- Department of Orthopaedics, University of Rochester School of Medicine, Rochester NY, United States
Correspondence Address:
Jefferson Hunter, Department of Orthopaedics, University of Rochester School of Medicine, Rochester NY, United States.
DOI:10.25259/SNI_1017_2024
Copyright: © 2025 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Jefferson Hunter, Gabriel Ramirez, Caroline Thirukumaran, Paul Rubery. Safety and efficacy of cervical foraminotomy versus anterior cervical discectomy and fusion for 1–2 level radiculopathy. 28-Feb-2025;16:77
How to cite this URL: Jefferson Hunter, Gabriel Ramirez, Caroline Thirukumaran, Paul Rubery. Safety and efficacy of cervical foraminotomy versus anterior cervical discectomy and fusion for 1–2 level radiculopathy. 28-Feb-2025;16:77. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13402
Abstract
BackgroundCervical foraminotomy (CF) and anterior cervical discectomy and fusion (ACDF) are both used to treat 1–2 level cervical radiculopathy. We evaluated demographic and Patient-Reported Outcomes Measurement Information System (PROMIS) to match cohorts and compare the safety/efficacy of performing CF versus ACDF for 1–2 level unilateral radiculopathy.
MethodsThis was a retrospective review of 64 patients with similar clinical and radiological data that underwent 1–2 level unilateral CF versus ACDF for cervical radiculopathy. Variables studied included operative revision rates, adverse events, surgical costs, postoperative imaging, PROMIS scores, numeric pain scores, incidence of dysphagia, frequency of vocal cord paralysis, and postoperative neurological status.
ResultsWe found no clinical or radiological differences between patients undergoing ACDF versus CF for unilateral 1–2 level cervical radiculopathy. Surgical differences were observed; ACDF patients demonstrated a 6.25% revision rate versus 0% for CF patients, 40% of ACDF patients reported mild dysphagia versus 0% for CF, 3% undergoing ACDF exhibited vocal cord paralysis versus 0% for CF, and ACDF incurred high implant costs (i.e., $1,836.37 and $2,773.44 for one- and two-level ACDFs) versus 0% for CF warranting no implants.
ConclusionPatients undergoing CF versus ACDF for 1–2 level unilateral cervical radiculopathy required 3.70 fewer postoperative X-rays, 40 min less operative time, and 10.95-h shorter lengths of hospital stay (P
Keywords: Anterior cervical discectomy and fusion, Cervical radiculopathy, Patient reported outcomes, Posterior cervical foraminotomy, Posterior keyhole foraminotomy
INTRODUCTION
Patient-Reported Outcomes Measurement Information System (PROMIS) is a National Institutes of Health (NIH) sponsored tool that utilizes standardized questionnaires to measure patient-based outcomes (i.e., pain, function, and depression).[
MATERIALS AND METHODS
Study design and setting
This is an IRB-approved retrospective cohort study of outcomes for 32 ACDF (CPT 22551) versus 32 CF (CPT 63020) patients matched by demographic and clinical characteristics [2015–2021;
RESULTS
Adverse events
For ACDFs performed over 6.15 years, two patients required revisions (i.e., 1 for pseudoarthrosis and the other for recurrent axial pain), 13 had mild dysphagia, and there was one case of vocal cord paralysis but no infections. A 5.99-year record review following CF showed no patients required operative revisions, and there were no adverse events (i.e., no dysphagia, no vocal cord paralysis, and no infections).
PROMIS evaluations
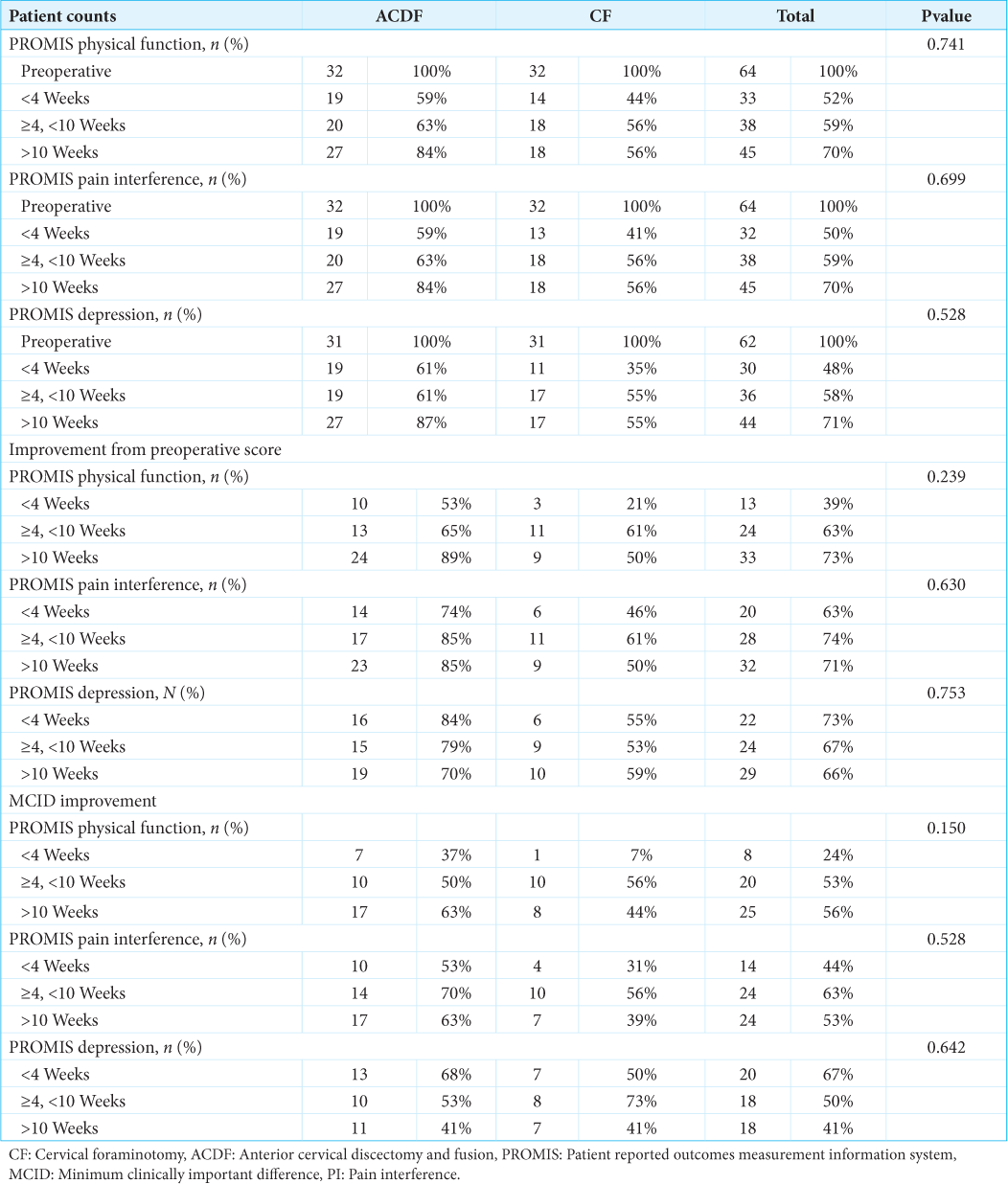
Ten weeks postoperatively, 89%/85% of ACDF and 50%/50% of CF patients reported improvement versus their preoperative PROMIS function/pain status [
Symptom resolution
Sixty-three percentages of ACDF versus 56% of CF patients reported complete pain resolution, 34% versus 47% reported full return of strength, and 47% versus 56% reported resolution of neurological symptoms [
Lower hospital costs, operating room time, and length of stay for CF versus ACDF
The average implant cost for one-level ACDF was $1,836.37, and for two-level ACDF was $2,773.44; CF incurred no implant costs [
Fewer postoperative radiographs for CF versus ACDF patients
CF patients required fewer postoperative cervical radiographs (i.e., average 0.4) versus ACDF patients [i.e., average 4.10;
DISCUSSION
Although ACDF is more commonly performed to treat cervical radiculopathy without myelopathy, CF appears to provide comparable results but with fewer adverse events/morbidity and costs.[
ACDF and CF revision rates range between 5% and 10%[
CONCLUSION
Advantages for CF versus ACDF for one- or two-level unilateral cervical radiculopathy included 3.70 fewer postoperative X-rays, 40 min less operative time, a 10.95-h shorter length of hospital stay, a 0% reoperation rate versus 6.5% for ACDF, no implant costs, no postoperative dysphagia (41% for ACDF), and no vocal cord paralysis (3% for ACDF).
Ethical approval
The research/study was approved by the Institutional Review Board at the University of Rochester research subjects review board (RSRB), number STUDY00000982, approved the study dated March 02, 2023.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Supplementary material available on
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Bydon M, Mathios D, Macki M, de la Garza-Ramos R, Sciubba DM, Witham TF. Long-term patient outcomes after posterior cervical foraminotomy: An analysis of 151 cases. J Neurosurg Spine. 2014. 21: 727-31
2. Fang W, Huang L, Feng F, Yang B, He L, Du G. Anterior cervical discectomy and fusion versus posterior cervical foraminotomy for the treatment of single-level unilateral cervical radiculopathy: A meta-analysis. J Orthop Surg Res. 2020. 15: 202
3. Herkowitz HN, Kurz LT, Overholt DP. Surgical management of cervical soft disc herniation. A comparison between the anterior and posterior approach. Spine (Phila Pa 1976). 1990. 15: 1026-30
4. Hilibrand AS, Robbins M. Adjacent segment degeneration and adjacent segment disease: The consequences of spinal fusion?. Spine J. 2004. 4: 190s-4
5. Jayaram RH, Joo PY, Gouzoulis MJ, Ratnasamy PP, Caruana DL, Grauer JN. Single-level anterior cervical discectomy and fusion results in lower five-year revisions than posterior cervical foraminotomy in a large national cohort. Spine (Phila Pa 1976). 2023. 48: 1266-71
6. Jones RS, Stukenborg GJ. Patient-reported outcomes measurement information system (PROMIS) use in surgical care: A scoping study. J Am Coll Surg. 2017. 224: 245-54.e241
7. Papuga MO, Mesfin A, Molinari R, Rubery PT. Correlation of PROMIS Physical Function and Pain CAT instruments with oswestry disability index and neck disability index in spine patients. Spine (Phila Pa 1976). 2016. 41: 1153-9
8. Purvis TE, Andreou E, Neuman BJ, Riley LH, Skolasky RL. Concurrent validity and responsiveness of PROMIS health domains among patients presenting for anterior cervical spine surgery. Spine (Phila Pa 1976). 2017. 42: E1357-65
9. Sahai N, Changoor S, Dunn CJ, Sinha K, Hwang KS, Faloon M. Minimally invasive posterior cervical foraminotomy as an alternative to anterior cervical discectomy and fusion for unilateral cervical radiculopathy: A systematic review and meta-analysis. Spine (Phila Pa 1976). 2019. 44: 1731-9
10. Simões de Souza NF, Broekema AE, Reneman MF, Koopmans J, van Santbrink H, Arts MP. Posterior cervical foraminotomy compared with anterior cervical discectomy with fusion for cervical radiculopathy: Two-year results of the FACET randomized noninferiority study. J Bone Joint Surg Am. 2024. 106: 1653-63
11. Wang TY, Lubelski D, Abdullah KG, Steinmetz MP, Benzel EC, Mroz TE. Rates of anterior cervical discectomy and fusion after initial posterior cervical foraminotomy. Spine J. 2015. 15: 971-6
12. Witiw CD, Smieliauskas F, O’Toole JE, Fehlings MG, Fessler RG. Comparison of anterior cervical discectomy and fusion to posterior cervical foraminotomy for cervical radiculopathy: Utilization, costs, and adverse events 2003 to 2014. Neurosurgery. 2019. 84: 413-20