- Department of Neurosurgery, Japan Community Health care Organization Kobe Central Hospital, Kobe, Hyogo, Japan.
Correspondence Address:
Takuma Aoki, Department of Neurosurgery, Japan Community Health care Organization Kobe Central Hospital, Kobe, Hyogo, Japan.
DOI:10.25259/SNI_842_2023
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Takuma Aoki, Yuichi Furuno, Keisuke Fuji, Kazuyuki Kuwayama, Keigo Matsumoto. Successful endonasal transsphenoidal surgery to treat acute internal carotid artery occlusion caused by pituitary apoplexy: Usefulness of arterial spin labeling imaging for emergency decision. 31-May-2024;15:176
How to cite this URL: Takuma Aoki, Yuichi Furuno, Keisuke Fuji, Kazuyuki Kuwayama, Keigo Matsumoto. Successful endonasal transsphenoidal surgery to treat acute internal carotid artery occlusion caused by pituitary apoplexy: Usefulness of arterial spin labeling imaging for emergency decision. 31-May-2024;15:176. Available from: https://surgicalneurologyint.com/surgicalint-articles/12923/
Abstract
Background: Pituitary apoplexy (PA) is a rare clinical condition presenting with acute headache, visual disturbance, and disorientation. PA can cause strokes due to acute internal cervical artery occlusion (ICO), which is an extremely rare condition. Arterial spin labeling (ASL) on magnetic resonance imaging (MRI) is a popular technique, which is a quantitative perfusion imaging useful for the diagnosis of ischemia. We report a treatment with acute pseudo-ICO in which ASL on MRI was useful for the decision of surgery timing.
Case Description: A 50-year-old male presented with a sudden headache and nausea. MRI and magnetic resonance angiography revealed a large pituitary tumor and left ICO. However, the left middle cerebral and anterior cerebral arteries were depicted due to a cross-flow through the anterior communicating artery. ASL on MRI showed decreased perfusion of the left hemisphere, suggesting acute ICO. As he had no neurological deficit, we treated him conservatively, following the guidelines. Two days after admission, he presented with sensory aphasia and incomplete right paralysis. Emergency head computed tomography revealed a low-density area in his left temporal lobe. We decided on emergency tumor decompression surgery to prevent ischemic progression. We performed endonasal transsphenoidal surgery. Postoperative MRI showed recanalization of the left internal carotid artery (ICA). His incomplete right paralysis improved immediately after surgery but remains mild sensory aphasia.
Conclusion: ICO-related PA is a very rare occasion but there are few similar reports. Some cases of successful ICO treatment due to PA have been reported, but the question of whether emergency or elective surgery is better remains unanswered. Our case may have been no neurological deficit if we had decided to have surgery on admission. Hypoperfusion of the ICA area due to PA may be an adaptation of emergency surgery. Perfusion images like ASL could be a useful technique to decide on surgery or conservative treatment.
Keywords: Arterial spin labeling, Endonasal transsphenoidal surgery, Internal carotid artery occlusion, Pituitary apoplexy
INTRODUCTION
Pituitary apoplexy (PA) is a rare clinical condition presenting with acute headache, visual disturbance, and disorientation. Emergency surgery for PA with visual disturbance and deteriorating consciousness can improve neurological dysfunction.[
PA can cause strokes due to acute internal cervical artery occlusion (ICO), which is an extremely rare condition. However, although emergency surgery might prevent stroke progression due to acute ICO, the appropriate timing of surgery is still unclear. The diagnosis of acute or chronic obstruction is difficult without suggestive symptoms and is important for indicating emergency surgery.
Arterial spin labeling (ASL) on magnetic resonance imaging (MRI) is a popular and prominent technique, which is a quantitative perfusion imaging useful for the diagnosis of ischemia. Herein, we report a treatment with acute pseudo-ICO in which ASL on MRI was useful for the decision of surgery timing.
CASE DESCRIPTION
A 50-year-old male presented with a sudden headache and nausea from the past day. He had a history of asthma, hypertension, and sinusitis. His Glasgow Coma Scale (GCS) was 15 (E4V5M6). There were no neurological deficits, including visual disturbance or hemiparesis. He was started on oral betamethasone 1 week before to treat his sinusitis.
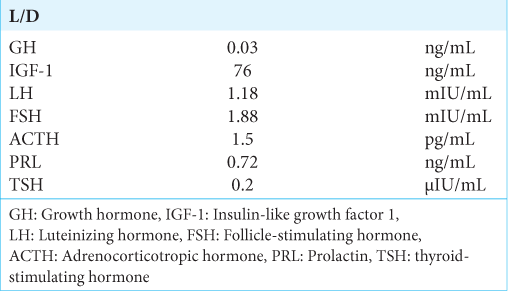
Routine blood tests revealed an elevated white blood cell count. Endocrinological blood tests showed low secretion of thyroid-stimulating hormone, adrenocorticotropic hormone, and follicle-stimulating hormone (FSH) [
Figure 1:
(a) Head computed tomography, (b) diffusion-weighted imaging and (c) T2*-weighted image revealed an enlarged pituitary fossa and suggested pituitary apoplexy. Contrasted magnetic resonance imaging (d: coronal, e: sagittal) showed mass lesions without enhancement. (f) There had been no infarction on admission .
As he had no neurological deficit, we treated him conservatively with intravenous hydration and hydrocortisone infusion. Two days after admission, he presented with sudden disorientation, a GCS of 12 (E3V4M5), sensory aphasia, and incomplete right paralysis.
Emergency head CT revealed a low-density area in his left temporal lobe [
Under general anesthesia, we performed endonasal transsphenoidal surgery. After the dura incision, a white tumor erupted, reflecting high intrasellar pressure (ISP).
Pathological findings showed a paucity of FSH-positive cells with immunostaining among many unstained cells. Based on pathological and physical findings, we diagnosed him with a nonfunctional adenoma.
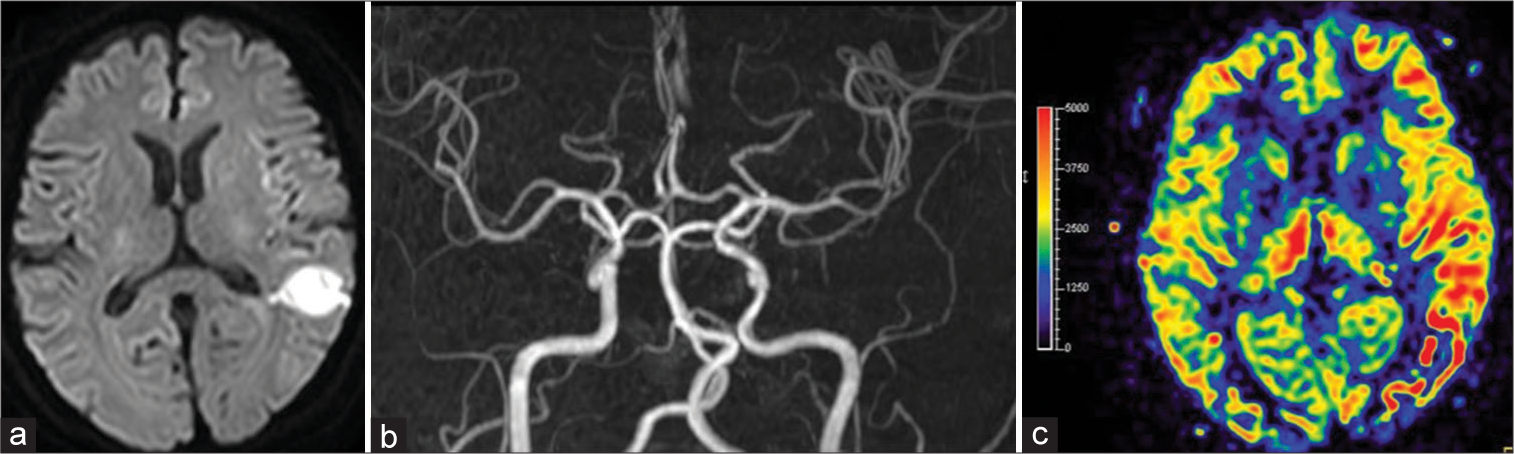
Postoperative MRI showed recanalization of the left ICA and no fresh cerebral infarction except for a known temporal lobe stroke [
Figure 4:
(a) Postoperative head magnetic resonance imaging showed the known ischemic stroke of the left temporal lobe but no newly high-intensity area. (b) Head magnetic resonance angiography revealed recanalization of the left internal carotid artery, and (c) arterial spin labelingshowed improvement of hypoperfusion of the left hemisphere.
DISCUSSION
PA is a rare clinical condition, representing about 1.6–4.8% of all pituitary adenomas, and many cases present with severe headache, disorientation, and visual disturbances.[
PA-induced ICO is a rare clinical condition. There have been a few similar reports in the past.[
However, similar to mechanical thrombectomy, preventing ischemic stroke in a rare condition of major artery occlusion is important since the ISP decompression surgery can lead to ICA recanalization. Some cases of successful ICO treatment due to PA have been reported, but the question of whether emergency or elective surgery is better remains unanswered.
PA progression can invade ICA and cavernous sinus, leading to chronic ICO. When a low-perfusion area progresses to an ischemic stroke, emergency ISP decompression surgery to recanalize ICA is ineffective, leading to a large hemorrhagic infarction. Based on emergency management of PA in adult patients, emergency surgery will not be indicated in patients without focal neurological deficits, and conservative treatment, such as steroid injection, will be prioritized.
ASL is a prominent technique of MRI that can produce quantitative brain perfusion images without tracer injection. The tracer is the blood water itself created by inverting magnetization with a train of radiofrequency pulses. Thus, the ASL technique is useful to detect ischemic stroke by finding differences between DWI and ASL.[
In terms of preventing stroke, perfusion imaging can be useful in deciding whether elective or emergency surgery should be performed, especially for ASL, to prevent the progression of ischemic stroke.
In our case, the patient had no focal neurological defects on admission, but ASL of the left hemisphere showed low perfusion. As a result, he was diagnosed with ischemic stroke of the temporal lobe. Therefore, the stroke could have been prevented if the decision of surgery had been made earlier due to his ischemic intolerance. In such cases of PA with ICO showing low perfusion in ASL but no high intensity in DWI, emergency surgery for PA should be considered to prevent ischemic stroke.
CONCLUSION
We reported a case of successful treatment of ischemic stroke caused by ICO due to PA. Due to high ISP, PA could lead to ischemic stroke, such as major artery occlusion. For cases of ischemic intolerance, emergency ISP decompression surgery can prevent stroke progression and lead to a better prognosis. Perfusion imaging, like ASL on MRI is a useful imaging test to decide a strategy to treat such complicated conditions. Low perfusion indicated an urgent risk of ischemic stroke, which may warrant emergency surgery.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Ahn JM, Oh HJ, Oh JS, Yoon SM. Pituitary apoplexy causing acute ischemic stroke: Which treatment should be given priority. Surg Neurol Int. 2020. 11: 113
2. Baldeweg SE, Vanderpump M, Drake W, Reddy N, Markey A, Plant GT. Society for endocrinology endocrine emergency guidance: Emergency management of pituitary apoplexy in adult patients. Endocr Connect. 2016. 5: G12-5
3. Chokyu I, Tsuyuguchi N, Goto T, Chokyu K, Chokyu M, Ohata K. Pituitary apoplexy causing internal carotid artery occlusion--case report. Neurol Med Chir (Tokyo). 2011. 51: 48-51
4. Dogan S, Kocaeli H, Abas F, Korfali E. Pituitary apoplexy as a cause of internal carotid artery occlusion. J Clin Neurosci. 2008. 15: 480-3
5. Dubuisson AS, Beckers A, Stevenaert A. Classical pituitary tumour apoplexy: Clinical features, management and outcomes in a series of 24 patients. Clin Neurol Neurosurg. 2007. 109: 63-70
6. Haller S, Zaharchuk G, Thomas DL, Lovblad KO, Barkhof F, Golay X. Arterial spin labeling perfusion of the brain: Emerging clinical applications. Radiology. 2016. 281: 337-56
7. Hashimoto G, Wada S, Yoshino F, Kuwashiro T, Yasaka M, Okada Y. Case report: transient ischemic stroke caused by internal carotid artery occlusion due to compression by pituitary apoplexy and hemodynamic mechanism. Rinsho Shinkeigaku. 2020. 60: 146-51
8. Kruse A, Astrup J, Cold GE, Hansen HH. Pressure and blood flow in pituitary adenomas measured during transsphenoidal surgery. Br J Neurosurg. 1992. 6: 333-41
9. Nagure PV, Nikam VR, Garud AS. Pituitary apoplexy producing internal carotid and basilar artery compression: A rare case report. Asian J Neurosurg. 2018. 13: 1264-8
10. Yang SH, Lee KS, Lee KY, Lee SW, Hong YK. Pituitary apoplexy producing internal carotid artery compression: A case report. J Korean Med Sci. 2008. 23: 1113-7
11. Zhu X, Wang Y, Zhao X, Jiang C, Zhang Q, Jiang W. Incidence of pituitary apoplexy and its risk factors in Chinese people: A database study of patients with pituitary adenoma. PLoS One. 2015. 10: e0139088