- Department of Neurosurgery, University of Kansas Medical Center, Kansas City, Kansas, USA
- Department of Orthopedics, Southwest Hospital, Third Military Medical University, Chongqing, China
Correspondence Address:
Paul M. Arnold
Department of Neurosurgery, University of Kansas Medical Center, Kansas City, Kansas, USA
DOI:10.4103/sni.sni_6_17
Copyright: © 2017 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Chengmin Zhang, Qiang Zhou, Paul M. Arnold. Safety and efficacy of lateral mass screws at C7 in the treatment of cervical degenerative disease. 07-Sep-2017;8:218
How to cite this URL: Chengmin Zhang, Qiang Zhou, Paul M. Arnold. Safety and efficacy of lateral mass screws at C7 in the treatment of cervical degenerative disease. 07-Sep-2017;8:218. Available from: http://surgicalneurologyint.com/surgicalint-articles/safety-and-efficacy-of-lateral-mass-screws-at-c7-in-the-treatment-of-cervical-degenerative-disease/
Abstract
Background:To evaluate the safety and efficacy of lateral mass screws at C7 in the treatment of cervical degenerative disease.
Methods:Patients with cervical degenerative disease who underwent posterior cervical fusion and fixation from 2009 to 2015 were included in the study. All complications were captured. Postoperative X-ray and computed tomography (CT) confirmed fusion at 6 and 12 months after surgery. X-ray and CT confirmed screw loosening, misplacement, pull-out, breakage, or rod breakage.
Results:Seventy-two patients underwent cervical laminectomy and fixation with lateral mass screws at C7 and had at least 1 year follow-up. One patient had C3 screw pull-out; revision was not required. There were no complications related to the C7 screws, and all were in the lateral mass.
Conclusions:Lateral mass screws are as safe and effective as pedicle screws at C7 in long-segment posterior cervical fixation, have a lower rate of perioperative complications than pedicle screws, and are technically easier to place.
Keywords: Cervical spine, lateral mass screw, pedicle screw, posterior fusion, spinal degenerative disease
INTRODUCTION
Posterior cervical procedures are performed for degenerative diseases such as cervical myelopathy, ossification of the posterior longitudinal ligament (OPLL), and multilevel disc herniation. Decompression relieves pressure on the spinal cord and fixation helps maintain cervical alignment and stability. There are several techniques for screw placement in the subaxial cervical spine. Lateral mass screws (LMS) and pedicle screws (PS) are the most commonly used.[
MATERIALS AND METHODS
This was a retrospective study of 72 patients who were followed for 1 year following posterior cervical fusion from January 2009 to August 2015 addressing cervical degenerative disease.
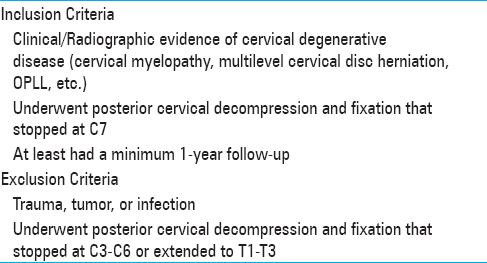
Inclusion/Exclusion criteria
The details of inclusion and exclusion criteria are listed in
Clinical outcomes and radiographic assessment
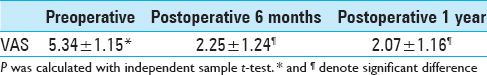
Patients’ clinical outcomes [using visual analog scale (VAS)] and radiographic outcomes [computed tomography (CT), dynamic X-rays] were assessed preoperatively and postoperatively 6 months and 1 year.
Surgery technique
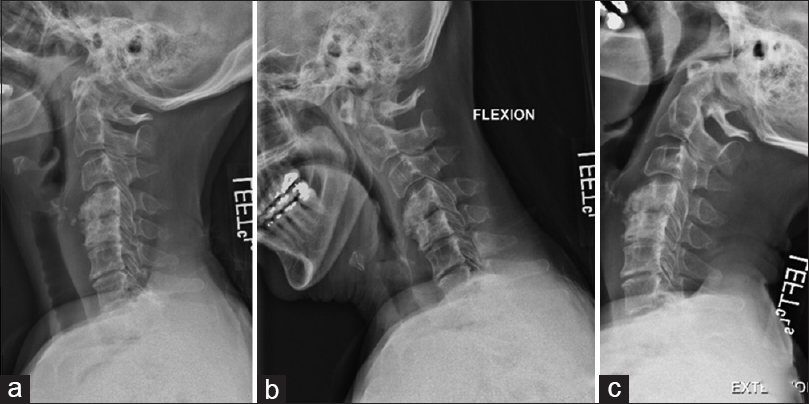
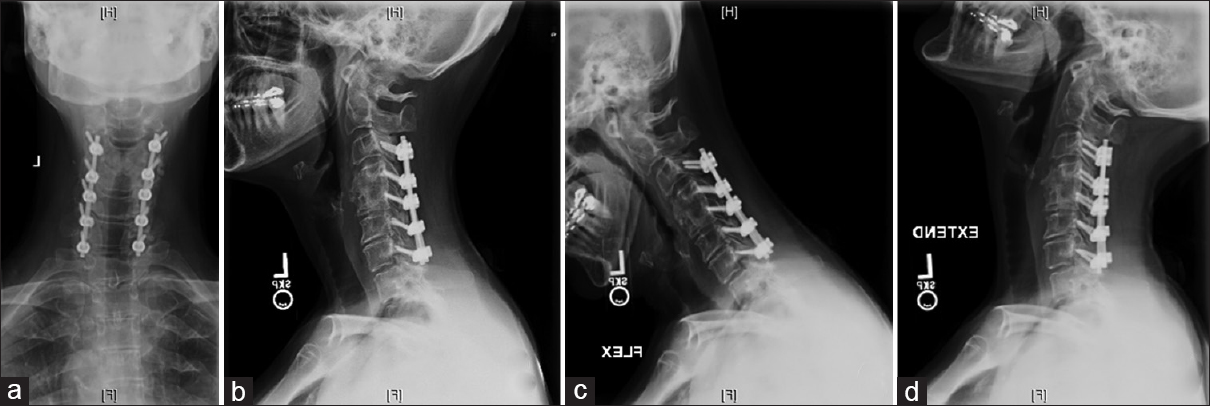
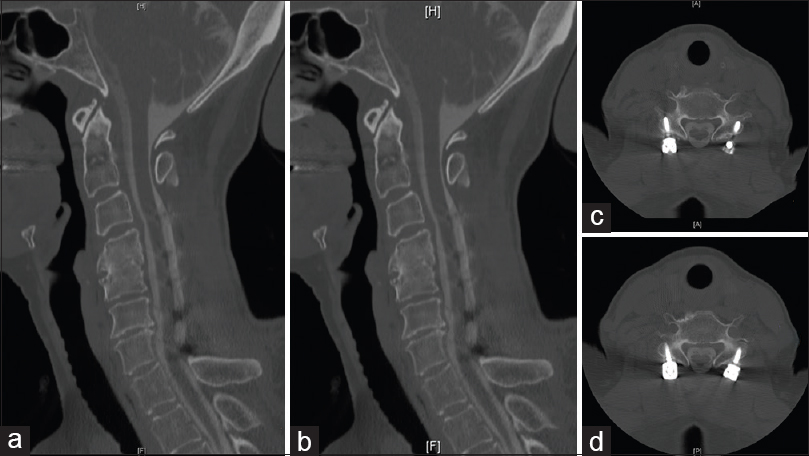
Lateral mass screws were placed bilaterally from C2-C7. They were placed free hand using anatomic landmarks to locate the entry point; intraoperative X-rays were then used to confirm that all screws were placed correctly. Following cervical laminectomies (average 3.5 levels), rods were cut to size and placed bilaterally within the screw heads. Bone from the laminectomy was then used for the fusion [Figures
RESULTS
All 72 patients had at least 1 year follow-up. There were 32 females and 40 males; mean age was 63.7 years. Of the 72 patients, 29 had cervical stenosis, 39 had cervical myelopathy, 3 hadpost-laminectomy kyphosis, and 1 had cervical central cord syndrome. Levels operated were C3–C7 (46 patients), C4–C7 (17), C5–C7 (8), and C2–C7 (1). Follow-up ranged from 12 to 72 months.
Outcomes
Clinical outcomes in all 83 patients were good and all patients reported relief of neck and radiating pain [
Complications
The complication rate was low. There were no neurovascular, spinal central cord, or nerve root injuries in all 72 patients. A cerebrospinal fluid (CSF) leak was reported in 1 patient intraoperatively and the dura was repaired primarily. Screw loosening was confirmed by X-ray and CT at the C3 level in 1 patient during the postoperative period; the patient did not require further surgery. There were no screw-related complications and there were no revision surgeries. Specifically, there was no evidence of neural injury, vascular injury, screw breakage, or screw pull-out related to insertion at the C7 level.
DISCUSSION
Posterior cervical fixation is the standard treatment for this disease. LMS are commonly used in posterior cervical fixation, with good clinical outcomes and low rates of complications. Most surgeons use LMS from C3–C6, but controversy remains regarding the use of LMS and PS at C7. LMS have good clinical outcomes, a low rate of complications, a high rate of fusion, and a low rate of screw loosening and breakage.[
Anatomy of the C7 vertebra
The width of the cervical pedicles decreases significantly from C2 to C7 and the unique anatomy of C7, along with the vertebral artery and nerves around the pedicle, result in technical challenges placing PS at C7. Moreover, the pedicle diameter of C7 is small, so there is a higher risk of nerve and vertebral artery injury during placement of PS at C7. Notably, neurovascular injury is the primary complication with the use of PS, whereas the rate of neurovascular injury is lower with the use of LMS at this level. In addition, if LMS are used at C3–C6 and PS at C7, contouring the rod can be difficult.
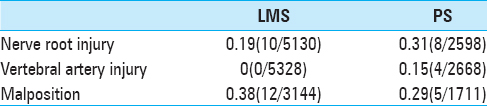
Yoshihara et al.[
Neuronavigation impacts placement of C7 PS
With the development of intraoperative navigation, the accuracy of cervical PS insertion has improved.[
No LMS loosening or pull-out
Most surgeons prefer hybrid screw fixation, using LMS from C3–C6 and PS at C7. Some biomechanical studies[
Late complications of LMS vs. PS
A review regarding late complications of LMS and PS showed no screw loosening,[
In our study, screw pull-out was reported in 1 patient for arate of 1.3%. There were no complications related to the pull-out of C7 screws.
CONCLUSION
Lateral mass screws are as safe and effective as pedicle screws at C7 in long-segment posterior cervical fixation. In addition, lateral mass screws have a lower rate of perioperative complications than pedicle screws and are technically easier to place.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Coe JD, Vaccaro AR, Dailey AT, Skolasky RL, Sasso RC, Ludwig SC. Lateral mass screw fixation in the cervical spine: A systematic literature review. J Bone Joint Surg Am. 2013. 95: 2136-43
2. Desai S, Sethi A, Ninh CC, Bartol S, Vaidya R. Pedicle screw fixation of the C7 vertebra using an anteroposterior fluoroscopic imaging technique. Eur Spine J. 2010. 19: 1953-9
3. Johnston TL, Karaikovic EE, Lautenschlager EP, Marcu D. Cervical pedicle screws vs. lateral mass screws: Uniplanar fatigue analysis and residual pullout strengths. Spine J. 2006. 6: 667-72
4. Katonis P, Papadakis SA, Galanakos S, Paskou D, Bano A, Sapkas G. Lateral mass screw complications: Analysis of 1662 screws. J Spinal Disord Tech. 2011. 24: 415-20
5. Mohamed E, Ihab Z, Moaz A, Ayman N, Haitham AE. Lateral mass fixation in subaxial cervical spine: Anatomic review. Global Spine J. 2012. 2: 39-46
6. Nakashima H, Yukawa Y, Imagama S, Kanemura T, Kamiya M, Yanase M. Complications of cervical pedicle screw fixation for nontraumatic lesions: A multicenter study of 84 patients. J Neurosurg Spine. 2012. 16: 238-47
7. Pelton MA, Schwartz J, Singh K. Subaxial cervical and cervicothoracic fixation techniques-indications, techniques, and outcomes. Orthop Clin North Am. 2012. 43: 19-28, vii
8. Regan CM, Emmanuel S, Hornik C, Weinhold P, Lim MR. Lateral mass versus hybrid construct for cervical laminectomy and fusion. Orthopedics. 2013. 36: e484-8
9. Theologis AA, Burch S. Safety and Efficacy of Reconstruction of Complex Cervical Spine Pathology Using Pedicle Screws Inserted with Stealth Navigation and 3D Image-Guided (O-Arm) Technology. Spine (Phila Pa 1976). 2015. 40: 1397-406
10. Uehara M, Takahashi J, Ikegami S, Mukaiyama K, Kuraishi S, Shimizu M. Screw perforation features in 129 consecutive patients performed computer-guided cervical pedicle screw insertion. Eur Spine J. 2014. 23: 2189-95
11. Uehara M, Takahashi J, Mukaiyama K, Kuraishi S, Shimizu M, Ikegami S. Mid-term results of computer-assisted cervical pedicle screw fixation. Asian Spine J. 2014. 8: 759-67
12. Xu R, McGirt MJ, Sutter EG, Sciubba DM, Wolinsky JP, Witham TF. Biomechanical comparison between C-7 lateral mass and pedicle screws in subaxial cervical constructs. Presented at the 2009 Joint Spine Meeting. Laboratory investigation. J Neurosurg Spine. 2010. 13: 688-94
13. Yoshihara H, Passias PG, Errico TJ. Screw-related complications in the subaxial cervical spine with the use of lateral mass versus cervical pedicle screws: A systematic review. J Neurosurg Spine. 2013. 19: 614-23
14. Yukawa Y, Kato F, Ito K, Horie Y, Hida T, Nakashima H. Placement and complications of cervical pedicle screws in 144 cervical trauma patients using pedicle axis view techniques by fluoroscope. Eur Spine J. 2009. 18: 1293-9