- Department of Neurosurgery, Cairo University Hospital, Cairo, Egypt
- Department of Neurosurgery, Hannover Medical School, Hannover Medical School, Hannover, Germany
- Department of Neurology, Cairo University Hospital, Cairo, Egypt
- Department of Neurosurgery, Hamed Abdelma’aboud Mostafa, AlAzher University, Dameitta, Egypt
Correspondence Address:
Mohammed A. Azab, Department of Neurosurgery, Cairo University Hospital, Cairo, Egypt.
DOI:10.25259/SNI_431_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Mohammed A. Azab1, Oday Atallah2, Nour El-Gohary3, Ahmed Hazim1, Hamed Abdelma’aboud Mostafa4. Small-cell neuroendocrine carcinoma of the cervix with leptomeningeal spread: A rare coincidence report and literature review. 30-Aug-2024;15:310
How to cite this URL: Mohammed A. Azab1, Oday Atallah2, Nour El-Gohary3, Ahmed Hazim1, Hamed Abdelma’aboud Mostafa4. Small-cell neuroendocrine carcinoma of the cervix with leptomeningeal spread: A rare coincidence report and literature review. 30-Aug-2024;15:310. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13071
Abstract
Background: Metastasis from cancers of the cervix to the central nervous system is relatively uncommon. Small-cell neuroendocrine cancer of the cervix is a very rare tumor with a high tendency to spread early.
Case Description: A 33-year-old-woman was diagnosed with a small-cell neuroendocrine cancer of the cervix after complaining about a long time of post-coital bleeding. The patient was treated with eight cycles of chemotherapy and whole pelvis consolidation radiotherapy. One year later, the patient experienced local recurrence with metastases to the liver, left adrenal, and brain. Brain metastases were treated with radiosurgery. The patient started immunotherapy. Two months later, the patient was presented to the emergency department with urinary incontinence, neck pain, and difficulty walking. She was then diagnosed with craniospinal leptomeningeal disease (LMD). The patient received craniospinal palliative radiation therapy. The disease activity was severely progressive, and the patient passed out within 10 days after being diagnosed with cranial LMD.
Conclusion: A high index of suspicion for LMD is essential in patients diagnosed with cervix cancer who present with unexplained neurologic symptoms, especially with the high-grade neuroendocrine cancer type. Implementing robust research to uncover the biology of these aggressive tumors is important due to the rarity of this pathology.
Keywords: Cervix, Leptomeningeal disease, Metastasis, Neuroendocrine cell cancer
INTRODUCTION
Leptomeningeal disease (LMD) is characterized by diffuse multifocal involvement of the meninges by cancerous cells. It is considered a lethal complication of malignancy. Cancers that are associated with a high incidence of LMD include melanoma, lymphoma, leukemia, and lung and breast cancer.[
Recently, cervical cancer incidence has declined due to the widespread Human papilloma virus (HPV) vaccinations and the regular screening.[
CASE DESCRIPTION
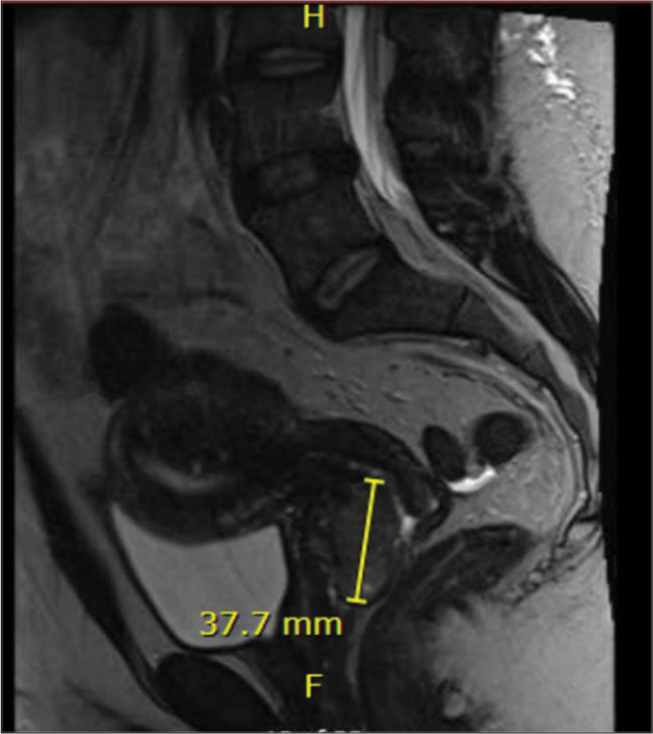
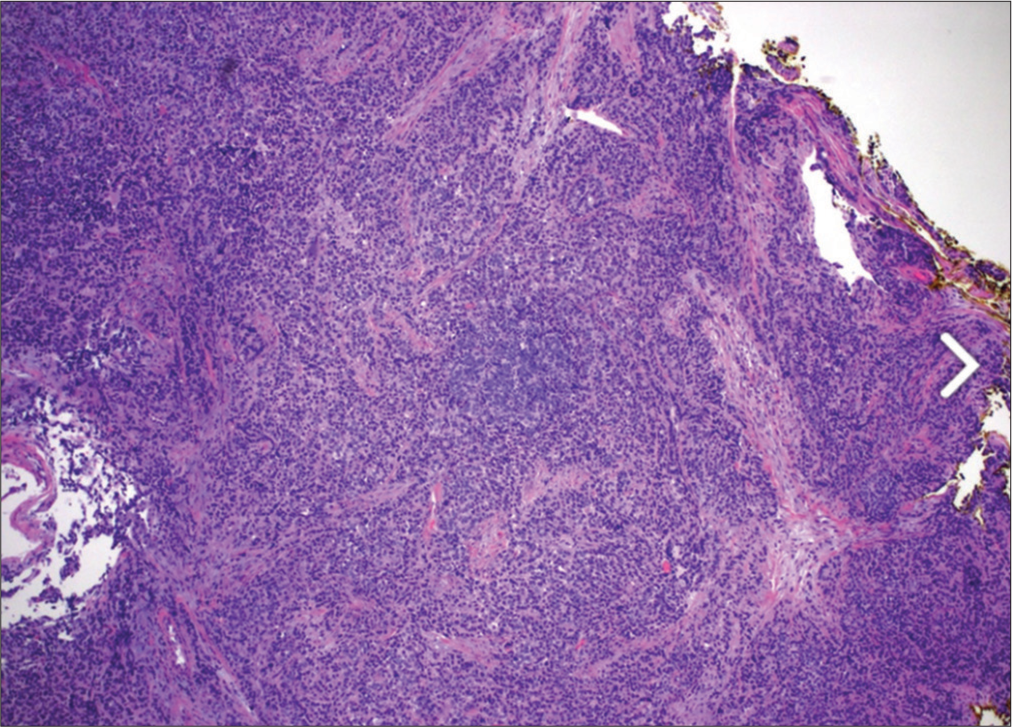
A 33-year-old woman was referred to a gynecological examination on June 8, 2018, due to repeated episodes of postcoital bleeding and pelvic pain. A mass lesion was detected on magnetic resonance imaging (MRI) in the cervix and upper third of the vagina and measured about 3.8 × 2.7 (AP diameter) × 3.6 (craniocaudal) [
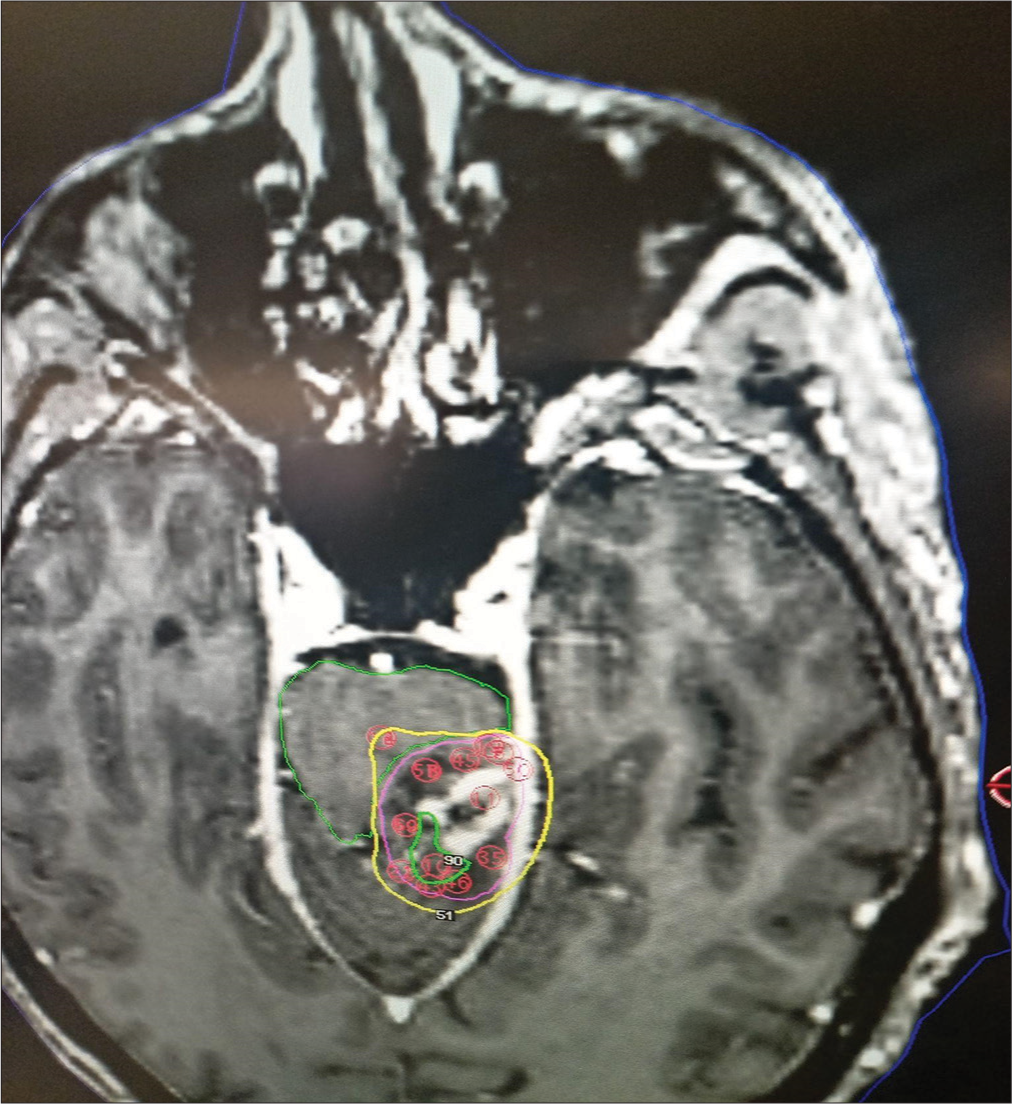
The patient was treated with chemotherapy in the form of eight cycles of carboplatin, etoposide, and whole pelvis consolidation radiotherapy with a dose of 4500 cGy in 25 fx, and then he received brachytherapy to the cervix and parametrium with a dose of 1400 cGy in 2 fx. One year later, the patient had a recurrence with multiple metastases affecting the liver, adrenal gland, and brain. The brain metastases were treated with Gamma Knife radiosurgery [
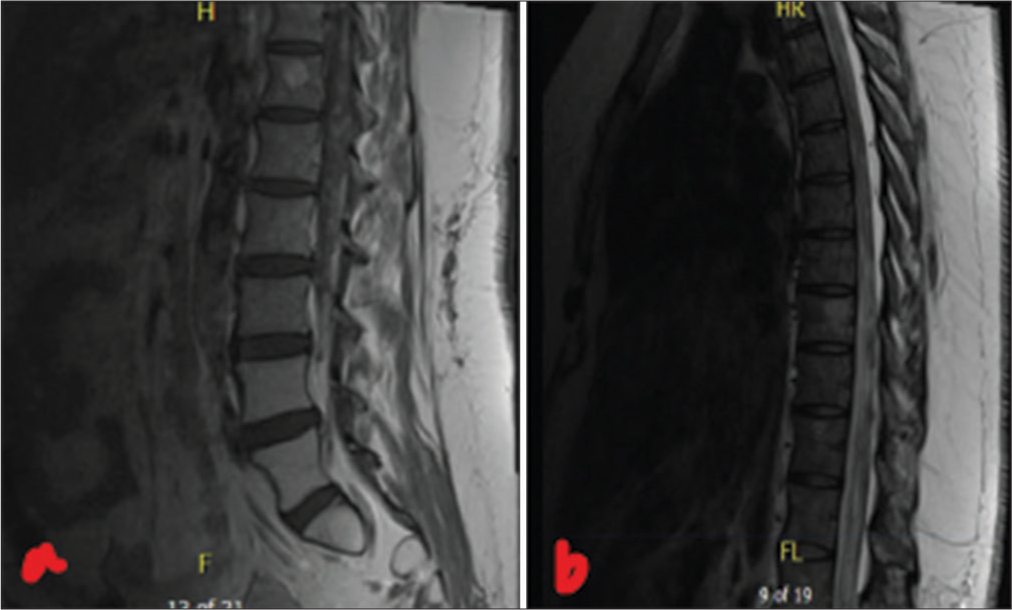
Two months later, she presented to the emergency department with neck stiffness, cervical pain, trouble walking, and bilateral lower limb numbness associated with urinary incontinence. The patient had a Glasgow coma scale (GCS) of 15. Neurologic examination was positive only for cervical pain limitation. MRI spine revealed leptomeningeal enhancement extending from T2 superiorly through the conus medullaris and involving the cauda equina nerve roots [
Figure 4:
(a) Lumbar spine magnetic resonance imaging (MRI) T2 showing leptomeningeal enhancement along the conus and innumerable tiny nodular enhancing foci along the descending cauda equina nerve roots. (b) Thoracic spine MRI T2 with contrast showing diffuse leptomeningeal enhancement of the thoracic cord.
DISCUSSION
Neuroendocrine cells have been identified throughout the female genital tract, frequently affecting the uterus and ovaries. In 1972, Albores-Saavedra et al. first identified this pathology.[
The most common primary treatment reported in the literature was radical surgery combined with chemotherapy, and platinum and etoposide were the most used.[
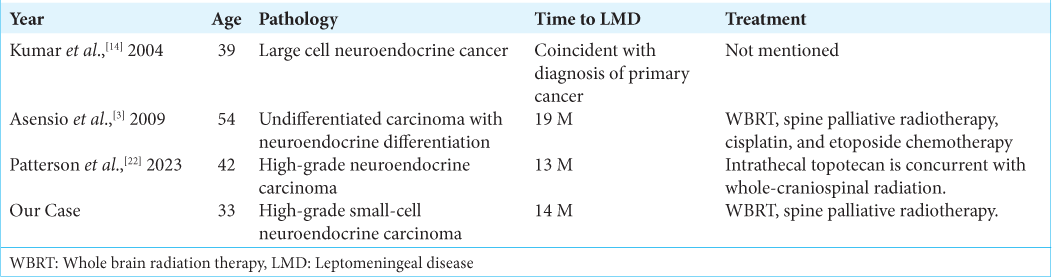
There is only one reported case of LMD in the context of a cervical high-grade neuroendocrine tumor.[
Given the dismal prognosis of LMD, the most common treatment is palliative radiation. Clinical trials involving LMD treatment include a combination of radiotherapy, systemic therapy, and intrathecal chemotherapy; however, studies have shown variable responses to treatment, making it difficult to use a general treatment protocol.[
Whole brain radiotherapy dismantles the integrity of the blood-brain barrier and increases the cerebrospinal fluid (CSF) concentration of systemic therapies. Circulating tumor cells in the CSF favor the use of intrathecal therapy. The most used agents for intrathecal chemotherapy are methotrexate, thiotepa, and cytarabine.[
CONCLUSION
Clinical trials that involve small-cell neuroendocrine cell cancer (SCNECC) should be recruited to understand factors associated with LMD and determine the most efficient therapy. We report a rare case of a patient with SCNECC with brain metastasis and craniospinal LMD. The type of LMD in our case was mixed, which is different from the previously reported case.[
Authors’ contributions
Dr. MA contributed to designing the idea and manuscript writing, Dr. AH contributed to the final review, and Dr. HM contributed to the editing. Dr. N contributed to the table design. Dr OA contributed to the final review.
Ethical approval
The research/study was approved by the Institutional Review Board at Cairo University Hospital, number CU1335, and dated January 10, 2024.
Declaration of patient consent
The authors certify that they have obtained appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
Acknowledgment
I acknowledge the equal participation of all authors in the design and production of this manuscript.
References
1. Ahn SJ, Joo B, Park M, Park HH, Suh SH, Ahn SG. Dural metastasis in breast cancer: MRI-based morphological subtypes and their clinical implications. Cancer Res Treat. 2024. p.
2. Albores-Saavedra J, Larraza O, Poucell S, Rodríguez Martínez HA. Carcinoid of the uterine cervix: Additional observations on a new tumor entity. Cancer. 1976. 38: 2328-42
3. Asensio N, Luis A, Costa I, Oliveira J, Vaz F. Meningeal carcinomatosis and uterine carcinoma: Three different clinical settings and review of the literature. Int J Gynecol Cancer. 2009. 19: 168-72
4. Borm KJ, Behzadi ST, Hörner-Rieber J, Krug D, Baumann R, Corradini S. DEGRO guideline for personalized radiotherapy of brain metastases and leptomeningeal carcinomatosis in patients with breast cancer. Strahlenther Onkol. 2024. 200: 259-75
5. Brown PD, Ballman KV, Cerhan JH, Anderson SK, Carrero XW, Whitton AC. Postoperative stereotactic radiosurgery compared with whole brain radiotherapy for resected metastatic brain disease (NCCTG N107C/CEC•3): A multicentre, randomized, controlled, phase 3 trial. Lancet Oncol. 2017. 18: 1049-60
6. Chilkulwar A, Pottimutyapu R, Wu F, Padooru KR, Pingali SR, Kassem M. Leptomeningeal carcinomatosis associated with papillary renal cell carcinoma. Ecancermedicalscience. 2014. 8: 468
7. Eichhorn JH, Young RH. Neuroendocrine tumors of the genital tract. Am J Clin Pathol. 2001. 115: S94-112
8. Ishikawa M, Kasamatsu T, Tsuda H, Fukunaga M, Sakamoto A, Kaku T. Prognostic factors and optimal therapy for stages I-II neuroendocrine carcinomas of the uterine cervix: A multi-center retrospective study. Gynecol Oncol. 2018. 148: 139-46
9. Jaeckle KA, Dixon JG, Anderson SK, Moreno-Aspitia A, Colon-Otero G, Hebenstreit K. Intra-CSF topotecan in treatment of breast cancer patients with leptomeningeal metastases. Cancer Med. 2020. 9: 7935-42
10. Kim MJ, Kim NR, Cho HY, Lee SP, Ha SY. Differential diagnostic features of small cell carcinoma in the uterine cervix. Diagn Cytopathol. 2008. 36: 618-23
11. Kim Y, Ha HJ, Kim JS, Chung JH, Koh JS, Park S. Significance of cytologic smears in the diagnosis of small cell carcinoma of the uterine cervix. Acta Cytol. 2002. 46: 637-44
12. Kirkpatrick JP. Classifying leptomeningeal disease: An essential element in managing advanced metastatic disease in the central nervous system. Int J Radiat Oncol Biol Phys. 2020. 106: 587-8
13. Klöppel G. Neuroendocrine neoplasms: Dichotomy, origin and classifications. Visc Med. 2017. 33: 324-30
14. Kumar S, Nair S, Alexander M. Carcinomatous meningitis occurring prior to a diagnosis of large cell neuroendocrine carcinoma of the uterine cervix. J Postgrad Med. 2004. 50: 311-2
15. Le Rhun E, Devos P, Weller J, Seystahl K, Mo F, Compter A. Prognostic validation and clinical implications of the EANO ESMO classification of leptomeningeal metastasis from solid tumors. Neuro Oncol. 2021. 23: 1100-12
16. Le Rhun E, Weller M, Brandsma D, Van den Bent M, de Azambuja E, Henriksson R. EANO-ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up of patients with leptomeningeal metastasis from solid tumours. Ann Oncol. 2017. 28: iv84-99
17. Mahajan A, Ahmed S, McAleer MF, Weinberg JS, Li J, Brown P. Post-operative stereotactic radiosurgery versus observation for completely resected brain metastases: A single-centre, randomized, controlled, phase 3 trial. Lancet Oncol. 2017. 18: 1040-8
18. Marlina YS, Novirianthy R, Beočanin A. Palliative radiotherapy for leptomeningeal metastases after photon-based intensity-modulated radiotherapy in a nasopharyngeal cancer patient. Narra J. 2023. 3: e266
19. Mizumatsu S, Wakabayashi K, Terashima Y. Palliative treatment of leptomeningeal carcinomatosis from renal cell carcinoma with local cyberknife radiotherapy and systemic pazopanib therapy: A case report. Cureus. 2024. 16: e54025
20. Muñoz N, Bosch FX, de Sanjosé S, Herrero R, Castellsagué X, Shah KV. Epidemiologic classification of human papillomavirus types associated with cervical cancer. N Engl J Med. 2003. 348: 518-27
21. Nayar G, Ejikeme T, Chongsathidkiet P, Elsamadicy AA, Blackwell KL, Clarke JM. Leptomeningeal disease: Current diagnostic and therapeutic strategies. Oncotarget. 2017. 8: 73312-28
22. Patterson JD, Farach AM, Singh M, Britz GW, Rostomily RC. Leptomeningeal metastasis from neuroendocrine carcinoma of the cervix: Illustrative case. J Neurosurg Case Lessons. 2023. 5: CASE22457
23. Prabhu RS, Turner BE, Asher AL, Marcrom SR, Fiveash JB, Foreman PM. A multi-institutional analysis of presentation and outcomes for leptomeningeal disease recurrence after surgical resection and radiosurgery for brain metastases. Neuro Oncol. 2019. 21: 1049-59
24. Qin J, Shahangian S, Saraiya M, Holt H, Gagnon M, Sawaya GF. Trends in the use of cervical cancer screening tests in a large medical claims database, United States, 2013-2019. Gynecol Oncol. 2021. 163: 378-84
25. Takayanagi A, Florence TJ, Hariri OR, Armstrong A, Yazdian P, Sumida A. Brain metastases from cervical cancer reduce longevity independent of overall tumor burden. Surg Neurol Int. 2019. 10: 176
26. Tan CY, Yang QL, Xu N, Wang HJ. Small cell neuroendocrine carcinoma of the cervix: An analysis for 5 cases and literature review. Asian J Surg. 2024. 47: 2508-9
27. Tempfer CB, Tischoff I, Dogan A, Hilal Z, Schultheis B, Kern P. Neuroendocrine carcinoma of the cervix: A systematic review of the literature. BMC Cancer. 2018. 18: 530
28. Pavithra V, Shalini CN, Priya S, Rani U, Rajendiran S, Joseph LD. Small cell neuroendocrine carcinoma of the cervix: A rare entity. J Clin Diagn Res. 2014. 8: 147-8