- Department of Neurosurgery, Medical School, University Sidi Mohammed Ben Abdellah, Hassan II University Hospital of Fez, Fez, Morocco.
Correspondence Address:
Marouane Hammoud, Department of Neurosurgery, Medical School, University Sidi Mohammed Ben Abdellah, Hassan II University Hospital of Fez, Fez,
DOI:10.25259/SNI_291_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Marouane Hammoud, Dramane Cisse, Khalid Chakour, Mohamed El Faiz Chaoui. Spinal epidermoid cyst associated with limited dorsal myeloschisis. 24-May-2024;15:169
How to cite this URL: Marouane Hammoud, Dramane Cisse, Khalid Chakour, Mohamed El Faiz Chaoui. Spinal epidermoid cyst associated with limited dorsal myeloschisis. 24-May-2024;15:169. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=12910
Abstract
Background: Epidermoid cysts (ECs) are rare benign tumors arising from epidermal cells, associated with congenital abnormalities or acquired through trauma, surgery, or lumbar punctures. They represent
Case Description: A 7-year-old neurologically intact male had a dorsal skin mass since birth located posteriorly in the midline of the inferior thoracic spine. The mass was palpable, painless, mobile, vascularized, and could be transilluminated. Thoracic magnetic resonance imaging showed an extensive intradural extramedullary cystic lesion extending from D6 to D8 that did not enhance with contrast, accompanied by a subcutaneous fluid collection at D8–D9 communicating with the subarachnoid space. The patient underwent gross total resection of the lesion, pathologically confirmed as an EC. The postoperative course was uneventful, with no recurrence 1 year postoperatively.
Conclusion: LDM may be associated with ECs. Early diagnosis and surgical resection of these lesions are essential for favorable outcomes.
Keywords: Congenital epidermoid cyst, Limited dorsal myeloschisis, Spine
INTRODUCTION
Limited dorsal myeloschisis (LDM) is a rare form of spinal dysraphism characterized by a focal midline skin lesion and a fibroneural pedicle or stalk connecting the spinal cord to the overlying skin lesion.[
CASE DESCRIPTION
A 7-year-old male presented with a progressively enlarging lower thoracic dorsal T8–T9 skin mass since birth. On examination, it was palpable, painless, mobile, vascularized, and readily transilluminated [
Figure 2:
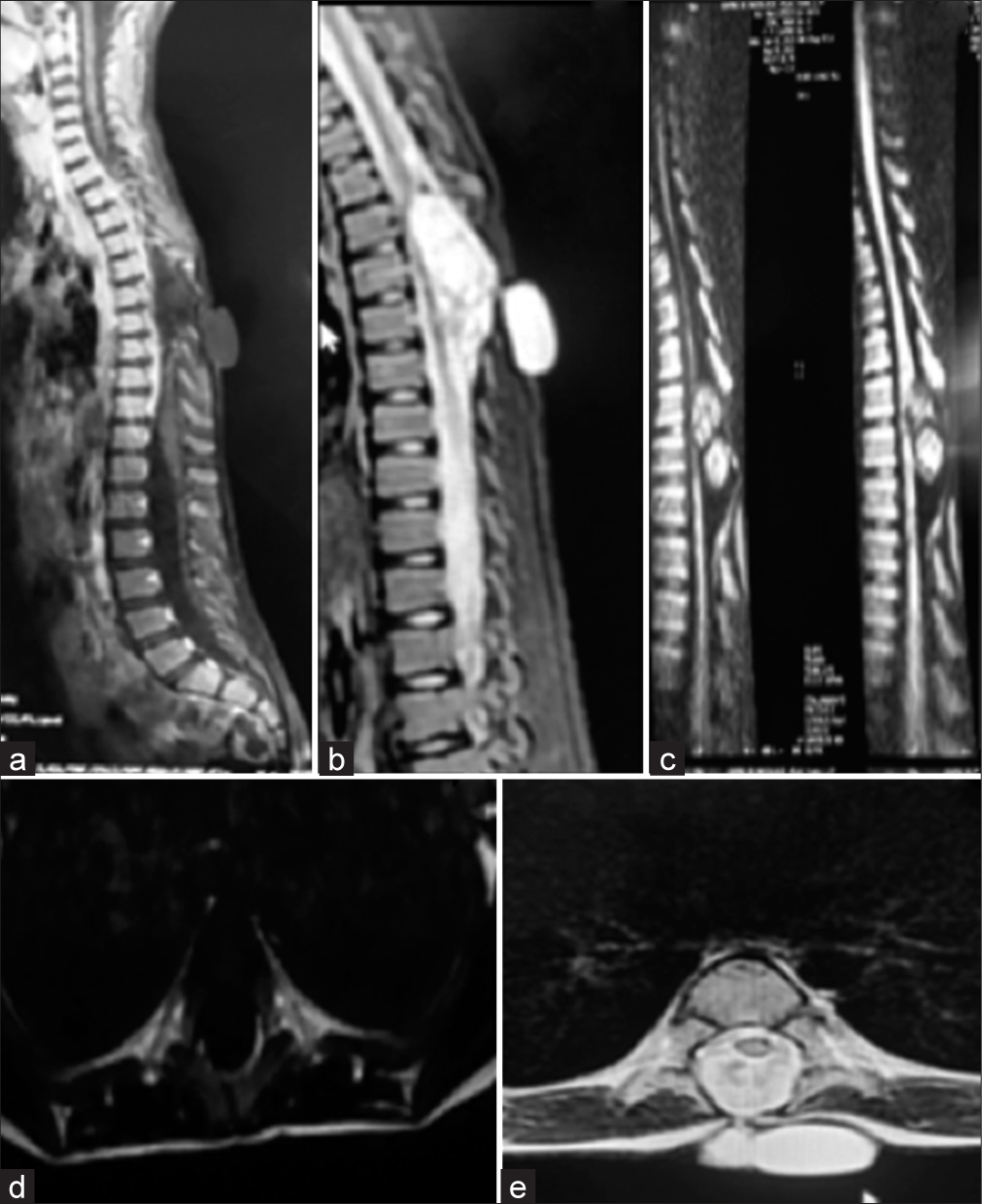
(a) Medullary magnetic resonance imaging (MRI) on a sagittal section in T1-weighted sequence ,(b) T2 sequence, (c) and short-tau inversion-recovery showing an extramedullary intradural cyst from D6 to D8 in T1 hyposignal and T2 hypersignal. (d) Spinal cord MRI on axial section in T1-weighted sequence objecting the extramedullary intradural cystic lesion in T1 hyposignal, (e) T2 sequence showing the subcutaneous fluid formation in T2 hypersignal at the level of D8-D9 communicating with the subarachnoid spaces.
Surgery
During surgery, the LDM was initially punctured, followed by a D6–D7 laminectomy. The LDM stalk extended deep through a midline defect into the ligamentum flavum and through the dura. Intradurally, the stalk was divided [
Postoperative course
The postoperative course was uneventful, and the patient was discharged 10 days following surgery. The patient remained neurologically intact, and no postoperative cerebrospinal fluid fistula developed. Histopathology confirmed the diagnosis of an EC [
Figure 4:
In the histopathological examination, (a) cystic lesion with stratified squamous epithelium (black arrow) (hematoxylin-eosin, ×100). (b) Stained by leukocyte common antigen (LCA), around the cystic lesion with stratified squamous epithelium (LCA, ×100). (c) Stratified squamous epithelium stained with pancytokeratin. Desquamation of keratin from the epithelial lining can be observed (pancytokeratin, ×100) (White arrow), inflammatory cells (black arrowhead).
DISCUSSION
Frequency and location of ECs
The term “tumor perlée” (pearly tumors) was coined by Croveilhier in 1835 to describe the first EC.[
LDM
LDM represents a rare form of closed spinal dysraphism often associated with various congenital anomalies such as tethered cord, lipoma, lipomyelomeningocele, split cord malformation, and teratoma, among others.[
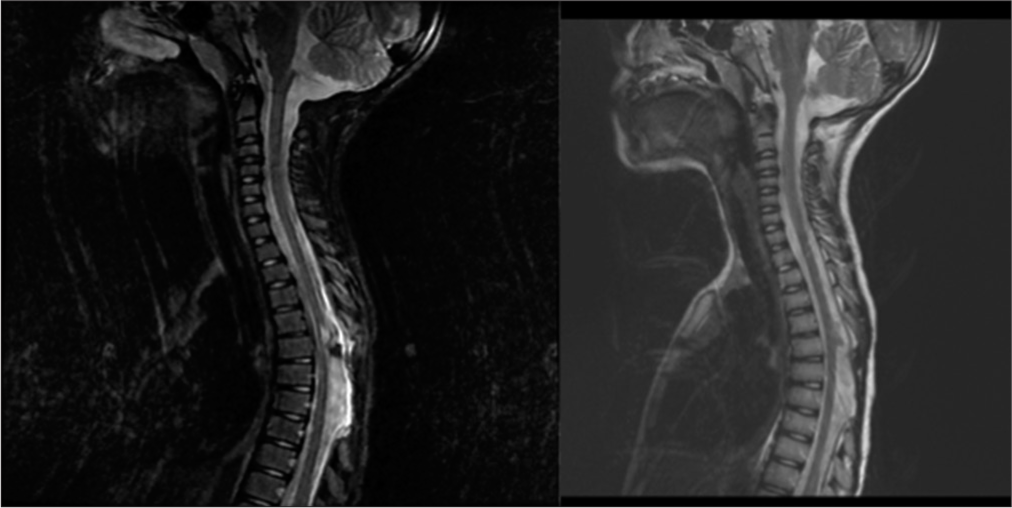
MRI diagnosis of EC and LDM
On MRI, ECs exhibit variable characteristics. They typically appear isointense/hypointense on T1-weighted images and hyperintense on T2-weighted images, with limited enhancement under contrast. However, the presence of a thin rim of enhancement on gadolinium-enhanced MRI images has been inconsistently described in the literature.[
Surgery for EC
Surgical resection remains the cornerstone of EC treatment. Aimed at achieving gross total resection whenever feasible, as subtotal resections are associated with a higher risk of recurrence (reported at 11% by Sîrbu et al.[
Prognosis
Benign ECs generally have a favorable prognosis, particularly in younger patients at the time of diagnosis.[
CONCLUSION
Despite EC being benign and slow-growing lesions, early diagnosis and gross total excision achieves the best results with/without LDM.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Publication of this article was made possible by the James I. and Carolyn R. Ausman Educational Foundation.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Bansal S, Suri A, Borkar SA, Kale SS, Singh M, Mahapatra AK. Management of intramedullary tumors in children: Analysis of 82 operated cases. Childs Nerv Syst. 2012. 28: 2063-9
2. Bretz A, Van den Berge D, Storme G. Intraspinal epidermoid cyst successfully treated with radiotherapy: Case report. Neurosurgery. 2003. 53: 1429-31 discussion 1431-2
3. Dobre MC, Smoker WR, Moritani T, Kirby P. Spontaneously ruptured intraspinal epidermoid cyst causing chemical meningitis. J Clin Neurosci. 2012. 19: 587-9
4. Erşahin Y, Barçin E, Mutluer S. Is meningocele really an isolated lesion?. Childs Nerv Syst. 2001. 17: 487-90
5. Graillon T, Rakotozanany P, Meyer M, Dufour H, Fuentes S. Intramedullary epidermoid cysts in adults: Case report and updated literature review. Neurochirurgie. 2017. 63: 99-102
6. Manzo G, De Gennaro A, Cozzolino A, Martinelli E, Manto A. DWI findings in a iatrogenic lumbar epidermoid cyst: A case report. Neuroradiol J. 2013. 26: 469-75
7. Munshi A, Talapatra K, Ramadwar M, Jalali R. Spinal epidermoid cyst with sudden onset of paraplegia. J Cancer Res Ther. 2009. 5: 290-2
8. Sîrbu OM, Chirteş AV, Mitricã M, Sîrbu CA. Spinal intramedullary epidermoid cyst: Case report and updated literature review. World Neurosurg. 2020. 139: 39-50
9. Somasundaram A, Lesser GJ, Mott RT, Hsu W. Malignant transformation of an intramedullary epidermoid cyst in the thoracic region of the spinal cord: Case report. J Neurosurg Spine. 2013. 19: 591-4
10. Yin H, Zhang D, Wu Z, Zhou W, Xiao J. Surgery and outcomes of six patients with intradural epidermoid cysts in the lumbar spine. World J Surg Oncol. 2014. 12: 50