- Craniofacial Unit, Department of Pediatric Neurosurgery, Hôpital Necker-Enfants Malades, Paris, France
- Department of Biochemistry, Hôpital Lariboisière, APHP, Paris, France
Correspondence Address:
Federico Di Rocco
Craniofacial Unit, Department of Pediatric Neurosurgery, Hôpital Necker-Enfants Malades, Paris, France
DOI:10.4103/sni.sni_465_17
Copyright: © 2018 Surgical Neurology International This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.How to cite this article: Federico Di Rocco, Kenichi Usami, Tatiana Protzenko, Corinne Collet, Kim Giraudat, Eric Arnaud. Results and limits of posterior cranial vault expansion by osteotomy and internal distractors. 30-Oct-2018;9:217
How to cite this URL: Federico Di Rocco, Kenichi Usami, Tatiana Protzenko, Corinne Collet, Kim Giraudat, Eric Arnaud. Results and limits of posterior cranial vault expansion by osteotomy and internal distractors. 30-Oct-2018;9:217. Available from: http://surgicalneurologyint.com/surgicalint-articles/9052/
Abstract
Background:Expanding the posterior cranial vault has become a common procedure in the treatment of complex craniosynostosis. Several techniques are available to remodel the posterior vault. Aim of this study was to analyze the posterior vault distraction osteogenesis.
Methods:Between 2011 and 2014, 21 children (12 boys) were operated on for a posterior distraction of the cranial vault. The mean age was 8.6 months (minimum, 3 months; maximum, 15 years). Thirteen patients presented a craniofacial syndrome. Five had already been operated on (two anterior cranial surgery, two suboccipital decompression, and one craniotomy for sagittal synostosis). Raised intracranial pressure (ICP) was present in 6 patients. Seven patients had symptomatic cerebellar tonsils herniation (TH).
Results:In 17 children, 2 lateral distractors were placed, in 3 a 3rd medial distractor was placed, and in 1 child 4 distractors were implanted. Volumetric analysis based on computed tomography showed a mean increase of volume of 13.9% 117 days later. After the distraction, symptoms related to raised ICP or TH were improved in all patients, however, radiologically TH was improved at the last follow-up in 54% of the cases.
Conclusion:Posterior cranial vault distraction is an efficacious technique to enlarge the posterior skull vault and treat increased ICP. Moreover, it appears to be efficacious in treating TH-related symptoms.
Keywords: Chiari, craniosynostosis, outcome, posterior cranial vault, skull remodeling, syndromic craniosynostosis
INTRODUCTION
Distraction osteogenesis of the craniofacial skeleton has several applications in the treatment of craniofacial malformations.[
The use of distraction osteogenesis involving the cranial vault was originally described for the frontal calvarium as part of monobloc advancements.[
The purpose of this study is to review the current surgical technique and results of posterior cranial vault distraction in patients with craniosynostosis.
PATIENTS AND METHODS
Patients
Children submitted to posterior cranial vault expansion with distractors at the Craniofacial Unit, Necker Enfants Malades Hospital, over the period between September 2011 and July 2014, were included.
Surgical technique
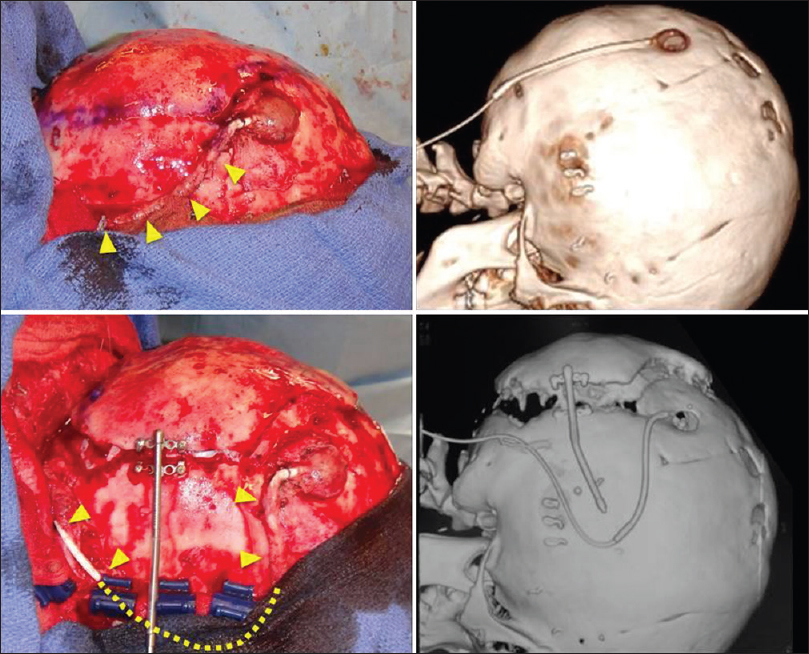
The preoperative preparation, skin incision, and exposure of the skull were performed, as described in the previous article.[
Psychological assessment
The level of anxiety of the parents generated by posterior distraction osteogenesis was also evaluated. Specific questionnaires were designed to measure at different time points of the postoperative period through ordinal scales parental anxiety related to (1) the surgery itself, (2) the use of the distractors and the distraction (the view of the latter, the ability to hold his child in the arms, the pain expressed by the child, etc.), (3) the return home and to school (the care of the scars, the way people look at the child, etc.), and (4) the morphological change (one week after surgery and few weeks after surgery). The questionnaires were given to the parents according to the date of surgery, and the answers were analyzed both quantitatively and qualitatively.
Data analysis
Volumetric analysis
Intracranial volume was calculated from computed tomography (CT) using Volume Viewer 2 medical imaging software (G.E. Healthcare, U.S.A) before and after distraction.
Evaluation of ossification
The degree of ossification of the bone defect on the osteotomy line after cranial vault expansion was evaluated clinically and on the CT performed at the time of removal of distractors. We divided the circle of the osteotomy defect into 10 parts. When more than half of one part was filled by new bone, we considered it as ossified. Therefore, the degree of ossification was counted by 10%, ranging from 0 to 100 percent.[
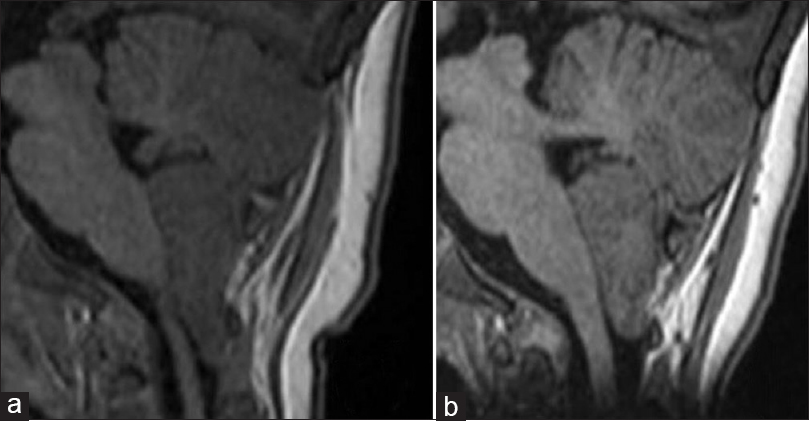
Evaluation of tonsillar herniation
Cerebellar tonsillar herniation (TH) was evaluated in all patients according to sagittal MRI images or reconstructed CT. Patients were diagnosed as TH when cerebellar TH was more than 5 mm through the foramen magnum. Clinical symptoms before and after distraction and at the latest follow-up were noted.
Group classification
Patients were classified according to their underlying syndrome and genetic condition. They were divided into three groups as follows – (1) Group “CAP,” patients with Crouzon syndrome, Apert syndrome, and Pfeiffer syndrome. (2) Group “Other syndromes,” patients with Saethre–Chötzen syndrome, Muenke syndrome, and craniofrontal nasal dysplasia (CFND). (3) Group “complex,” patients without any genetic mutation in FGFRs, TWIST, or EFBN1.
RESULTS
Patient population
A posterior vault distraction was originally intended in 22 cases. However, in a child with a FGFR3-related Crouzon with acanthosis nigricans, because of a severe bleeding from emissary veins during the osteotomy, distractors were not inserted. This child was not included in the analysis. Thus, posterior distractors were implanted in a total of 21 patients.
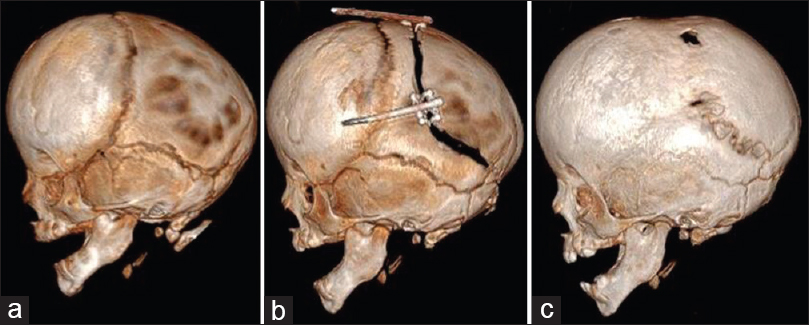
Twelve of the patients were boys and 9 were girls. Signs of raised intracranial pressure were present in 6 patients. Distribution of age at surgery was from 3 months to 15 years; median age was 8.6 months. Two patients had a previous anterior craniotomy, 2 had suboccipital decompression for Chiari malformation, 1 had craniotomy for sagittal synostosis, and 16 patients had no previous craniotomy. Concerning the group 1, there were 7 patients (4 Crouzon, 2 Pfeiffer, and 1 Apert, syndrome), in group 2, 6 patients (3 Saethre-Chötzen syndrome, 2 Muenke syndrome, and 1 CFND), and in group 3, 8 patients. One patient of group “CAP” had a VP shunt implanted 12 years before occipital distraction that needed to be rerouted during surgery [
Surgical procedure and complications
Thirteen of the 21 patients underwent supratorcular craniotomy and 8 infratorcular. The number of distractors was 2 in 17 patients, 3 in 3 patients, and 4 in 1 patient. One patient needed re-installation of distractors in the right side because of distractor malfunction. One patient needed to resuture the surgical wound 3 days after the ablation of distractors because of wound disruption. One patient had pneumonia postoperatively.
Distraction
Distraction started 3 days after implantation, 0.5–1.0 mm a day for 10–15 days. Mean duration between installation and ablation of distractors was 107 ± 32 days. Duration between installation of distractors and the CT evaluation was 117 ± 58 days.
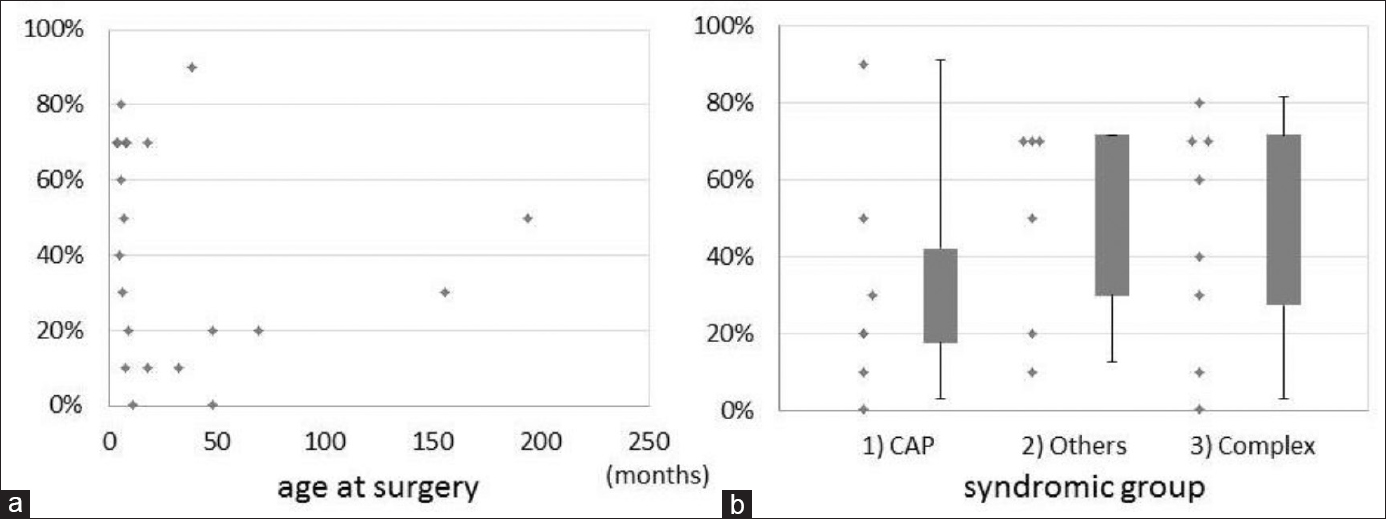
Intracranial volume [ Figure 2 ]
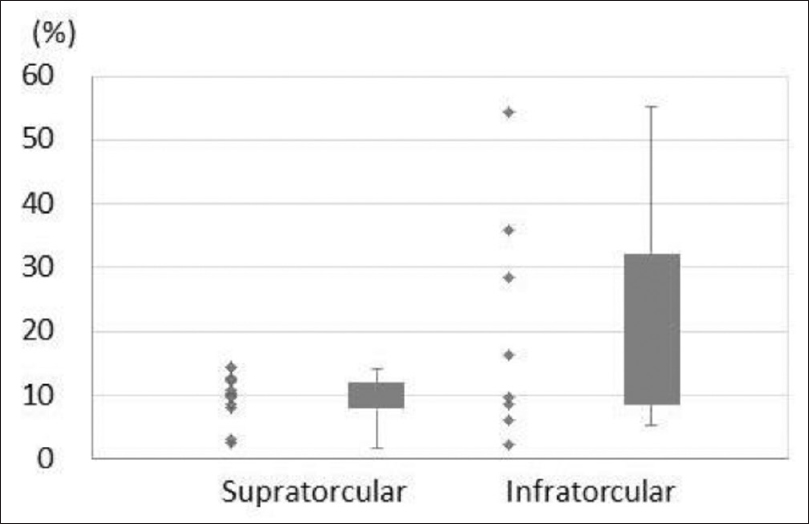
The increase in intracranial volume was 132 ± 86 cc after distraction. The percentage of increase was 13.9 ± 11.9%. The earlier the surgery was performed, the more the intracranial volume augmented. According to symptomatic groups, median value of augmentation was 9.8% in the group “CAP,” 9.1% in the group “Others,” and 13.5% in the group “complex.” There were no significant differences among these groups. Between supratorcular and infratorcular craniotomy, there was no significant difference but there was a tendency of better expansion in infratorcular craniotomy [
Ossification
An accurate evaluation of ossification could not be done clinically. However, CT scan analysis allowed us to precisely divide patients into four groups as follows – “absent,” 8 patients (0–25% ossification), “poor” (26–50% ossification) 5 patients, “ fair” (51–75% ossification) 5 patients, and “good” (76–100% ossification) 2 patients. The age at installation of distractors was 30.2 months in the group “absent,” 73.3 months in “poor,” 7.7 months in “fair,” and 21.8 in “good.” As expected, there was a tendency to ossify more in longer duration from installation of distractors to CT evaluation. However, surprisingly, there was no significant correlation between ossification and age at distraction [
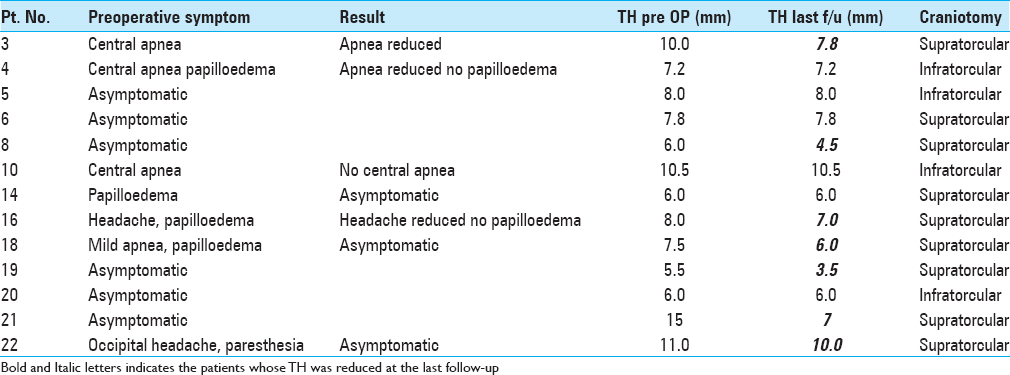
Evolution of tonsillar herniation
Thirteen of 21 patients were diagnosed as TH preoperatively. Two of 13 patients with TH had already undergone posterior decompression prior to distraction, but in 1 of 2 patients, the symptom had recurred. Seven patients had some symptoms preoperatively as follows – sleep apnea in 4, headache in 2, papilloedema in 4, and paresthesia in 1. The average value of TH was 8.3 mm before distraction and 8.1 mm at first control after distraction [
Psychological assessment
Eighteen parents agreed to answer the questionnaires. All parents, as expected, feared the surgical operation, the distraction, and their return home with the child having the distractors implanted. All parents were pleased to see that the children did not suffer during distraction. At first, they were all surprised by the aspect of the distractors on the head of their children and they needed some time to get used to them. One-third were in the beginning uncomfortable in handling their child, but they were finally at ease with the distractors in a few days. All parents could appreciate the morphological change induced by the distraction osteogenesis, and the return home and to school went well in all cases.
The concerns reported by some of the parents were mainly due to their feeling of lack of information concerning the distraction devices; only one-third of the parents felt completely satisfied with the information given ahead of surgery. Few parents reported that they would have liked to have had further details on the characteristics of the distractors, to know the recommended sleeping positions, and to know children's reactions to distractors.
DISCUSSION
Expansion of the posterior cranial vault was suggested to adequately increase the intracranial volume, avoid intracranial hypertension, and at the same time redirect the cerebral expansion posteriorly to prevent turricephaly.[
Initially practiced techniques for posterior cranial vault expansion were formal cranioplasty, with rearrangement and fixation of bone segments, either in the posterior aspect of the skull alone or as part of a combined anterior and posterior cranial vault expansion.[
Several techniques are available nowadays including[
The use of distraction osteogenesis involving the cranial vault was first described for the monobloc advancements,[
White et al. first described posterior cranial expansion with internal distractors in 2009.[
Compared to springs, internal distractors share some risks of device-related complications:[
Compared to translambdoid springs the distractor techniques allow obtaining a good control of the vectors depending on their placement and design of the craniotomy. The design of the craniotomy will decide the size of the bone flap and consequently affect the gain in intracranial volume as well as the change in posterior cranial shape. As for springs, there is a risk of hardware dislocation or dysfunction. Such complication occurred in one of our children leading to reoperation.
Though in the original description of this procedure the horizontal craniotomy was placed below the level of the torcula,[
The number of distractors used for posterior cranial vault expansion has varied from 2 to 4.[
Cerebral tonsils’ prolapse and posterior fossa crowding
Posterior cranial vault expansion has the potential to relieve any local compression on the brain in the posterior cranial fossa. In patients with progressive hydrocephalus, decompression of the subtentorial compartment should theoretically enhance CSF flow in the compressed cerebral aqueduct. Cinalli et al. reported that, in their experience, occipital remodelling and suboccipital decompression may fail to sufficiently restore normal CSF circulation.[
Indications and timing
Posterior cranial vault expansion is indicated in infants with syndromic and nonsyndromic craniosynostosis with a posterior flatness of the skull. In fact, though the posterior cranial flatness is usually less severe in nonsyndromic patients compared to complex multiple suture synostosis, bicoronal synostosis is still associated with an increased risk for raised intracranial pressure.[
The procedure should be done early enough to prevent negative effects on brain development and further progression towards brachy-turricephaly. In most cases, a correction of the frontal region will be needed at a later stage.
Conversely, posterior expansion can also be used in old children, already operated on for the frontal region, who present with recurrent raised ICP or symptoms related to the posterior fossa crowding and descent of cerebellar tonsils. Because of the age of the patient and the limited effect that could be anticipated, we used internal distractors in old children. Though translambdoid springs are not used in our institution in children over 18 months, we can assume, by extrapolation of the volumetric effect according to age, that such springs cannot achieve an increase in volume as important as internal distractors. With this latter technique, we could obtain a resolution of the symptomatology (either raised ICP or brainstem compression) in all children of our series independent of age.
CONCLUSION
Surgical procedures aiming to expand the posterior cranial vault may be considered both in nonsyndromic and syndromic forms of bicoronal synostosis. Posterior cranial vault expansion offers large increase in intracranial volume, which may be needed to prevent intracranial hypertension in such patients. Further, by expanding the posterior cranial vault, local compression of the brain in the posterior cranial fossa may be relieved and progression of cranial dysmorphology towards turricephaly may be prevented. Moreover, an effect on the prolapse of the tonsils can be observed in some patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Arnaud E, Di Rocco F. Faciocraniosynostosis: Monobloc frontofacial osteotomy replacing the two-stage strategy?. Childs Nerv Syst. 2012. 28: 1557-64
2. Choi JW, Ra YS, Hong SH, Kim H, Shin HW, Chung IW. Use of distraction osteogenesis to change endocranial morphology in unilateral coronal craniosynostosis patients. Plast Reconstr Surg. 2010. 126: 995-1004
3. Cinalli G, Chumas P, Arnaud E, Sainte-Rose C, Renier D. Occipital remodeling and suboccipital decompression in severe craniosynostosis associated with tonsillar herniation. Neurosurgery. 1998. 42: 66-
4. Cohen SR, Boydston W, Hudgins R, Burstein FD. Monobloc and facial bipartition distraction with internal devices. J Craniofac Surg. 1999. 10: 244-51
5. Davis C, MacFarlane MR, Wickremesekera A. Occipital expansion without osteotomies in Apert syndrome. Childs Nerv Syst. 2010. 26: 1543-8
6. Ilizarov GA. Clinical application of the tension-stress effect for limb lengthening. Clin Orthop Relat Res. 1990. p. 8-26
7. Levitt MR, Niazi TN, Hopper RA, Ellenbogen RG, Ojemann JG. Resolution of syndromic craniosynostosis-associated Chiari malformation Type I without suboccipital decompression after posterior cranial vault release. J Neurosurg Pediatr. 2012. 9: 111-5
8. McCarthy JG, Schreiber J, Karp N, Thorne CH, Grayson BH. Lengthening the human mandible by gradual distraction. Plast Reconstr Surg. 1992. 89: 1-
9. Mofid MM, Manson PN, Robertson BC, Tufaro AP, Elias JJ, Vander Kolk CA. Craniofacial distraction osteogenesis: A review of 3278 cases. Plast Reconstr Surg. 2001. 108: 1103-
10. Nowinski D, Di Rocco F, Renier D, SainteRose C, Leikola J, Arnaud E. Posterior cranial vault expansion in the treatment of craniosynostosis. Comparison of current techniques. Childs Nerv Syst. 2012. 28: 1537-44
11. Nowinski D, Saiepour D, Leikola J, Messo E, Nilsson P, Enblad P. Posterior cranial vault expansion performed with rapid distraction and time-reduced consolidation in infants with syndromic craniosynostosis. Childs Nerv Syst. 2011. 27: 1999-2003
12. Oyama A, Arnaud E, Marchac D, Renier D. Reossification of cranium and zygomatic arch after monobloc frontofacial distraction advancement for syndromic craniosynostosis. J Craniofac Surg. 2009. 20: 1905-9
13. Persing JA, Jane JA, Delashaw JB. Treatment of bilateral coronal synostosis in infancy: A holistic approach. J Neurosurg. 1990. 72: 171-5
14. Pollack IF, Losken HW, Hurwitz DJ. A combined frontoorbital and occipital advancement technique for use in total calvarial reconstruction. J Neurosurg. 1996. 84: 424-9
15. Renier D, Lajeunie E, Arnaud E, Marchac D. Management of craniosynostoses. Childs Nerv Syst. 2000. 16: 645-58
16. Serlo WS, Ylikontiola LP, Lahdesluoma N, Lappalainen OP, Korpi J, Verkasalo J. Posterior cranial vault distraction osteogenesis in craniosynostosis: Estimated increases in intracranial volume. Childs Nerv Syst. 2011. 27: 627-33
17. Sgouros S, Goldin JH, Hockley AD, Wake MJ. Posterior skull surgery in craniosynostosis. Childs Nerv Syst. 1996. 12: 727-33
18. Shetye PR, Davidson EH, Sorkin M, Grayson BH, McCarthy JG. Evaluation of three surgical techniques for advancement of the midface in growing children with syndromic craniosynostosis. Plast Reconstr Surg. 2010. 126: 982-94
19. Steinbacher DM, Skirpan J, Puchala J, Bartlett SP. Expansion of the posterior cranial vault using distraction osteogenesis. Plast Reconstr Surg. 2011. 127: 792-801
20. Strahle J, Muraszko KM, Buchman SR, Kapurch J, Garton HJ, Maher CO. Chiari malformation associated with craniosynostosis. Neurosurg Focus. 2011. 31: E2-
21. White N, Evans M, Dover MS, Noons P, Solanki G, Nishikawa H. Posterior calvarial vault expansion using distraction osteogenesis. Childs Nerv Syst. 2009. 25: 231-6
22. Yonehara Y, Hirabayashi S, Sugawara Y, Sakurai A, Harii K. Complications associated with gradual cranial vault distraction osteogenesis for the treatment of craniofacial synostosis. J Craniofac Surg. 2003. 14: 526-8
23. Yu JC, Fearon J, Havlik RJ, Buchman SR, Polley JW. Distraction Osteogenesis of the Craniofacial Skeleton. Plast Reconstr Surg. 2004. 114: 1E-20E