vague cervicalgia, and the acute onset of an incomplete quadriparesis over just 2-3 hours (e.g. motor deficit 2-3/5 in the upper/lower extremities with incomplete sensory dysfunction: ASIA/Frankel Grade C) [
The patient was placed on the high-dose steroid trauma protocol of Methylprednisolone (30 mg/kg bolus followed by 5.4 mg/kg/ hour over 24 hours), and brought to surgery 8 hours following the onset of symptoms. A C5-C6 ACDF was routinely performed using an iliac autograft with a plate. Notably, at surgery, there was evidence of prior trauma. Immediately postoperatively, the patient’s motor status improved to the 3/5 level in the upper and lower extremities. However, 3 days later, the patient acutely became fully quadriplegic, requiring immediate ventilatory support. Although the cervical X-rays showed the fusion construct was intact, the STAT MR revealed an intramedullary hemorrhagic cord infarction with edema maximal at the C5-C6 level (hyperintense on T1 and T2 weighted signals) without extrinsic cord compresion. The contrast study showed “patchy enhancement with luxury perfusion” in the cord. The patient’s deterioration was attributed to a RPI/WCS injury characterized as a; “…delayed ischemic/reperfusion injury,…(due to) restoration of blood flow through the anterior spinal artery”. Within a year, the patient’s motor function improved to the 4-/5 level in all four extremities. Although he continued to have a relative C4 pin level, he regained vibratory/position appreciation, and no longer required a ventilator.
Case # 4
A 64-year-old male in Giammalva et al. 2017 study underwent a C3-C4 and C5-6 ACDF for severe cervical cord compromise [
2 Cases of ACDF With Residual Extrinsic Cord Compression Requiring Additional Surgery; These Patients Did Not Have the RPI/WCS Syndrome
In two case reports, the diagnosis of RPI/WCS should have been excluded; both patients’ new postoperative deficits following ACDF were due to MR-documented residual extrinsic cord compression requiring secondary surgery (e.g. stenosis and OPLL respectively) [
Case # 5
Bayley et al. (2015) performed a C6-C7 ACDF in a 30-year-old male who presented with left upper extremity paresthesias accompanied by left leg weakness; the MR demonstrated a large C6-C7 disc herniation [
Case # 6
A 59-year-old male in the Chin et al. (2013) study underwent a two-level C4-C5/C5-C6 ACDF [
Reperfusion Injury After Anterior Cervical Corpectomy and Fusion (ACCF)
Three patients in Zhang et al. series, undergoing multilevel anterior corpectomy/fusions for OPLL, exhibited postoperative RPI/WCS [
Summary of 3 OPLL Cases with RPI/WCS with Specific Presentation of Case #7 Who Required an Additional Posterior Decompression
Zhang et al. (2013) reported 3 patients with OPLL, ranging from 41-61 years of age; all 3 developed acute postoperative quadriplegia (e.g. within 30 minutes-4 hours) following anterior cervical corpectomy and fusion procedures (ACCF: C(5), C(5-6), and C(6-7)) [
CONCLUSION
Pathophysiologically, the RPI/WCS occurs following acute cervical spinal cord decompression when normal blood flow is restored to previously under-perfused/ischemic spinal cord tissues. To establish the diagnosis of RPI/WCS, postoperative MR studies must demonstrate new or expanded, focal or diffuse hyperintense cord signals on T2 weighted images indicative of cord edema/swelling with occasional additional intramedullary hemorrhages.
However, RPI/WCS is a diagnosis of exclusion. Postoperative MR studies must rule out new/residual extrinsic causes of cord compression; (e.g. extramedullary hematomas, residual/ new disc/stenosis/OPLL/other, graft and/or vertebral fracture/ dislocation, direct cord injury due to overzealous intraoperative dissection, amongst other factors) to determine if further surgery is warranted.[
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Bayley E, Boszczyk BM, Chee Cheong RS, Srivastava A. Major neurological deficit following anterior cervical decompression and fusion: what is the next step?. Eur Spine J. 2015. 24: 162-7
2. Chin KR, Seale J, Cumming V. White cord syndrome” of acute tetraplegia after anterior cervical decompression and fusion for chronic spinal cord compression: a case report. Case Rep Orthop. 2013. 2013: 697918
3. Giammalva GR, Maugeri R, Graziano F. White cord syndrome after non-contiguous double-level anterior cervical decompression and fusion (ACDF): A “no reflow phenomenon”?. Interdiscip Neurosurg Adv Tech Case Manag. 2017. 7: 47-49
4. Khan MF, Jooma R, Hashmi FA, Raghib MF. Delayed spinal cord infarction following anterior cervical surgical decompression. BMJ Case Reports. 2017. Oct 9: bcr2017219863
5. Seichi A, Takeshita K, Kawaguchi H, Nakajima S, Akune T, Nakamura K. Postoperative Expansion of Intramedullary High-Intensity Areas on T2-weighted Magnetic Resonance Imaging After Cervical Laminoplasty. Spine. 2004. 29: 1478-82
6. Vinodh VP, Rajapathy SK, Sellamuthu P, Kandasamy R. White cord syndrome: A devastating complication of spinal decompression surgery. Surgical Neurol Int. 2018. 9: 136
7. Wiginton JG, Brazdzionis J, Mohrdar C, Sweiss R, Lawandy S. Spinal Cord Reperfusion Injury: Case Report, Review of the Literature, and Future Treatment Strategies, Cureus. 2019. 11: e5279
8. Zhang JD, Xia Q, Ji N, Liu YC, Han Y, Ning SL. Transient paralysis shortly after anterior cervical corpectomy and fusion. Orthop Surg. 2013. 5: 23-8






Ahmed Ashry
Posted October 2, 2020, 5:03 pm
I would like to congratulate Dr. Nancy E. Epstein for her nice article. I wish if the author had included our report “White Cord Syndrome: The Terrible Nightmare” in her work.
https://m.scirp.org/papers/99593