- Professor of Clinical Neurosurgery, School of Medicine, State University of NY at Stony Brook and Editor-in-Chief Surgical Neurology International NY, USA, and c/o Dr. Marc Agulnick, 1122 Franklin Avenue Suite 106, Garden City, NY, USA
- Assistant Clinical Professor of Orthopedics, NYU Langone Hospital, Long Island, NY, USA, 1122 Franklin Avenue Suite 106, Garden City, NY, USA
Correspondence Address:
Nancy E. Epstein, M.D., F.A.C.S., Professor of Clinical Neurosurgery, School of Medicine, State University of NY at Stony Brook, and Editor-in-Chief of Surgical Neurology International NY, USA, and c/o Dr. Marc Agulnick, 1122 Franklin Avenue Suite 106, Garden City, NY, USA
DOI:10.25259/SNI_815_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Nancy E. Epstein1, Marc A. Agulnick2. Review/Perspective: Incidence and treatment of CSF leaks/dural tears (DT) occurring during anterior cervical surgery. 01-Nov-2024;15:401
How to cite this URL: Nancy E. Epstein1, Marc A. Agulnick2. Review/Perspective: Incidence and treatment of CSF leaks/dural tears (DT) occurring during anterior cervical surgery. 01-Nov-2024;15:401. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13191
Abstract
Background: The incidence of cerebrospinal fluid (CSF) leaks/dural tears (DT) occurring during anterior cervical diskectomy and fusion (ACDF) are typically relatively low. However, this frequency markedly increases when anterior corpectomy and fusion (ACF) are performed to address ossification of the posterior longitudinal ligament (OPLL).
Methods: The reported frequencies of CSF leaks/DT occurring during elective ACDF (i.e. exclusive of trauma), ranges from 0.24% to 1.7%. Notably, this incidence substantially rises for multilevel ACF addressing anterior OPLL, markedly varying from 3.4 - 44.7%.
Results: The classical risks of anterior cervical CSF leaks/DT with anterior cervical surgery may be minimized utilizing an operating microscope. For OPLL, careful evaluation of preoperative non-contrast CT studies is critical, especially to document whether any of the 3 signs of dural penetrance is present. Here, posterior operative choices should be strongly considered in the presence of sufficient lordosis and/or a Positive K Line (+ K Line) as this will avoid an anterior cervical CSF leak/dural fistula. Alternatively, for patients with kyphosis and a Negative K Line (- K Line), preoperative anticipation and planning to treat an intraoperative anterior CSF leak/DT (i.e. direct anterior primary dural graft repair with 7-0 Gore-Tex sutures, microdural staples, microfibrillar collagen, wound-peritoneal shunt, and lumbar drain or lumboperitneal shunt) are essential in the course of performing direct anterior OPLL resection.
Conclusion: The incidence of anterior cervical CSF leaks/DT is relatively low (i.e. range 0.24 - 1.7%) where ACDF is performed for disc disease/spur/spondylosis exclusive of OPLL. However, where ACF is performed for multilevel OPLL, the risk of CSF Leaks/DT is substantially higher (i.e. range 4.3-44.7%).
Keywords: Anterior Cervical Diskectomy/Fusion (ACDF), Anterior Corpectomy Fusion (ACF), Ossification Posterior Longitudinal Ligament (OPLL), Radiculopathy, Myelopathy, Cervical Cerebrospinal Fluid (CSF) Leaks, Dural Tears (DT), Repair Stragies CSF Fistulas
INTRODUCTION
The frequencies of anterior cervical CSF leaks/dural tears (DT) occurring during anterior cervical surgery vary markedly dependent upon the pathology; relatively low rates are observed for anterior cervical diskectomy/fusion (ACDF)[
Case Summary
A middle-aged patient had previously undergone a C6-C7 ACDF [
Figure 2:
(a) Preoperative Axial and (b) Sagittal MR of the Cervical Spine. The preoperative Cervical Axial (a) and Sagittal (b) MR documented a large central disc herniation at the C56 level above the prior C67 anterior cervical diskectomy and fusion (ACDF). This disc herniation filled over 50% of the ventral spinal canal causing marked cord compression (i.e. as confirmed by the high intramedullary cord signal consistent with edema).
Figure 3:
(a) Postoperative Axial and (b) Sagittal Cervical MR 5 Days Following the C56 ACDF. The initial C56 anterior cervical diskectomy and fusion (ACDF), performed under the microscope, required the removal of a large disc herniation and placement of microfibrillar collagen over a cerebrospinal fluid (CSF) fistula attributed to a traumatic limbus vertebral fracture. (i.e. occurring secondary to the history of trauma). A Polyetheretherketone (PEEK) cage was placed. However, 5 days later, fluid accumulated in the wound, and the follow-up Axial (a) and Sagittal (b) MR scans documented a ventral hyperintense fluid collection consistent with a CSF leak/DT in the anterior epidural disc space. The second surgery, also performed utilizing an operating microscope, included teatment of the anterior CSF leak/DT by direct suturing in an anterior dural graft with 7-0 Gore-Tex Sutures, placement of 1.4 mm microdural staples between the sutures, and the application of microfibrillar collagen.
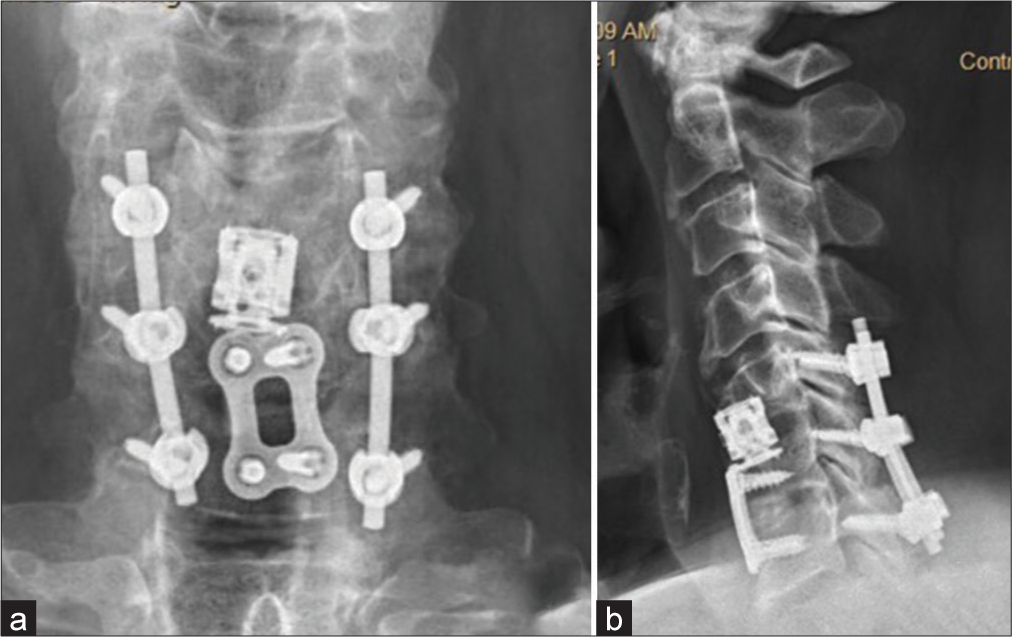
Figure 4:
No Change in the (a) Anteroposterior (AP) and (b) Lateral Cervical X-rays Obtained 2 Months and 2 Years Following the C56 Anterior Cervical Diskectomy and Fusion (ACDF) and Posterior C5-C7 Instrumented Fusion. The AP (a) and Lateral (b) Cervical X-rays obtained 2 months and 2 years following the C56 ACDF and C5-C7 posterior instrumented fusion showed no changes in the location of the anterior (C56 ACDF) or posterior (C5-C7 fusion) instrumentation.
Lessons Learned From This Case
In this patient, who sustained a traumatic cervical disc herniation, the first lesson was that we should have obtained a preoperative cervical CT scan in addition to the MR. This would likely have documented the attendant limbus vertebral fracture responsible for the ventral cerebrospinal fluid (CSF)/DT, enabling the surgeon to better anticipate the need for a complex anterior cervical dural repair. Second, surgery for traumatic cervical disc herniations require not only the routine use of an operating microscope, but also the ready availability of 7-0 Gore-Tex sutures, microdural staples (1.4 mm), and microfibrillar collagen in case a CSF leak is encountered.
Range of Incidence of CSF Leaks For Elective ACDF Surgery
The risk of CSF leaks/DT occurring during ACDF surgery ranges from 0.24-1.7% [
Incidence of Anterior Cervical CSF Leaks/DT for Patients Undergoing ACDF For Trauma
Two studies, one case report and another small case series, discussed performing anterior cervical dural repairs of CSF leaks following traumatic injuries [
Single Case Reports or Small Series of Patients Developing Cervical CSF Leaks/DT Following ACDF Performed in the Absence of Trauma
Single case reports and small series recounted varying rates of CSF leaks/DT occurring following non-traumatic injuries requiring ACDF.[
Large Series Summarizing Risks and Management of CSF Leaks/DT in OPLL Patients
Epstein, in 2014, looked at 3 CT signs of OPLL penetrating the anterior cervical dura [
One Small Case Series and One Case Report on Treatment of CSF Leaks/DT in OPLL Patients Undergoing Anterior Cervical Surgery
One small case series and one case report discussed the presentation/management of CSF leaks/DT occurring due to OPLL and/or other pathologies [
Case Report of Anterior Cervical CSF Leak/DT in OPLL Patient Treated with Contraindicated DuraSeal Resulting in Quadriplegia
Epstein (2021) noted that the package insert for the fibrin sealant DuraSeal (Integra LifeSciences Princeton NJ) states that it’s use is contraindicated for treating anterior cervical CSF fistulas/DT due to the risk of cord swelling/cord compression (i.e. the hydrogel swells 12% “in all directions”) [
CONCLUSION
The incidence of anterior cervical CSF leaks/DT is relatively low (i.e. 0.24% to 1.7%) for ACDF performed to address disc disease/spur/spondylosis exclusive of OPLL [
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Adamson T, Godil SS, Mehrlich M, Mendenhall S, Asher AL, McGirt M. Anterior cervical discectomy and fusion in the outpatient ambulatory surgery setting compared with the inpatient hospital setting: Analysis of 1000 consecutive cases. J Neurosurg Spine. 2016. 24: 878-84
2. Elder BD, Theodros D, Sankey EW, Bydon M, Goodwin CR, Wolinsky JP. Management of cerebrospinal fluid leakage during anterior cervical discectomy and fusion and its effect on spinal fusion. World Neurosurg. 2016. 89: 636-40
3. Epstein NE. Cervical surgery for ossification of the posterior longitudinal ligament: One spine surgeon’s perspective. Surg Neurol Int. 2014. 5: S88-92
4. Epstein NE. A review of complication rates for anterior cervical diskectomy and fusion (ACDF). Surg Neurol Int. 2019. 10: 100
5. Epstein NE, Lancione J. Medicolegal corner (spine): Contraindicated use of DuraSeal in anterior cervical spine led to quadriplegia. Surg Neurol Int. 2021. 12: 532
6. Fengbin Y, Xinyuan L, Ziaowei L, Xinwei W, Deyu C. Management and outcomes of cerebrospinal fluid leak associated with anterior decompression for cervical ossification of the posterior longitudinal ligament with or without dural ossification. Spinal Disord Tech. 2015. 28: 389-93
7. Gazzeri R, Balarza M, Callovini G. Use of tissue sealant patch (TachoSil) in the management of cerebrospinal fluid leaks after anterior cervical spine discectomy and fusion. Br J Neurosurg. 2023. 37: 1406-9
8. Goodwin CR, Boone CE, Pendleton J, Elder BD, Wei Z, Hsu W. Pneumocephalus leading to the diagnosis of cerebrospinal fluid leak and esophageal perforation after cervical spine surgery. J Clin Neurosci. 2016. 26: 141-2
9. Guppy KH, Silverthorn JW. Spinal cord herniation after cervical corpectomy with cerebrospinal fluid leak: Case report and review of the literature. World Neurosurg. 2017. 100: 711.e7-12
10. Halayqeh S, Glueck J, Balmacerno-Criss M, Alsoof D, McDonald CL, Diebo BG. Delayed cerebrospinal fluid (CSF) leak following anterior cervical discectomy and fusion surgery. N Am Spine Soc J. 2023. 16: 100271
11. Jang SW, Lee SH, Shin HK, Jeon SR, Roh SW, Park JH. Management of cerebrospinal fluid leakage by pump-regulated volumetric continuous lumbar drainage following anterior cervical decompression and fusion for ossification of the posterior longitudinal ligament. Neurospine. 2023. 20: 1421-30
12. Kapadia BH, Decker SI, Boylan MR, Shah NV, Paulino CB. Risk factors for cerebrospinal fluid leak following anterior cervical discectomy and fusion. Clin Spine Surg. 2019. 32: E86-90
13. Lee SE, Chung CK, Jahng TA, Kim CH. Dural tear and resultant cerebrospinal fluid leaks after cervical spinal trauma. Eur Spine J. 2014. 23: 1772-6
14. Lei T, Shen Y, Wang LF, Cao JM, Ding WY, Ma QH. Cerebrospinal fluid leakage during anterior approach cervical spine surgery for severe ossification of the posterior longitudinal ligament: Prevention and treatment. Orthop Surg. 2012. 4: 247-52
15. Mazur M, Jost GF, Schmidt MH, Bisson EF. Management of cerebrospinal fluid leaks after anterior decompression for ossification of the posterior longitudinal ligament: A review of the literature. Neurosurg Focus. 2011. 30: E13
16. Mitchell BD, Verla T, Reddy D, Winnegan L, Omeis I. Reliable intraoperative repair nuances of cerebrospinal fluid leak in anterior cervical spine surgery and review of the literature. World Neurosurg. 2016. 88: 252-9
17. Odate S, Shikata J, Soeda T, Yamamura S, Kawagushi S. Surgical results and complications of anterior decompression and fusion as a revision surgery after initial posterior surgery for cervical myelopathy due to ossification of the posterior longitudinal ligament. J Neurosurg Spine. 2017. 26: 466-73
18. Syre P, Bohman LE, Baltuch G, Le Roux P, Welch WC. Cerebrospinal fluid leaks and their management after anterior cervical discectomy and fusion: A report of 13 cases and a review of the literature. Spine (Phila Pa 1976). 2014. 39: E936-43
19. Yoshihara H, Yoneoka D. Incidental dural tear in cervical spine surgery: Analysis of a nationwide database. J Spinal Disord Tech. 2015. 28: 19-24
20. Zhai J, Panchal RP, Tian Y, Wang S, Zhao L. The management of cerebrospinal fluid leak after anterior cervical decompression surgery. Orthopedics. 2018. 41: e283-8