- Department of Neurosciences, University of the Witwatersrand, Johannesburg, Gauteng, South Africa.
Correspondence Address:
Dinesh Naidoo, Department of Neurosciences, University of the Witwatersrand, Johannesburg, Gauteng, South Africa.
DOI:10.25259/SNI_491_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Dinesh Naidoo. Spontaneous and rapid resolution of a massive lumbar disc herniation. 19-Jul-2021;12:352
How to cite this URL: Dinesh Naidoo. Spontaneous and rapid resolution of a massive lumbar disc herniation. 19-Jul-2021;12:352. Available from: https://surgicalneurologyint.com/surgicalint-articles/10986/
Abstract
Background: Most lumbar disc herniations can be successfully treated conservatively. However, massive lumbar disc herniations are often treated surgically to avoid permanent cauda equina syndromes/neurological deficits and potential litigation. Nevertheless, here, we present a 51-year-old female who refused lumbar surgery due to coronavirus disease 2019 (COVID-19) and sustained a full spontaneous recovery without surgical intervention.
Case Description: A 51-year-old female presented with a massive lumbar disc herniation at the L5S1 level. Despite refusing surgery for fear of getting COVID-19, she spontaneously neurologically improved without any residual neurological or radiographic sequelae.
Conclusion: Although the vast majority of patients with massive lumbar disc herniations are managed surgically, there are rare instances in which nonoperative management may be successful.
Keywords: Cauda equina syndrome, Conservative treatment, Coronavirus disease 2019, Litigation, Massive lumbar disc
INTRODUCTION
The first radiological demonstration of the spontaneous regression of a lumbar disc herniation was published in 1984[
Nevertheless, most spinal surgeons are reluctant to treat massive lumbar disc herniations conservatively due to the risk for developing a CES and permanent neurological sequelae.[
CASE PRESENTATION
Case history
A 51-year-old female presented with a 1-day history of the spontaneous onset of lower back pain radiating to both legs. On examination, she had mild right-sided plantar flexion weakness (4/5), without any bladder nor bowel disturbance.
The emergent magnetic resonance imaging (MRI) demonstrated a massive L5S1 lumbar disc herniation [
Patient refused surgery
The patient refused surgery as she was afraid that a hospital admission could result in her contracting coronavirus disease 2019 (COVID-19). Rather, she was treated with nonsteroidal anti-inflammatory medication, gabapentin, and weekly clinical examinations. Notably, we clearly discussed the risks/ complications of her developing a CES and the potential for a permanent, irreversible neurological injury/deficit.
The patient spontaneously improved and was able to return to work within 2 weeks. Three months later, she was neurologically normal, and the repeat MRI scan showed near-complete resolution of the original L5S1 massive disc herniation [
DISCUSSION
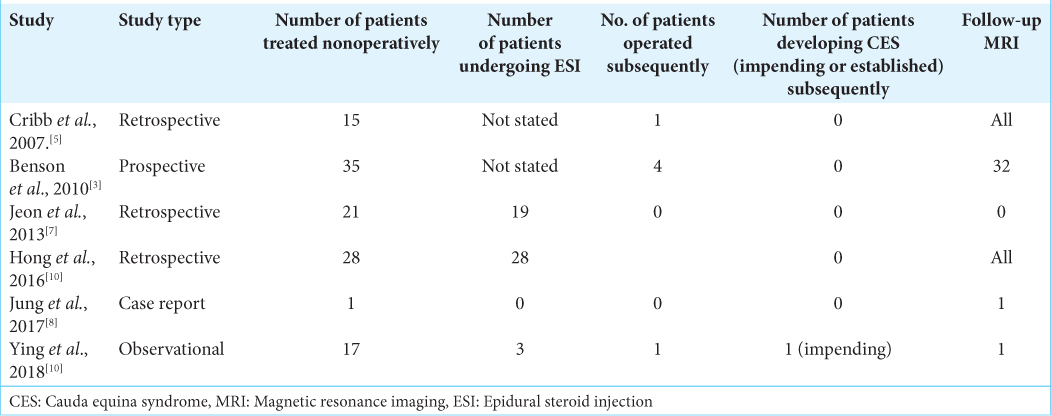
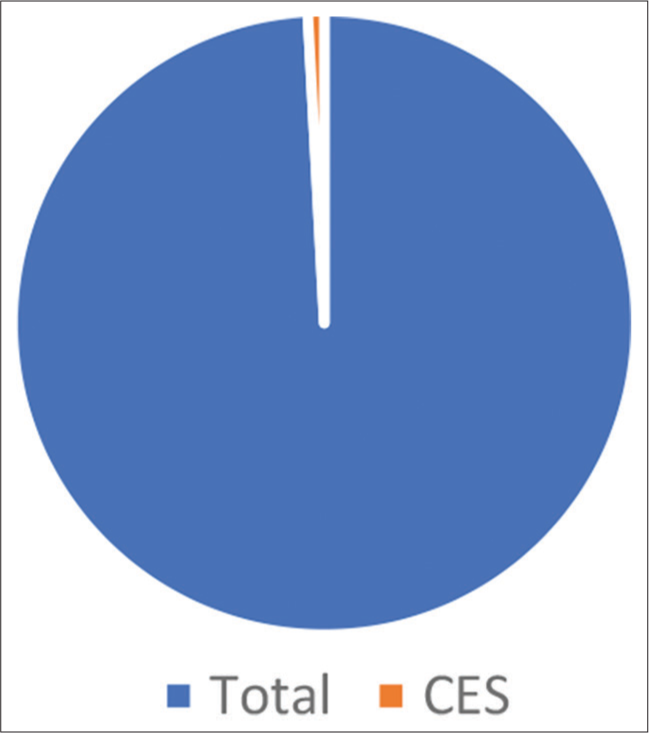
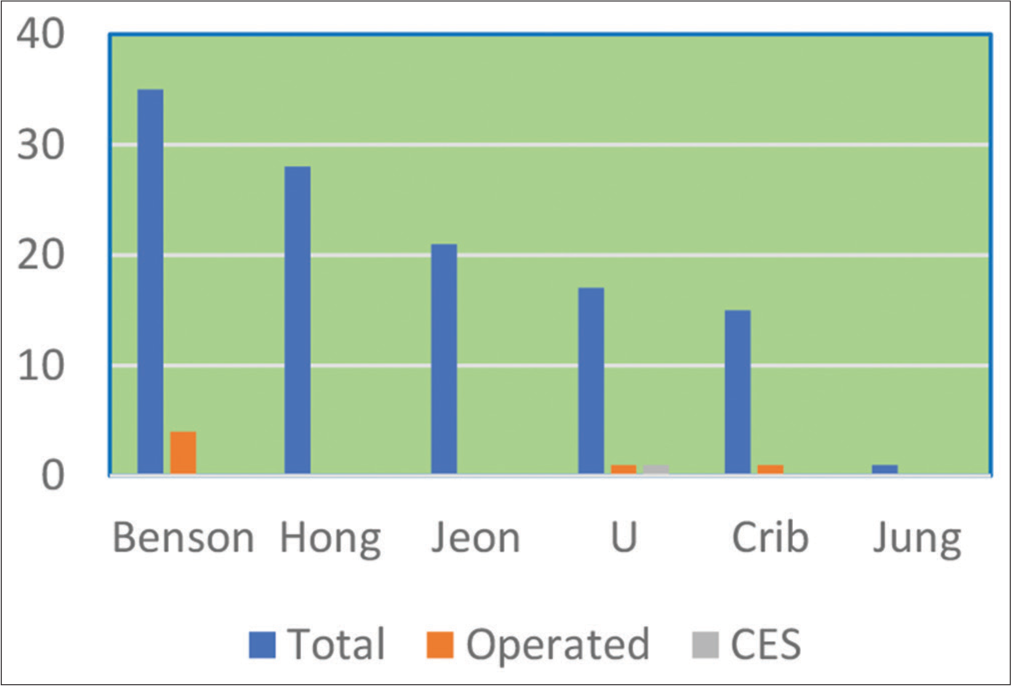
We reviewed six studies that described the conservative treatment of patients with massive lumbar disc herniations [
All patients were treated conservatively due to patient choice and because none presented with CES. The six studies yielded a total of 117 patients with massive lumbar disc herniations, treated conservatively for whom follow-up to symptomatic or radiological resolution or both were available. Although six patients eventually required surgery; only one patient underwent surgery for an impending CES, making an uneventful recovery.[
Both Hong et al.[
Further, all the patients in Hong et al.[
CONCLUSION
Due to the fear of contracting COVID-19, a 51-year-old female with a massive L5S1 disc herniation but minimal neurological deficit pursued a nonsurgical route resulting in full spontaneous resolution of her deficit and original MRI findings (3 months later).
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Benson RT, Tavares SP, Robertson SC, Sharp R, Marshall RW. Conservatively treated massive prolapsed discs: A 7-year follow-up. Ann R Coll Surg Engl. 2010. 92: 147-53
2. Chang CW, Lai PH, Yip CM, Hsu SS. Spontaneous regression of lumbar herniated disc. J Chin Med Assoc. 2009. 72: 650-3
3. Cribb GL, Jaffray DC, Cassar-Pullicino VN. Observations on the natural history of massive lumbar disc herniation. J Bone Joint Surg Br. 2007. 89: 782-4
4. Gardner A, Gardner E, Morley T. Cauda equina syndrome: A review of the current clinical and medico-legal position. Eur Spine J. 2011. 20: 690-7
5. Guinto FC, Hashim H, Stumer M. CT demonstration of disk regression after conservative therapy. AJNR Am J Neuroradiol. 1984. 5: 632-3
6. Hong SJ, Kim DY, Kim H, Kim S, Shin KM, Kang SS. Resorption of massive lumbar disc herniation on MRI treated with epidural steroid injection: A retrospective study of 28 cases. Pain Physician. 2016. 19: 381-8
7. Jeon CH, Chung NS, Son KH, Lee HS. Massive lumbar disc herniation with complete dural sac stenosis. Indian J Orthop. 2013. 47: 244-9
8. Jung YJ, Shin JS, Lee J, Lee YJ, Kim MR, Ha IH. Delayed spontaneous resorption of lumbar intervertebral disc herniation: A case report. Altern Ther Health Med. 2017. 23: 58-63
9. Long B, Koyfman A, Gottlieb M. Evaluation and management of cauda equina syndrome in the emergency department. Am J Emerg Med. 2020. 38: 143-8
10. Ying EC, Shetty A, Craig PR, Chitgopkar SD. An observation of massive lumbar disc prolapses. J Spine Surg. 2018. 4: 583-7










Firmansyah Purwanto
Posted October 2, 2021, 10:12 am
Interesting case. But the article didn’t go any details of what ” weekly clinical examinations” entails. Is there any conservative treatment other than medication? Thanks
Dinesh Naidoo
Posted November 6, 2021, 11:32 pm
The weekly clinical examinations were done to exclude any neurological deterioration that was not self reported.
Conservative trea