- Department of Neurosurgery, Gunma University, Maebashi, Gunma, Japan.
Correspondence Address:
Hiroya Shimauchi-Ohtaki, Department of Neurosurgery, Gunma University, Maebashi, Gunma, Japan.
DOI:10.25259/SNI_1152_2021
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Hiroya Shimauchi-Ohtaki, Fumiaki Honda, Shunsuke Nakamura, Yuhei Yoshimoto. Severe constipation due to sacral perineural cysts in a pediatrics patient: A case report. 22-Jul-2022;13:317
How to cite this URL: Hiroya Shimauchi-Ohtaki, Fumiaki Honda, Shunsuke Nakamura, Yuhei Yoshimoto. Severe constipation due to sacral perineural cysts in a pediatrics patient: A case report. 22-Jul-2022;13:317. Available from: https://surgicalneurologyint.com/surgicalint-articles/11733/
Abstract
Background: Symptomatic perineural cysts are rare in pediatric patients. Severe bowel dysfunction caused by the perineural cysts at the sacral level is particularly rare in children. Moreover, the long-term outcome of surgery for the perineural cysts in pediatric patients is uncertain. Here, we describe a rare case of perineural cysts originating in the S3 roots in a pediatric patient that manifested as severe constipation.
Case Description: The case was a 13-year-old girl who presented with intractable vomiting and constipation. She also had low back and buttock pain, urinary incontinence, and periproctal sensory disturbance. Radiological studies revealed bilateral perineural cysts originating from the S3 nerve roots, which were considered to be the cause of her symptoms. Microsurgical decompression of the cysts relieved her intractable bowel dysfunction. There has been no recurrence in the 5 years since surgery.
Conclusion: This case suggests that microsurgery for severe bowel dysfunction due to symptomatic perineural cysts could have a satisfactory long-term outcome in pediatric patients.
Keywords: Bowel dysfunction, Pediatric patient, Perineural cyst, Tarlov cyst
INTRODUCTION
Perineural cysts, also known as Tarlov cysts, develop between the endoneurium and perineurium of a nerve root.[
CASE DESCRIPTION
A 13-year-old girl presented with an intractable vomiting and constipation that did not respond to medical treatment. She was referred to our department when MRI revealed cysts at the sacral level. She was found to have low back and buttock pain, urinary incontinence, and periproctal sensory disturbance.
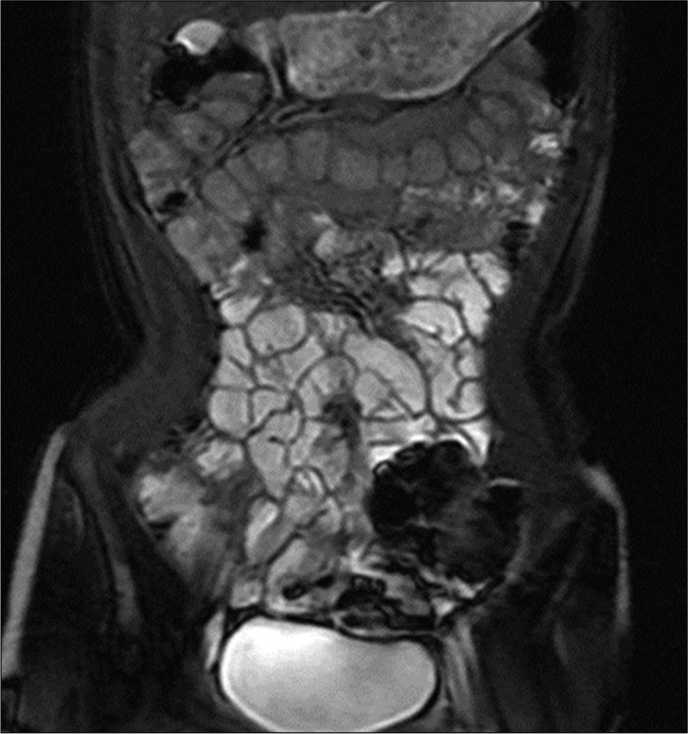
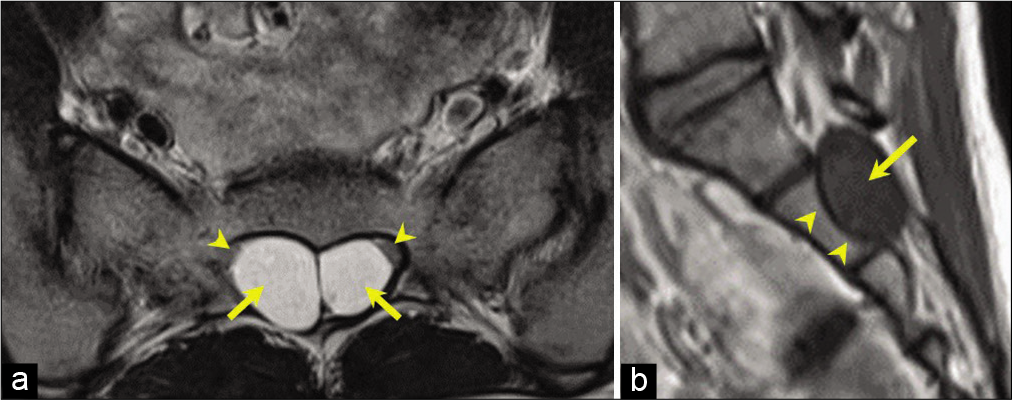
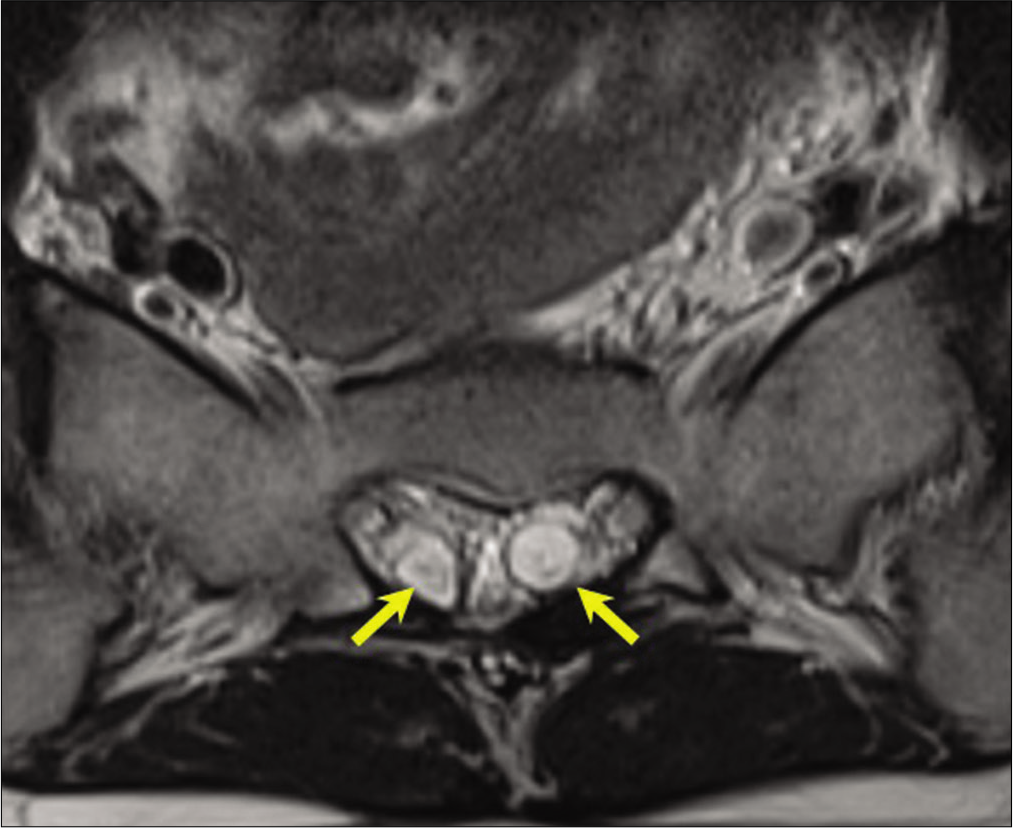
The MRI showed intestinal and bladder distension, suggesting severe bowel and bladder dysfunction [
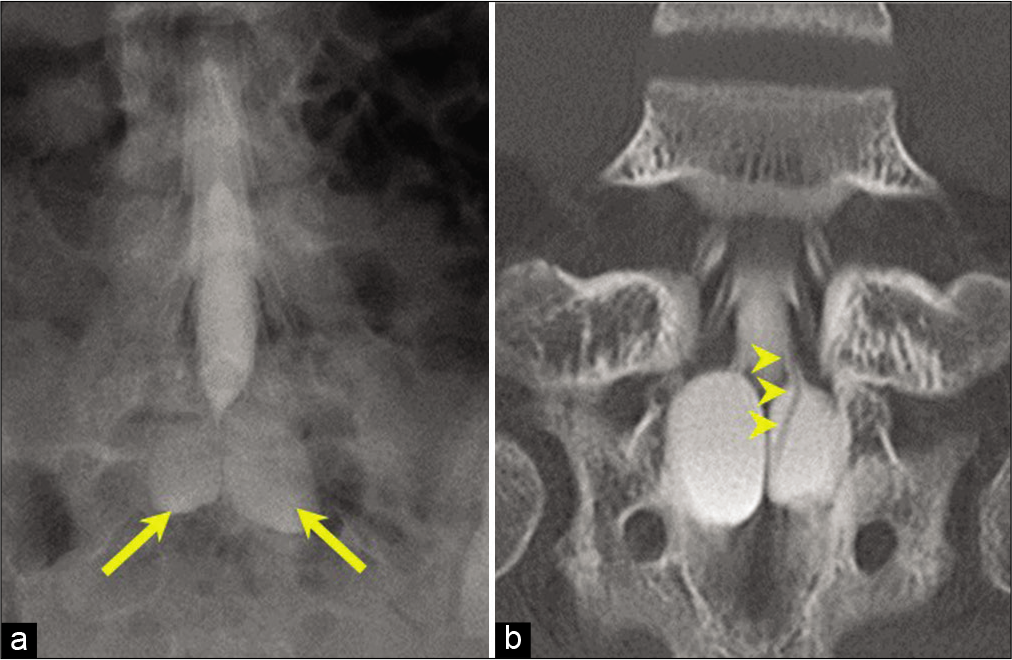
Figure 3:
Preoperative myelogram and computed tomography myelogram. (a) Myelogram showing bilateral sacral cysts (arrows) with immediate influx of contrast medium. (b) Computed tomography myelogram obtained 3 h after injection shows contrast medium in the cysts that originated from the S3 roots (arrowheads).
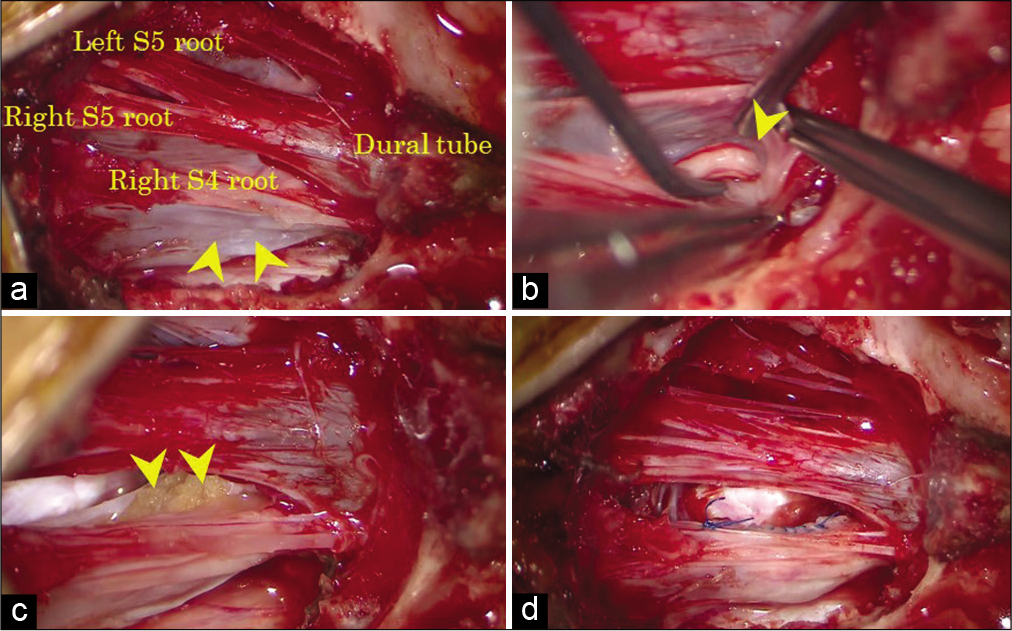
A bilateral partial laminectomy was performed at S1-2. The cysts, dural tube, and nerve roots were detected [
Figure 4:
Intraoperative photographs. (a) Photograph showing the perineural cyst (arrowheads), dural tube, and nerve roots after bilateral S1–2 partial laminectomy. (b) The right S3 root is seen within the cyst after the cyst wall incision. The proximal end of the S3 root in the cyst (arrowhead). (c) Sealing of the proximal end of the S3 root in the cyst using autologous fat tissue (arrowheads) and fibrin glue. (d) Cyst wall was sutured.
After the surgery, her severe bowel dysfunction was relieved. Although she complained of radicular pain in the left thigh after the surgery, the pain was relieved later. Moreover, there has been no recurrence until 5 years after her surgery [
DISCUSSION
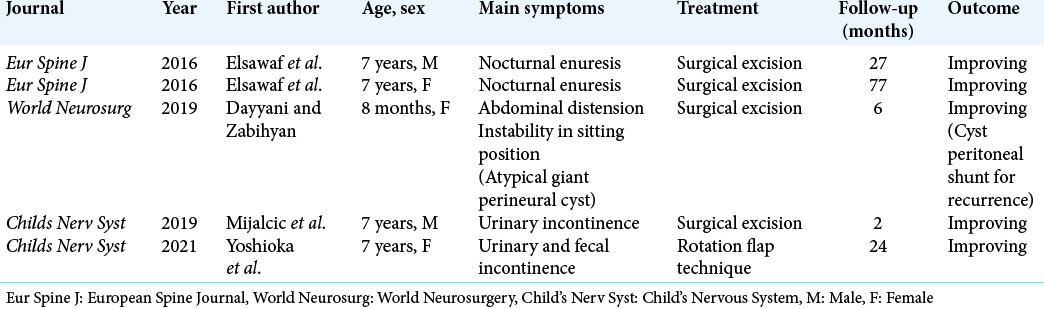
We have encountered an exceedingly rare case of perineural cysts originating from the S3 nerve roots of a pediatric patient that manifested as severe bowel dysfunction and was treated successfully by microsurgical decompression. A search of the literature revealed only a few reports on surgical outcome of pediatric perineural cysts [
Although various treatment strategies have been described, there is no consensus on the treatment of perineural cysts.[
CONCLUSION
This case suggests that microsurgery for severe bowel dysfunction due to symptomatic perineural cysts could have a satisfactory long-term outcome in pediatric patients.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Burke JF, Thawani JP, Berger I, Nayak NR, Stephen JH, Farkas T. Microsurgical treatment of sacral perineural (Tarlov) cysts: Case series and review of the literature. J Neurosurg Spine. 2016. 24: 700-7
2. Cantore G, Bistazzoni S, Esposito V, Tola S, Lenzi J, Passacantilli E. Sacral Tarlov cyst: Surgical treatment by clipping. World Neurosurg. 2013. 79: 381-9
3. Caspar W, Papavero L, Nabhan A, Loew C, Ahlhelm F. Microsurgical excision of symptomatic sacral perineurial cysts: A study of 15 cases. Surg Neurol. 2003. 59: 101-5
4. Dayyani M, Zabihyan S. Giant Tarlov cyst of infancy. World Neurosurg. 2019. 123: 348-50
5. Elsawaf A, Awad TE, Fesal SS. Surgical excision of symptomatic sacral perineurial Tarlov cyst: Case series and review of the literature. Eur Spine J. 2016. 25: 3385-92
6. Lucantoni C, Than KD, Wang AC, Valdivia-Valdivia JM, Maher CO, La Marca F. Tarlov cysts: A controversial lesion of the sacral spine. Neurosurg Focus. 2011. 31: E14
7. Mijalcic MR, Djurovic B, Cvrkota I, Jokovic M, Bascarevic V, Micovic M. Tarlov cyst-a rare lesion in children: Case report. Childs Nerv Syst. 2019. 35: 701-5
8. Mummaneni PV, Pitts LH, McCormack BM, Corroo JM, Weinstein PR. Microsurgical treatment of symptomatic sacral Tarlov cysts. Neurosurgery. 2000. 47: 74-8
9. Ramadorai UE, Hire JM, DeVine JG. Magnetic resonance imaging of the cervical, thoracic, and lumbar spine in children: spinal incidental findings in pediatric patients. Glob Spine J. 2014. 4: 223-8
10. Sharma M, SirDeshpande P, Ugiliweneza B, Dietz N, Boakye M. A systematic comparative outcome analysis of surgical versus percutaneous techniques in the management of symptomatic sacral perineural (Tarlov) cysts: a meta-analysis. J Neurosurg Spine. 2019. 30: 623-34
11. Weigel R, Polemikos M, Uksul N, Krauss JK. Tarlov cysts: Long-term follow-up after microsurgical inverted plication and sacroplasty. Eur Spine J. 2016. 25: 3403-10
12. Yoshioka F, Shimokawa S, Masuoka J, Inoue K, Ogata A, Abe T. Elimination of the check-valve mechanism of the sacral Tarlov cyst using a rotation flap technique in a pediatric patient: Technical note. Childs Nerv Syst. 2021. 37: 1741-5