- Department of Neurosurgery Neurological Institute of Thailand, BKK, Thailand
- Department of Neuroradiology, Neurological Institute of Thailand, BKK, Thailand
- Department of Radiology, Bumrungrad Hospital, BKK, Thailand
Correspondence Address:
Prasert Iampreechakul, Department of Neurosurgery, Neurological Institute of Thailand, BKK, Thailand.
DOI:10.25259/SNI_1113_2024
Copyright: © 2025 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Prasert Iampreechakul1, Korrapakc Wangtanaphat1, Wuttipong Tirakotai1, Yodkhwan Wattanasen2, Punjama Lertbutsayanukul2, Sunisa Hangsapruek2, Somkiet Siriwimonmas3. Spontaneous obliteration of a greater sphenoid wing dural arteriovenous fistula involving the diploic venous system. 21-Mar-2025;16:99
How to cite this URL: Prasert Iampreechakul1, Korrapakc Wangtanaphat1, Wuttipong Tirakotai1, Yodkhwan Wattanasen2, Punjama Lertbutsayanukul2, Sunisa Hangsapruek2, Somkiet Siriwimonmas3. Spontaneous obliteration of a greater sphenoid wing dural arteriovenous fistula involving the diploic venous system. 21-Mar-2025;16:99. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13447
Abstract
BackgroundSphenoid wing dural arteriovenous fistulas (DAVFs) are rare vascular anomalies caused by abnormal arteriovenous shunting near the sphenoid bone. They are associated with significant risks, including cortical venous reflux and intracranial hemorrhage, especially when involving high-risk drainage pathways. Spontaneous regression of high-flow sphenoid wing DAVFs is exceedingly rare and has not been previously documented.
Case DescriptionWe report a 59-year-old woman with a history of head trauma who presented with progressive right eye proptosis, redness, blurred vision, and tinnitus over 5 months. Imaging revealed a high-flow sphenoid wing DAVF with drainage into the diploic venous system, superficial middle cerebral vein, and basal vein of Rosenthal. Angiography demonstrated venous outlet stenosis and preexisting thrombosis in the superior ophthalmic vein. While the patient was being prepared for endovascular treatment, follow-up imaging 6 months later confirmed spontaneous obliteration of the fistula, accompanied by complete resolution of symptoms.
ConclusionThis case highlights the unique occurrence of spontaneous regression in a high-flow sphenoid wing DAVF. The obliteration was likely facilitated by venous outlet stenosis, preexisting thrombosis, and the hemodynamic effects of contrast media during angiography. These findings emphasize the importance of careful monitoring and follow-up in the management of DAVFs, as spontaneous resolution, although rare, may occur.
Keywords: Diploic venous system, Dural arteriovenous fistula, Sphenoid wing, Spontaneous obliteration, Superior ophthalmic vein thrombosis, Venous outlet stenosis
INTRODUCTION
Dural arteriovenous fistulas (DAVFs) of the sphenoid wing are exceedingly rare vascular anomalies, accounting for approximately 1% of all intracranial DAVFs.[
To the best of our knowledge, spontaneous obliteration of greater sphenoid wing DAVFs has not been previously reported in the literature.[
CASE PRESENTATION
A 59-year-old woman with a medical history of hypertension and dyslipidemia presented to a local hospital with a 5-month history of right eye redness, proptosis, and blurred vision. She also reported tinnitus in her right ear. Seven months prior, she had fallen while chasing a dog, striking her head on the floor, but without loss of consciousness. A computed tomography (CT) scan of the brain showed an enlarged right superior ophthalmic vein and a prominent cavernous sinus (CS) [
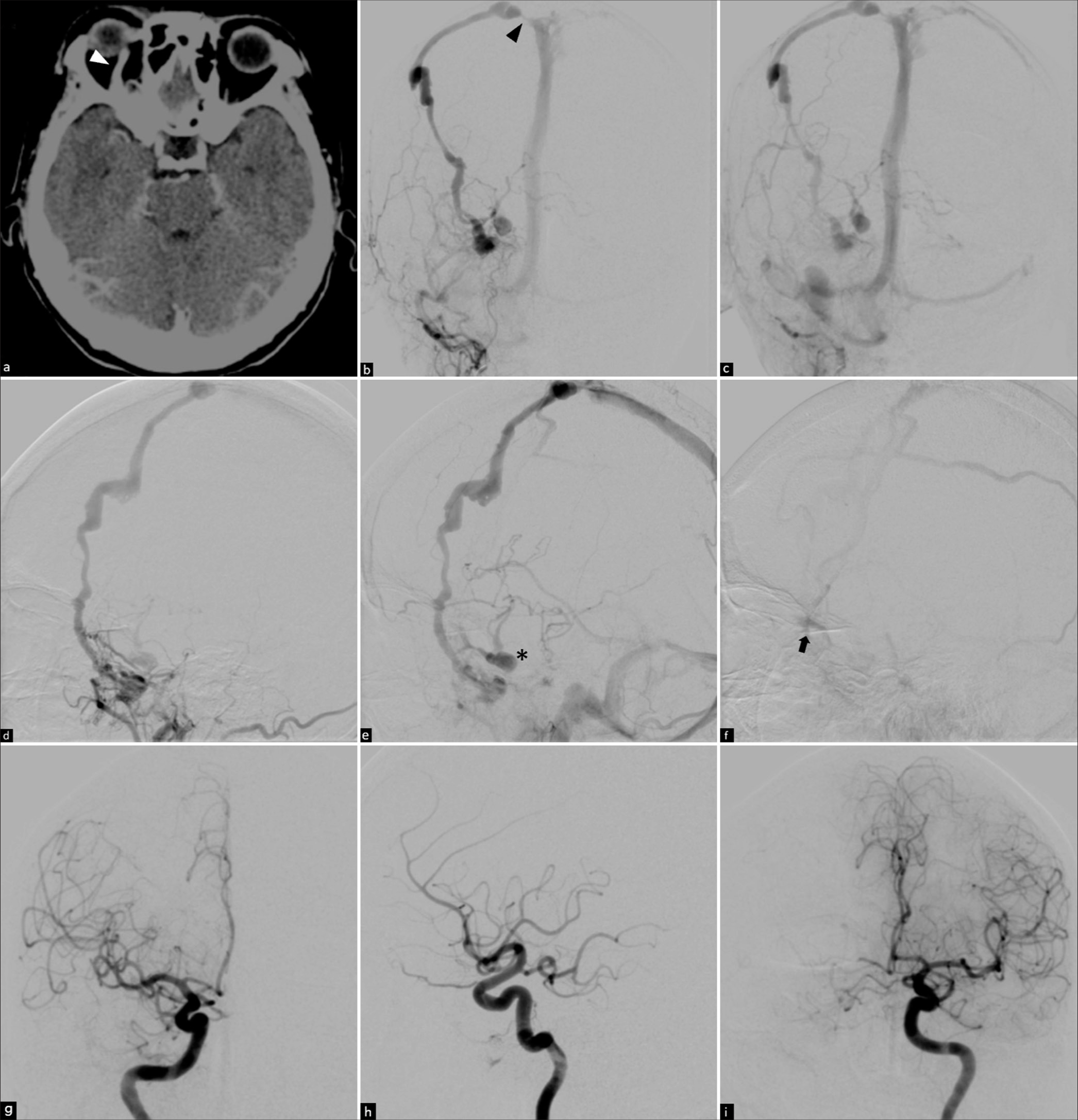
Figure 1:
(a) Axial contrast-enhanced computed tomography (CT) scan of the brain obtained 5 months after the onset of symptoms demonstrates mild right-sided proptosis and an enlarged right superior ophthalmic vein (white arrowhead). (b and c) Anteroposterior (AP) and (d-f) lateral views of the right external carotid artery angiography, from the arterial to venous phases, performed 7 months after symptom onset, reveal a right greater sphenoid wing dural arteriovenous fistula. The fistula is supplied by the right ascending pharyngeal artery, the middle meningeal artery, and the sphenopalatine branches of the internal maxillary artery. Venous drainage occurs through the dilated diploic vein of the greater sphenoid wing, subsequently into the engorged frontal diploic vein, and finally into the superior sagittal sinus. Notably, venous outlet stenosis is observed (black arrowhead). In addition, an alternative drainage route is identified through the bridging vein into the right cavernous sinus (asterisk), which further drains into the right deep middle cerebral veins and the right basal vein of Rosenthal through the uncal vein. This pathway extends to the contralateral basal vein of Rosenthal through the peduncular vein. The arrow indicates venous stasis in the right superior ophthalmic vein in the late venous phase. (g and h) AP and lateral views of the right internal carotid artery (ICA), and (i) AP view of the left ICA show minute branches from bilateral meningohypophyseal trunks contributing to the fistula’s vascular supply.
On ophthalmic examination, the right eye showed proptosis and dilated episcleral veins. Visual acuity was 20/40 in the right eye and did not improve with pinhole correction; in the left eye, visual acuity was 20/80 without correction and 20/32 with pinhole correction. Funduscopic examination revealed congested and tortuous vessels with venous stasis retinopathy in the left eye. Intraocular pressure (IOP) was 21.5 mmHg in the right eye and 9.8 mmHg in the left eye. The patient was diagnosed with secondary glaucoma in the right eye and started on 0.5% timolol maleate eye drops, to be administered twice daily.
Cerebral angiography confirmed a DAVF at the right greater sphenoid wing, supplied by the right ascending pharyngeal artery, the middle meningeal artery, and sphenopalatine branches of the internal maxillary artery, as well as tiny branches from bilateral meningohypophyseal trunks. Venous drainage occurred through the dilated diploic vein of the greater sphenoid wing, subsequently into the engorged frontal diploic vein, and finally into the superior sagittal sinus. A narrowing of the connecting pathway between the engorged diploic vein and the superior sagittal sinus was observed. An alternative drainage route was noted through the bridging vein into the right CS, which further drained into the right deep middle cerebral vein (DMCV) and the right basal vein of Rosenthal through the uncal vein. This venous pathway extended contralaterally into the basal vein of Rosenthal through the peduncular vein, consistent with the angioarchitectural features of a Cognard type IIa+b DAVF. Venous stasis in the right superior ophthalmic vein (SOV) was noted during the late venous phase [
Figure 2:
(a-c) Axial, (d and e) coronal, and (f) sagittal maximum intensity projection reformatted sequential images from angiographic computed tomography of the right external carotid artery (ECA) angiography demonstrate a dural arteriovenous fistula at the right greater sphenoid wing bone. The fistula drains into a large, dilated frontal diploic vein and additionally into the right cavernous sinus through a bridging vein (arrowhead). Further venous drainage is observed into the ipsilateral deep middle cerebral veins and the basal vein of Rosenthal through the uncal vein (arrow), with subsequent drainage into the contralateral basal vein of Rosenthal through the peduncular vein (curved arrow). (g) A lateral 3D reconstruction of the right ECA highlights a narrowed connecting pathway (asterisk) between the engorged diploic vein and the superior sagittal sinus. (h and i) Anteroposterior and lateral views of the right external carotid artery obtained 6 months after the initial angiography confirm complete obliteration of the fistula.
The patient was thoroughly counseled on the risks and benefits of treatment, provided informed consent, and scheduled for endovascular intervention the following week. However, due to the COVID-19 pandemic, the procedure was postponed. Over the subsequent 6 months, the patient initially experienced persistent proptosis, conjunctival injection, and intermittent blurred vision. Gradually, these symptoms improved, with a noticeable reduction in conjunctival congestion and complete resolution of proptosis.
Six months later, the patient was re-evaluated and prepared for endovascular treatment under general anesthesia. Remarkably, repeat angiography at that time demonstrated spontaneous complete obliteration of the fistula [
At the 2-year follow-up, the patient remained completely asymptomatic, with no signs of proptosis, conjunctival congestion, or diplopia. Ophthalmic examination at that time showed further normalization of IOP, measuring 9.4 mmHg in the right eye and 8.6 mmHg in the left eye.
DISCUSSION
The sphenoid bone, a central component of the cranial base, is a complex structure that contributes to the formation of the orbit, cranial cavity, and several foramina for neurovascular passage. It consists of a central body, greater and lesser wings, and pterygoid processes. The greater wings extend laterally to form part of the middle cranial fossa and orbital walls, while the lesser wings create the posterior boundary of the anterior cranial fossa and part of the superior orbital fissure.[
Greater sphenoid wing DAVFs often exhibit aggressive features, with shunts typically located near the foramina (e.g., foramen ovale or rotundum) and venous drainage involving the superficial middle cerebral vein (SMCV), a basal vein of Rosenthal, or sphenobasal vein. These lesions are commonly associated with cortical venous reflux and venous varices, increasing the risk of hemorrhagic complications. In contrast, lesser sphenoid wing DAVFs often drain into the CS, resembling CS DAVFs with fewer cases of cortical venous reflux. Despite their less aggressive nature, exceptions exist where direct drainage into deep veins can result in significant complications, such as venous infarction or intracranial hemorrhage.[
Greater sphenoid wing DAVFs are often associated with symptoms related to their venous drainage patterns and the presence of cortical venous reflux. Common presentations include ocular symptoms such as proptosis, chemosis, diplopia, and visual disturbances due to venous congestion in the orbital region. Patients may also experience retro-orbital pain, headaches, or pulsatile tinnitus, particularly when the venous drainage involves the CS or SMCV. In more aggressive cases, cortical venous reflux increases the risk of intracranial hemorrhage, leading to neurological deficits or acute hemorrhagic presentations. The involvement of deep venous structures, such as the basal vein of Rosenthal, can further exacerbate symptoms, emphasizing the importance of early detection and management.[
The management of greater sphenoid wing DAVFs requires a multidisciplinary approach to achieve optimal outcomes. Advances in endovascular techniques and hybrid surgical strategies have significantly improved the curative potential for these rare and complex lesions.[
In this study, the development of a greater sphenoid wing DAVF was likely precipitated by a history of head trauma. The patient presented with ocular symptoms, including proptosis and redness, which were directly attributed to venous congestion involving the CS and SOV. These symptoms prompted the patient to seek medical attention. This case is further distinguished by the unusual venous drainage pattern of the fistula, which prominently involved the diploic venous system. The primary drainage pathway included dilated diploic veins of the sphenoid bone, extending into the engorged frontal diploic vein and ultimately draining into the superior sagittal sinus. In addition, the fistula drained into the DMCV and basal vein of Rosenthal, increasing the risk of cortical venous reflux, venous congestion, and intracranial hemorrhage, making it a high-risk lesion.
In our case, the spontaneous closure of the greater sphenoid wing DAVF involving the diploic venous system appears to be associated with several contributing factors, including preexisting thrombosis in the SOV, venous outlet stenosis, and the potential role of contrast media from prior angiographic study.
The preexisting thrombosis observed in the SOV during angiography suggests that venous stasis had already initiated thrombosis, setting the stage for spontaneous closure. Venous stasis, often caused by impaired venous outflow, is a critical factor in thrombus formation within the draining veins of high-flow fistulas.[
These factors collectively underscore the complex interplay of hemodynamic and anatomical mechanisms underlying the rare phenomenon of spontaneous fistula closure. While this outcome is favorable, it remains unpredictable, highlighting the need for close monitoring and readiness for intervention to address potential complications or recurrence.
CONCLUSION
This case underscores the rare and unique phenomenon of spontaneous regression of a high-flow sphenoid wing DAVF, a condition not previously reported in the literature. The spontaneous obliteration observed in our patient was likely facilitated by a combination of preexisting thrombosis in the SOV, venous outlet stenosis, and the potential hemodynamic effects of contrast media used during angiography. Although spontaneous regression is uncommon, this case highlights the importance of careful monitoring, timely follow-up imaging, and individualized management to avoid unnecessary interventions and ensure optimal patient outcomes.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Akioka N, Kuwayama N, Kuroda S. Sphenoid wing dural arteriovenous fistulas. J Neuroendovasc Ther. 2023. 19: 1-11
2. Cochinski R, Agarwal M, Albuquerque J, De Almeida CA, Stricker RP, Uberti MF. Anatomy and diseases of the greater wings of the sphenoid bone. Radiographics. 2022. 42: 1177-95
3. Duangprasert G, Durongkaweroj P, Chotsakulthong P, Tantongtip D. Combined open surgery and endovascular embolization for a ruptured sphenoid wing dural arteriovenous fistula. Acta Neurochir (Wien). 2024. 166: 333
4. Ghali MG. Sphenoid dural arteriovenous fistulas. Neurosurg Rev. 2021. 44: 77-96
5. Iampreechakul P, Siriwimonmas S. Spontaneous obliteration of spontaneous vertebral arteriovenous fistula associated with fibromuscular dysplasia after partial surgery: A case report. Interv Neuroradiol. 2016. 22: 717-27
6. Iampreechakul P, Tirakotai W, Tanpun A, Wattanasen Y, Lertbusayanukul P, Siriwimonmas S. Spontaneous resolution of direct carotid-cavernous fistulas: Case series and literature review. Interv Neuroradiol. 2019. 25: 71-89
7. Kadono Y, Maeno K. Transvenous embolization of a Borden III middle cranial fossa dural arteriovenous fistula through the vein of Trolard and superficial middle cerebral vein: A technical case report. Radiol Case Rep. 2024. 19: 5399-403
8. Misaki K, Uchiyama N, Mohri M, Aida Y, Uno T, Nakada M. Unique venous drainage of a sphenoid wing dural arteriovenous fistula with ocular symptoms. World Neurosurg. 2017. 97: 753.e1-5
9. Osbun JW, Kim LJ, Spetzler RF, McDougall CG. Aberrant venous drainage pattern in a medial sphenoid wing dural arteriovenous fistula: A case report and review of the literature. World Neurosurg. 2013. 80: e381-6
10. Ritchie WG, Lynch PR, Stewart GJ. The effect of contrast media on normal and inflamed canine veins. A scanning and transmission electron microscopic study. Invest Radiol. 1974. 9: 444-55
11. Shimizu Y, Tokuda K, Park C. Sphenoid wing dural arteriovenous fistula: A case report and literature review. Surg Neurol Int. 2020. 11: 438
12. Shi ZS, Ziegler J, Feng L, Gonzalez NR, Tateshima S, Jahan R. Middle cranial fossa sphenoidal region dural arteriovenous fistulas: Anatomic and treatment considerations. AJNR Am J Neuroradiol. 2013. 34: 373-80
13. Watanabe J, Maruya J, Nishimaki K. Surgical treatment of a dural arteriovenous fistula in the sphenoid wing with a unique drainage pattern through the basal vein of Rosenthal. NMC Case Rep J. 2015. 2: 88-92
14. Yu J. Endovascular treatment for sphenoidal region dural arteriovenous fistula. Front Neurol. 2024. 15: 1348178