- Center for Cranial Base Surgery, Hospital Angeles Pedregal, Mexico City, Mexico
- Department of Neuropathology, Hospital General de Mexico, Mexico City, Mexico
Correspondence Address:
Agustin Dorantes-Argandar, Center for Cranial Base Surgery, Hospital Angeles Pedregal, Mexico City, Mexico.
DOI:10.25259/SNI_405_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Erik Burgos-Sosa1, Jose de Jesus Julian Mendoza1, Laura Chavez-Macias2, Juan Pablo Ichazo-Castellanos1, Marco Antonio Garfias Rodriguez1, Berenice Garcia-Guzman1, Agustin Dorantes-Argandar1. Rosai-Dorfman sphenoorbital histiocytosis with intraparenchymal invasion: Do we have to consider this skull base pathology as a malignant disease?. 20-Sep-2024;15:337
How to cite this URL: Erik Burgos-Sosa1, Jose de Jesus Julian Mendoza1, Laura Chavez-Macias2, Juan Pablo Ichazo-Castellanos1, Marco Antonio Garfias Rodriguez1, Berenice Garcia-Guzman1, Agustin Dorantes-Argandar1. Rosai-Dorfman sphenoorbital histiocytosis with intraparenchymal invasion: Do we have to consider this skull base pathology as a malignant disease?. 20-Sep-2024;15:337. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13109
Abstract
Background: Rosai-Dorfman disease (RDD) is a rare type of histiocytosis that can manifest with diverse symptoms. It usually presents with systemic involvement, and only a few cases have been reported at the level of the skull base. RDD typically follows a benign course during the progression of the disease. In this particular case reported, after the skull base invasion, the disease started to infiltrate the brain parenchyma. Our objective for this case report was to present this particular progression pattern and the nuances of its surgical treatment. In addition, a revision of the current literature was performed about skull base RDD with intracranial invasion and brain parenchyma infiltration not previously described.
Case Description: We are presenting the case study of a 57-year-old male patient who was experiencing severe headaches and an increase in volume in the right fronto-orbital region. On clinical examination, no neurologic clinical symptoms were observed. Contrast computed tomography and magnetic resonance imaging showed a tumor mass that affected the right orbit, frontal paranasal sinus, greater sphenoid wing, and right frontal lobe with moderate adjacent brain edema. The patient underwent surgery using an extended pterional approach with intracranial, orbital decompression, and frontal sinus cranialization, accompanied by frontal lobe tumor resection. Neuropathologic diagnosis revealed a Rosai-Dorfman histiocytosis disease.
Conclusion: The etiopathogenesis of RDD is still not completely understood. The current literature considers this disease to have a predominantly benign course. Nevertheless, as we have shown in this case, it may, in some cases, present direct parenchymal invasion. We consider that prompt surgical treatment should be ideal to avoid the local and systemic progression of the disease.
Keywords: Histiocytosis, Intraparenchymal invasion, Rosai-Dorfman disease, Skull base, Spheno-orbital
INTRODUCTION
Rosai-Dorfman disease (RDD) is a rare type of benign lymphoproliferative disorder, usually with a self-limiting course. Most cases involve lymph nodes in the cervical region, but it can also affect other areas of the body, representing 25–43% of cases outside of the lymph nodes.[
Scarce literature on this disease has been reported concerning when it starts to compromise brain structures. This case aims to present the development and possible extensions of this type of disease. We describe some intricacies for the appropriate and timely treatment of this skull base lesion to avoid a local progression and intraparenchymal invasion.
LITERATURE REVIEW
We analyzed articles from PubMed from inception to 2024. Search terms included Rosai–Dorfman, orbit, intracranial invasion, surgical resection, skull base, and intraparenchymal invasion. Irrelevant and duplicated articles were removed. Incomplete cases and missing data were excluded from the study. This search yielded 46 articles, representing 67 cases in the skull base. From this, we only included 58 cases. To analyze the invasion of parenchyma from the extension of the skull base, for each case, magnetic resonance imaging (MRI) and surgical reports were visualized and analyzed by the authors. Demographic data and the location of the tumor were collected. Additional information concerning treatment was registered and divided into the type of surgical treatment (biopsy, complete resection, and incomplete/subtotal resection), surgery + radiotherapy, surgery + steroids, and surgery + radiotherapy + steroid treatment. Recurrence was considered if the patient had new clinical symptoms or a new finding was detected on MRI. Statistical analysis for demographic data and recurrence of the disease about the type of surgical treatment was performed using the software Statistical Package for the Social Sciences (version 25.0; IBM Corporation, Armonk, New York, USA).
RESULTS
We found 58 cases with RDD in the skull base area with intracranial invasion with a mean age of 36.74 (±18.073) years, corresponding to 65.5% (n: 38) males and 34.5% (n: 20) females. In order of frequency, the sellar region was the most common affected area (27.6%; n: 16), followed by parasellar/middle fossa (25.9%; n: 15), and suprasellar (22.4%; n: 13). The intraorbital location with skull base involvement was only found in 6.9% (n: 4). In respect to the invasion, we only found a compromise of the cavernous sinus in 13.8% (n: 8).
Surgical treatment and recurrence
In all patients that we analyzed (n: 58), surgical treatment was divided into three modalities: complete resection (32.8%; n: 20), incomplete/subtotal resection (46.6%, n: 27), and biopsy (20.7%; n: 12). Patients received surgical resection without adjuvant therapy in 72.4% (n: 42), surgical resection + radiotherapy in 13.8% (n: 8), surgical treatment + steroids in 6.9% (n: 4), and surgical treatment + radiotherapy + steroids in 6.9% (n: 4).
From the total of cases (n: 58), recurrence was present in 20.7% (n: 12/P: 0.051) in an average follow-up time of 28 months (±26.878). For the patients from which only surgery was considered, recurrence for complete resection (n: 20) was found in 1 patient (5%). For incomplete/subtotal resection (n: 27), recurrence was present in 9 cases (33.3%), and for biopsy (n: 12), recurrence was found in 2 cases (16.7%) [
CASE DESCRIPTION
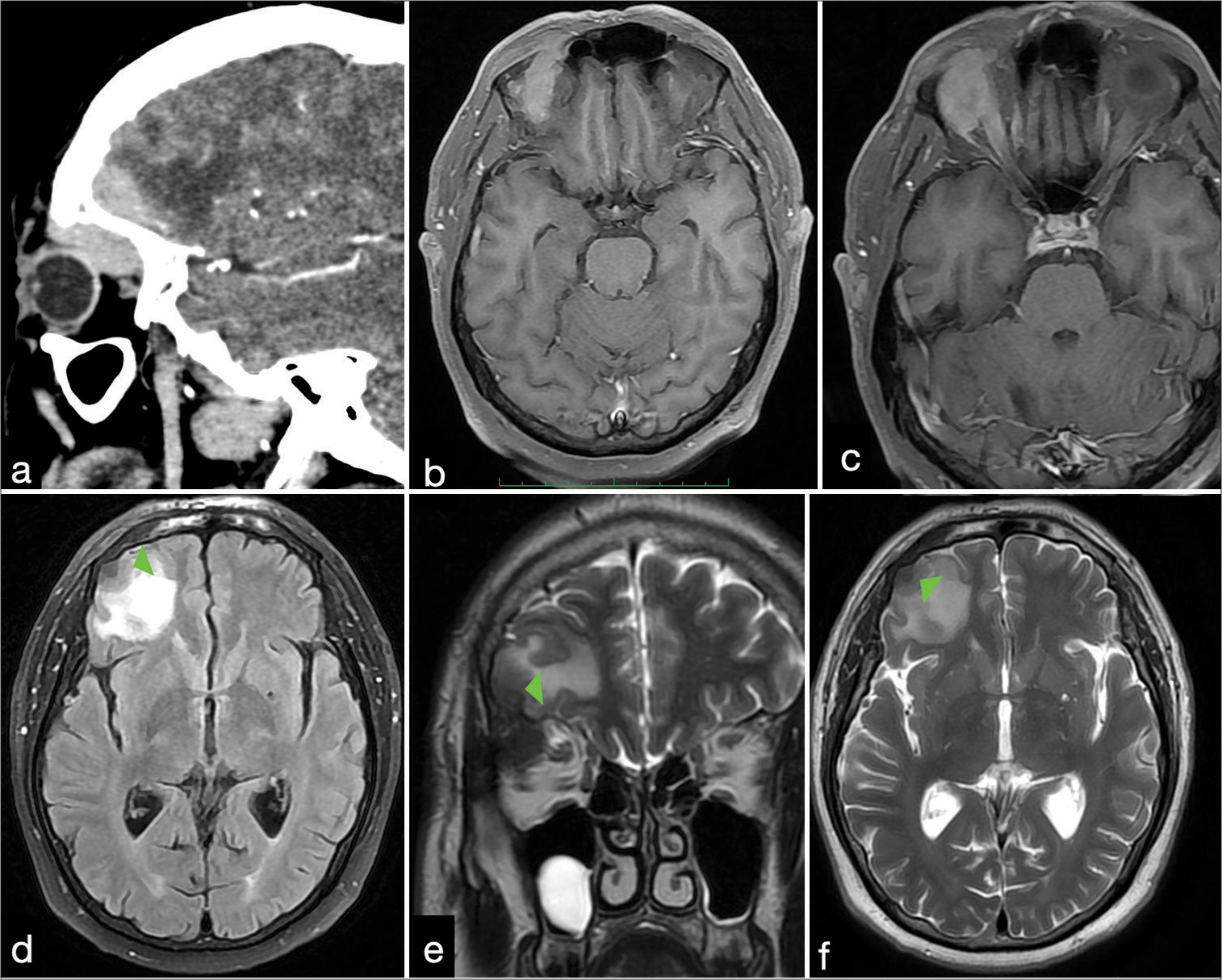
A 57-year-old man presented with persistent headaches and a noticeable increase in volume in the right fronto-orbital region, progressing over the past 3 months. The limitation of the ocular movements accompanied this progression of the disease. Clinical examination reveals only a slight right eye proptosis, with no visual deficit. Computed tomography (CT) and MRI show a solid mass involving the orbit, extending to the skull base, frontal sinus, and greater sphenoid wing with intracranial invasion, infiltration of the inferior frontal gyrus, and moderate brain edema [
Figure 2:
Computed tomography (CT) and magnetic resonance imaging (MRI). (a-c) CT and contrast MRI T1-weighted imaging with contrast shows enhancement of the lesion from the intraorbital area extending to the intracranial compartment with compromise of the frontal sinus. (d) Fluid-attenuated inversion recovery-MRI shows a hyperintense lesion adjacent to the tumor. Green arrowheads indicate the site of infiltration over the parenchyma. (e and f), This last was present on coronal and axial T2-weighted MRI, accompanied by peritumoral hyperintensity suggestive of perilesional edema. Green arrowheads indicate the site of infiltration over the parenchyma.
Surgical resection
An extended pterional approach was performed on the site of the lesion to expose the greater sphenoid wing, roof, and lateral orbital walls.[
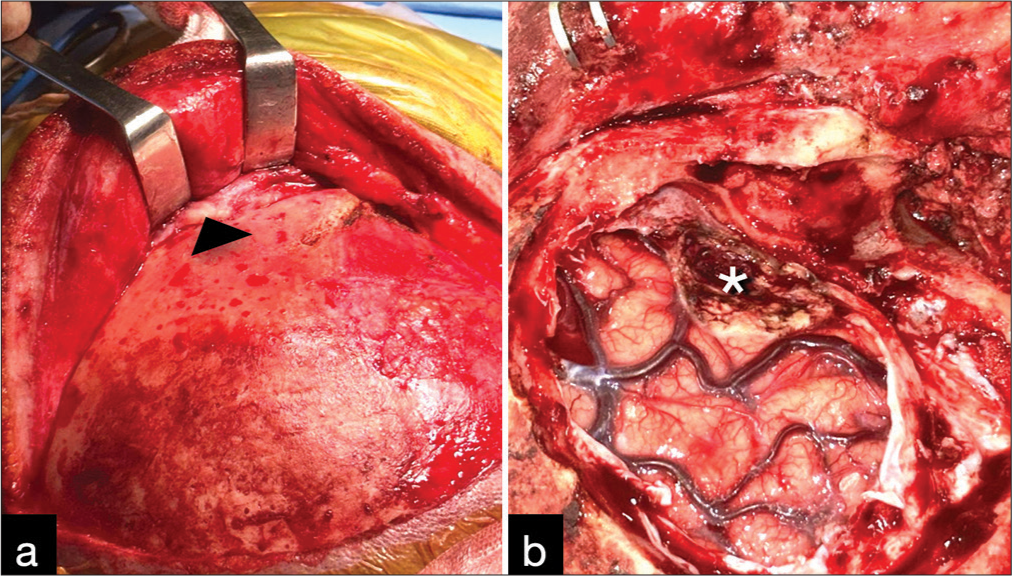
Figure 3:
Surgical resection. (a) Cutaneous flap retraction with superior perirorbital disease involvement. Interfascial dissection was performed to get adequate exposure (the head arrow indicates part of the orbital extension of the tumor). (b) Asterisk shows the resected tumor bed that was infiltrating the inferior frontal gyrus parenchyma.
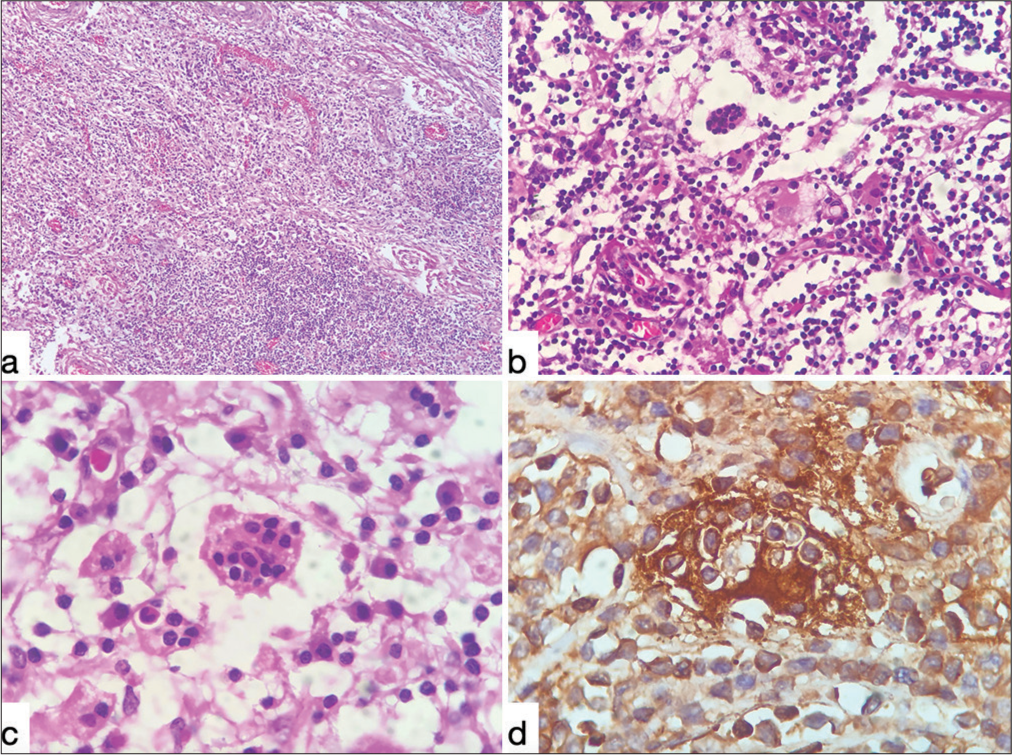
Figure 4
Histopathological findings. (a) Hematoxylin and eosin stain (H.E.). Magnifying glass panoramic photomicrographs recall the appearance of lymph node distribution. Small and large cells with abundant vessels and collagen fibers are noted. (b) (H.E. ×10). Under medium magnification, histiocytic cells with clear or eosinophilic cytoplasm, with some lipids, and a nucleus with moderate pleomorphism can be noted. (c) (H.E. ×40). Here, we can note the phenomenon of emperipolesis or lymphophagocytosis characteristic of this disorder. (d) (Inmunohystoquimic with S100 protein). This photomicrograph demonstrates the positivity of the cells that characterize the disease. (Courtesy from Professor Laura Chavez-Macias, Neuropathologist, Mexico City).
DISCUSSION
In this study, we describe the surgical treatment of a patient who had intracranial fronto-orbital invasive histiocytosis (RDD). Due to its rarity, performing adequate surgical treatment for RDD can be challenging, mainly when it has an involvement of the orbit, skull base, paranasal sinus, and brain parenchyma invasion. To the best of our knowledge, this is the first article that reports and remarks on the potential for brain invasion by this disease.
RDD is commonly regarded as a benign, non-neoplastic, self-limiting, and extracranial histiocytic disease. Its etiology and pathogenesis remain poorly understood.[
After conducting a thorough analysis of the previous reports and their radiologic studies, we found that there were 58 cases of skull base RDD with intracranial extension and only five cases with suggestive brain involvement, even though not specifically commented on in the referenced literature.[
The cause of RDD is still unknown, and while there is more information available, it remains unclear. Various etiologies have been described, including herpesvirus and Epstein– Barr virus;[
The clinical presentation of this disease can belong to several differential diagnoses.[
Intracranial RDD is a rare disease with no established treatment. In some reports, surgery, radiation, and chemotherapy have been effective in reducing neurological deficits.[
The main objective for the treatment of this pathology is to achieve a complete surgical resection, with the main objective to keep the neurovascular structures intact. The extent of resection apparently directly affects the disease progression and the morbidity of the patient.
If complete resection is not an option, adjuvant chemotherapy or radiotherapy may assist in the treatment of the disease.[
Further research is necessary to gain a better understanding of the disease and lead to the development of more effective treatments to treat the disease opportunely without allowing it to cause damage to the brain tissue.
CONCLUSION
The cause of intracranial RDD is still not well understood. It is always important to treat this disease promptly to avoid its progression into brain parenchyma invasion. Complete surgical removal is the preferred treatment due to a lower recurrence rate, and its success depends on the extent of invasion and the surgeon’s experience. For subtotal resection, radiotherapy or steroids may be considered as an adjuvant therapy.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Al-Maghrabi B, Elnaggar T, Alamri O, Al-Maghrabi J. Orbital Rosai-Dorfman disease: A case report and literature review. J Microsc Ultrastruct. 2019. 7: 50-2
2. Andriko JA, Morrison A, Colegial CH, Davis BJ, Jones RV. Rosai-Dorfman disease isolated to the central nervous system: A report of 11 cases. Mod Pathol. 2001. 14: 172-8
3. Basma J, Moore KA, Krisht K, Abuelem T, Arnautovic K, Michael LM. Morphometric comparison of the pterional trans-sylvian and the pretemporal trans-clinoidal approaches to the posterior communicating artery. Oper Neurosurg (Hagerstown). 2020. 20: E22-30
4. Bruce-Brand C, Schneider JW, Schubert P. Rosai-Dorfman disease: An overview. J Clin Pathol. 2020. 73: 697-705
5. Cao X, Yao B, Ma J, Li D, Wang L, Zhang J. RosaiDorfman disease in the skull base: A case series study. World Neurosurg. 2023. 173: e351-8
6. El Majdoub F, Brunn A, Berthold F, Sturm V, Maarouf M. Stereotactic interstitial radiosurgery for intracranial RosaiDorfman disease. A novel therapeutic approach. Strahlenther Onkol. 2009. 185: 109-12
7. Elbaz Younes I, Sokol L, Zhang L. Rosai-Dorfman disease between proliferation and neoplasia. Cancers (Basel). 2022. 14: 5271
8. Foucar E, Rosai J, Dorfman R. Sinus histiocytosis with massive lymphadenopathy (Rosai-Dorfman disease): Review of the entity. Semin Diagn Pathol. 1990. 7: 19-73
9. Foucar E, Rosai J, Dorfman RF. The ophthalmologic manifestations of sinus histiocytosis with massive lymphadenopathy. Am J Ophthalmol. 1979. 87: 354-67
10. Griffiths SJ, Tang W, Parameswaran R, Kelsey A, West CG. Isolated intracranial Rosai-Dorfman disease mimicking meningioma in a child. Br J Neurosurg. 2004. 18: 293-7
11. Gupta K, Bagdi N, Sunitha P, Ghosal N. Isolated intracranial Rosai-Dorfman disease mimicking meningioma in a child: A case report and review of the literature. Br J Radiol. 2011. 84: e138-41
12. Hadjipanayis CG, Bejjani G, Wiley C, Hasegawa T, Maddock M, Kondziolka D. Intracranial Rosai-Dorfman disease treated with microsurgical resection and stereotactic radiosurgery. Case report. J Neurosurg. 2003. 98: 165-8
13. Hollon T, Camelo-Piragua SI, McKean EL, Sullivan SE, Garton HJ. Surgical Management of skull base Rosai-Dorfman disease. World Neurosurg. 2016. 87: 661.e5-12
14. Hur K, Liu C, Koempel JA. Paranasal Rosai-Dorfman disease with osseous destruction. Case Rep Otolaryngol. 2017. 2017: 1453097
15. Khan AA, Siraj F, Rai D, Aggarwal S. Rosai-Dorfman disease of the paranasal sinuses and orbit. Hematol Oncol Stem Cell Ther. 2011. 4: 94-6
16. Kunimatsu A, Kunimatsu N. Skull base tumors and tumor-like lesions: A pictorial review. Pol J Radiol. 2017. 82: 398-409
17. McClellan SF, Ainbinder DJ. Orbital Rosai-Dorfman disease: A literature review. Orbit. 2013. 32: 341-6
18. Rosai J, Dorfman RF. Sinus histiocytosis with massive lymphadenopathy. A newly recognized benign clinicopathological entity. Arch Pathol. 1969. 87: 63-70
19. Song SK, Schwartz IS, Strauchen JA, Huang YP, Sachdev V, Daftary DR. Meningeal nodules with features of extranodal sinus histiocytosis with massive lymphadenopathy. Am J Surg Pathol. 1989. 13: 406-12
20. Su X, Zhang L. Orbital Rosai-Dorfman disease: A case report and literature review. J Int Med Res. 2019. 47: 5891-5
21. Wang F, Qiao G, Lou X, Song X, Chen W. Intracranial recurrences of Rosai-Dorfman disease in the sellar region: Two illustrative cases. Acta Neurochir (Wien). 2011. 153: 859-67
22. Yataco-Vicente JA, Araujo-Castillo RV, Lopez Fuentes MH. Orbital presentation of Rosai-Dorfman disease. Arch Soc Esp Oftalmol (Engl Ed). 2018. 93: 515-8
23. Zhang X, Yin W, Guo Y, He Y, Jiang Z, Li Y. RosaiDorfman disease of the central nervous system: A clinical, radiological, and prognostic study of 12 cases. Front Oncol. 2022. 12: 1013419