- Departments of Radiology San Antonio Uniformed Services Health Education Consortium, JBSA Ft. Sam Houston, Texas, United States of America.
- Departments of Neurosurgery, San Antonio Uniformed Services Health Education Consortium, JBSA Ft. Sam Houston, Texas, United States of America.
Correspondence Address:
Jordan R. Davis
Departments of Radiology San Antonio Uniformed Services Health Education Consortium, JBSA Ft. Sam Houston, Texas, United States of America.
DOI:10.25259/SNI_419_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Jordan R. Davis1, Matthew L. Kluckman1, Grant W. Mallory2, John L. Ritter1. Successful non-operative management for atlanto-occipital dislocation resulting in spinal cord contusion in a patient with atlanto-occipital assimilation and severe Chiari I malformation. 15-Oct-2020;11:338
How to cite this URL: Jordan R. Davis1, Matthew L. Kluckman1, Grant W. Mallory2, John L. Ritter1. Successful non-operative management for atlanto-occipital dislocation resulting in spinal cord contusion in a patient with atlanto-occipital assimilation and severe Chiari I malformation. 15-Oct-2020;11:338. Available from: https://surgicalneurologyint.com/surgicalint-articles/10325/
Abstract
Background: Atlanto-occipital dislocation (AOD) is a rare, highly morbid, and highly lethal injury that results from high-energy trauma and almost universally requires operative management for satisfactory outcomes. It can be difficult to identify the severity of injury at the time of presentation, and when diagnosis is delayed outcomes worsen significantly. Anatomic anomalies of the craniovertebral junction may further complicate its detection. When such anomalies are present either singly or in combination, they are known to cause space constraints which may increase the likelihood of spinal cord injury. Given that such anomalies and AOD are rare, few examples of patients with both are reported in the literature. Furthermore, it is not clear in what way patient management may be impacted in this context.
Case Description: We will present a unique case of an 18-year-old patient with traumatic AOD and an intact neurologic examination who was found to have atlanto-occipital assimilation (AOA), platybasia, basilar invagination, and severe Chiari I malformation, who was treated effectively with non-operative management.
Conclusion: Our case demonstrates the successful application of a non-operative treatment strategy in a carefully selected patient with AOD in the context of AOA.
Keywords: Atlanto-occipital dislocation, Atlanto-occipital assimilation, Chiari I malformation, Cervical spine trauma
INTRODUCTION
Atlanto-occipital dislocation (AOD) is a rare injury with high morbidity and mortality which typically occurs as a result of high-energy blunt trauma, particularly in cases of motor vehicle collisions.[
CASE DESCRIPTION
An 18-year-old man presented to our institution via ambulance after a high-speed motor vehicle collision. Paramedics noted a prolonged extrication. He had loss of consciousness at the scene with retrograde amnesia but scored a 15 on the Glasgow Coma Scale (GCS). He arrived at our hospital with stable vital signs and continued to score a 15 on the GCS. He complained of lower neck and left hip pain. He had lower neck tenderness to palpation, but had a normal neurologic evaluation to include full strength and sensation in the extremities and preserved cranial nerve function.
Imaging
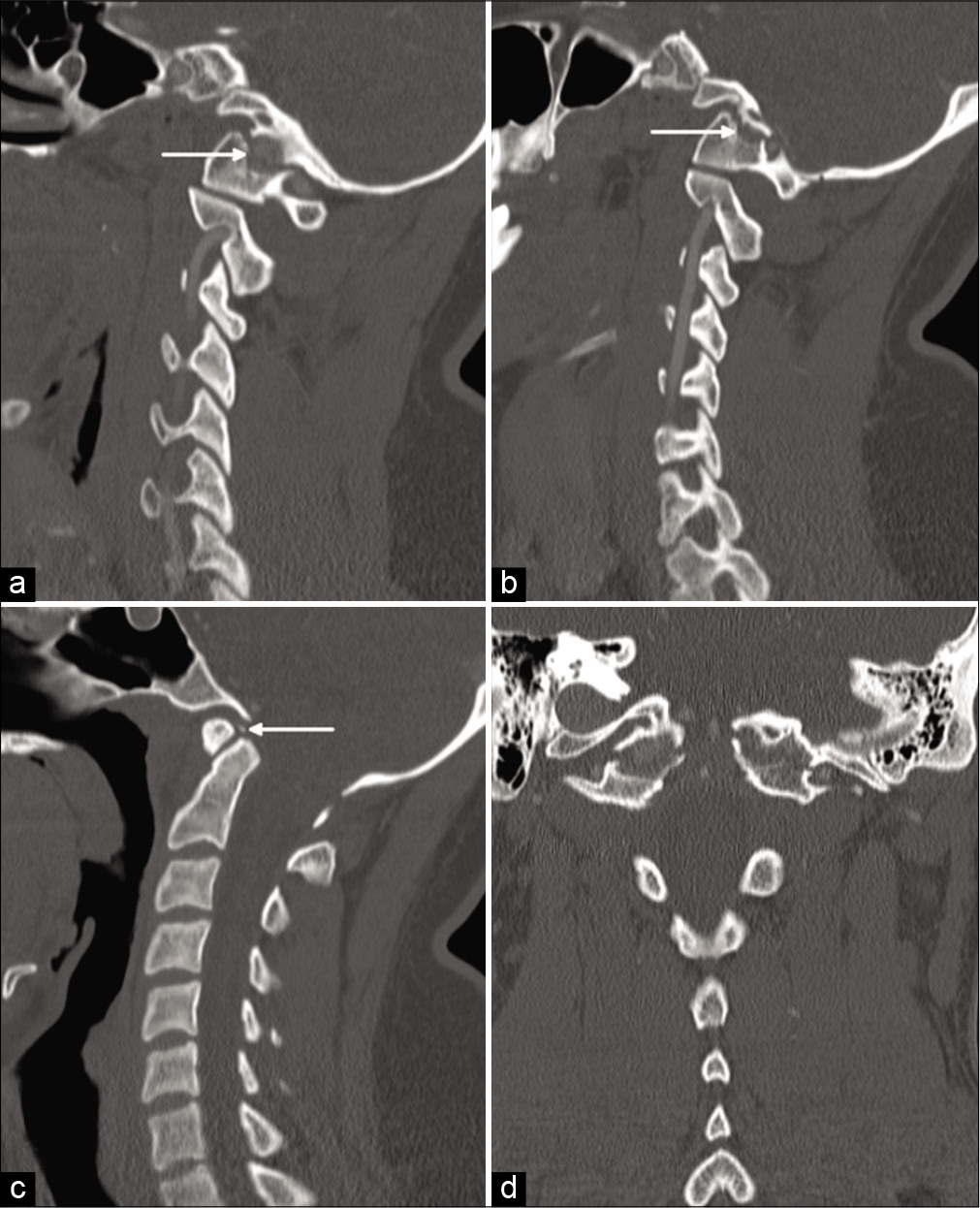
CT of his chest and body revealed an isolated grade two splenic laceration per the American Association for the Surgery of Trauma (AAST) guidelines. Computed tomography (CT) of the head demonstrated no traumatic injury. CT of the cervical spine [
Figure 1:
Computed tomography (CT) of the cervical spine in right (a) and left (b) parasagittal planes demonstrates partial atlanto-occipital assimilation (AOA), with bilateral fractures causing up to 3 mm of distraction at the craniovertebral junction (arrows). Note that fracture involves the rudimentary left foramen transversarium; no evidence for vascular injury was identified on CT angiography, not shown. A midsagittal plane (c) demonstrates a small avulsion fracture just superior to the odontoid process (arrow). Platybasia and basilar invagination are present. A C1 posterior fusion anomaly is also suggested, but better appreciated on axial images, not shown. The basion-dens interval is mildly widened, but the atlantodental interval is preserved. A coronal reconstruction (d) emphasizes the AOA with superimposed traumatic dissociation of the occiput from the cervical spine.
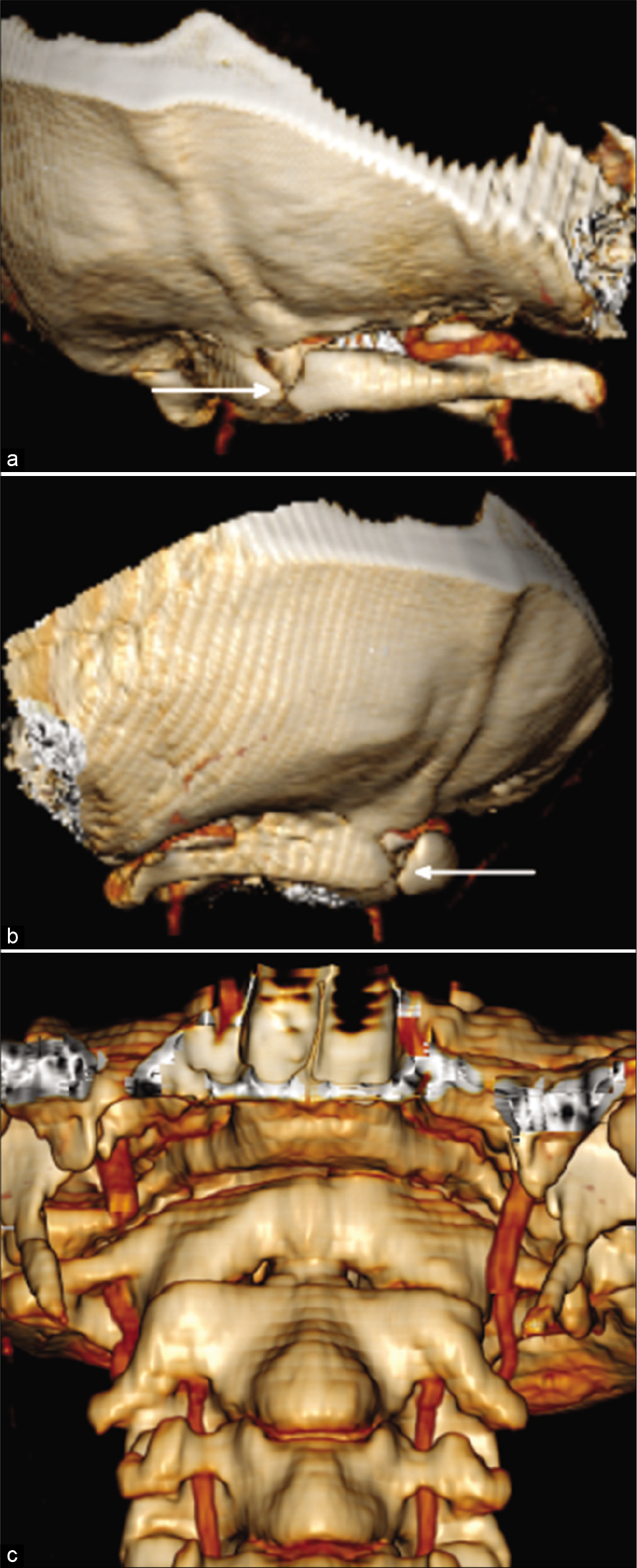
Figure 2:
Three-dimensional volume-rendered reconstructions of the skull base from right (a) and left (b) posterolateral views best show the variable fusion between C1 and the skull base, as well as incidental posterior fusion anomaly of C1 (arrows). Coronal three-dimensional volume-rendered reconstruction (c) shows the fractures en face, which can be mistaken for a normal atlanto-occipital joint.
MRI of the cervical spine [
Figure 3:
Mid-sagittal T1-weighted (a) and T2-weighted (b) magnetic resonance imaging of the cervical spine demonstrates discontinuity of the anterior atlanto-occipital membrane (horizontal white arrow) and apical ligament (diagonal white arrow), with associated edema and hematoma. The tectorial membrane is thinned, but intact (curved white arrow), and the transverse ligament (black arrow) is also intact. There is subtle signal hyperintensity in the spinal cord on the T2-weighted image (circle). The cerebellar tonsils are peg-like and extend up to 15 millimeters below the foramen magnum, resulting in inferior descent of the medulla and effacement of the spinal cord and thecal sac. A coronal T2 short-tau inversion recovery image (c) demonstrates intact alar ligaments (arrows), though due to the variant anatomy contiguity is difficult to appreciate on a single plane. An axial T2-weighted image at the level of C1–C2 (d) shows signal hyperintensity in the ventral left spinal cord, without signal hypointensity to indicate hemorrhage (circle). An axial T2-weighted image at the level of the foramen magnum (e) is notable for crowding of the foramen magnum due to inferior descent of the cerebellar tonsils related to Chiari I malformation, which compresses the brainstem and distorts its contour.
Treatment, hospital course, and post hospital follow-up
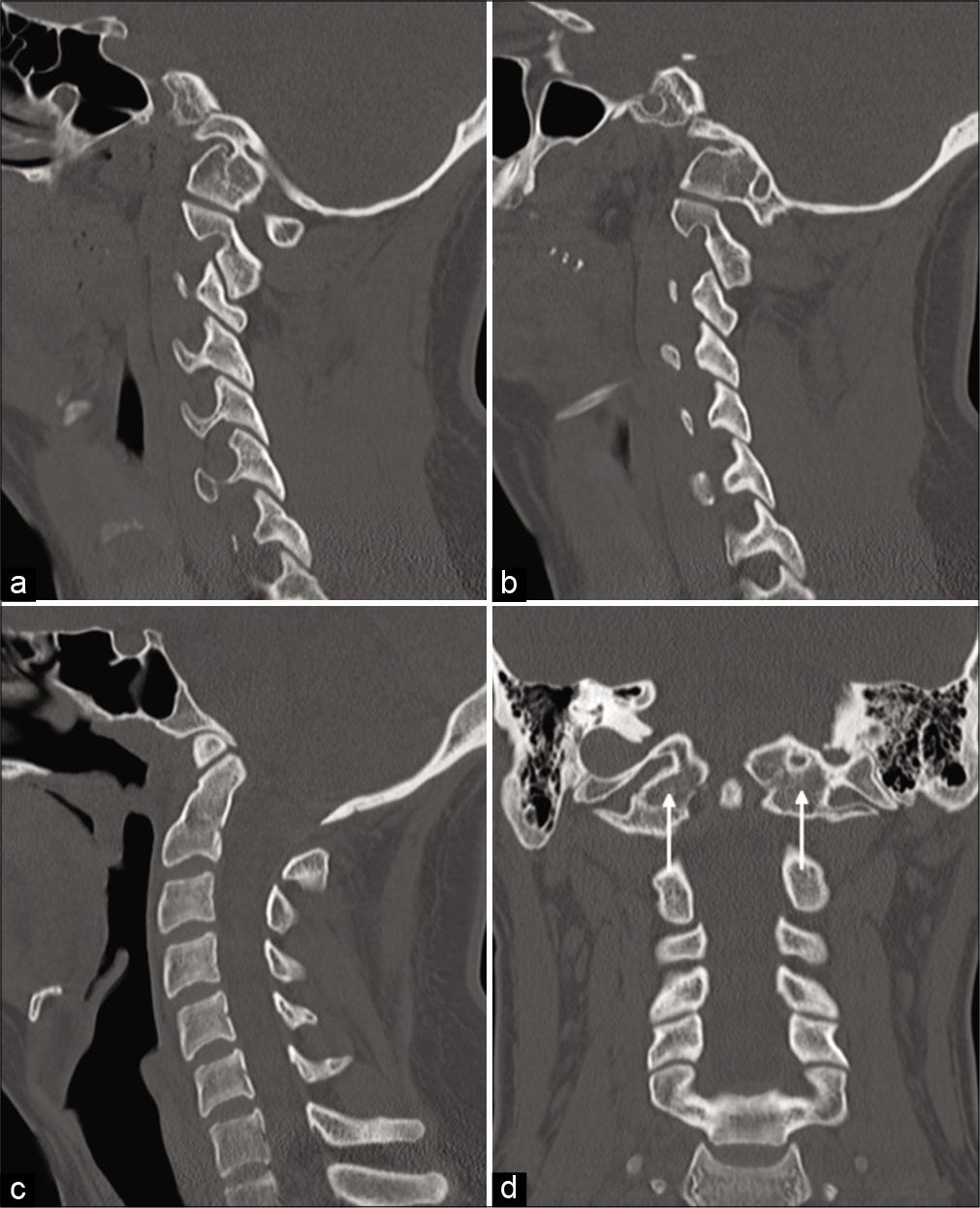
Because the tectorial membrane, transverse ligament, and alar ligaments were intact, and the patient had no neurologic deficits, surgical fixation was not performed. Instead, he was maintained in a hard cervical collar. He had an uncomplicated hospital stay and was discharged home two days later able to ambulate and accomplish his own activities of daily living. A follow-up CT of the cervical spine four weeks after injury [
Figure 4:
CT of the cervical spine four weeks after injury, in right (a) and left (b) parasagittal planes, demonstrates near-complete osseous bridging of the fractures. The midsagittal plane (c) reveals that the basion-dens interval has decreased, emphasizing the congenital basilar invagination in this patient. The previously identified avulsion fragment superior to the dens has also resolved. A coronal reconstruction (d) confirms near-complete resolution of injury, with subtle residual fracture lucencies (arrows).
DISCUSSION
AOD is rare in the hospital setting, historically accounting for up to 1% of cervical spine trauma treated in large level one trauma centers.[
AOD is characterized by failure of the CVJ osseous and/ or ligamentous structures in patients who sustain high-energy blunt trauma, often as a result of hyperflexion or hyperextension.[
AOD was historically diagnosed through lateral cervical spine radiographs, and the Powers’ ratio (basion-C1 posterior arch : opisthion-C1 anterior arch) was considered one of the first reliable radiographic criteria.[
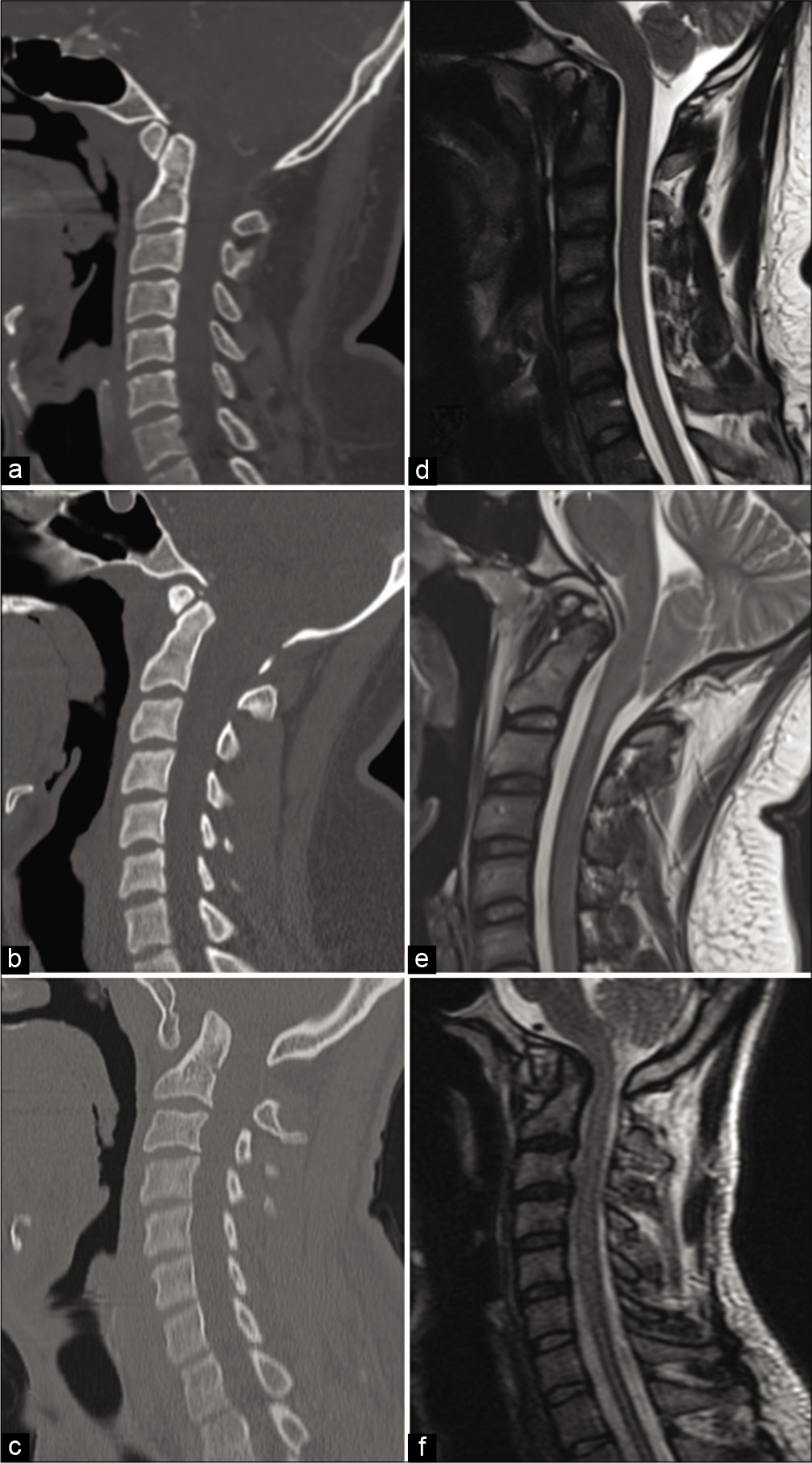
Figure 5:
Computed tomography and magnetic resonance imaging comparisons of a patient with atlanto-occipital assimilation (AOA) without traumatic injury (a and b), the patient presented in this case (c and d), and a different patient with AOA and atlanto-occipital dislocation presenting with widened atlanto-dental interval and a greater degree of post traumatic basilar invagination (e and f).
A large retrospective analysis[
Treatment for AOD almost universally requires surgical intervention, and the most common modern technique is occiput-C1 or occiput-C2 screw fixation. Patients with injuries at the lower levels may require fixation below the lowest injured level.[
AOD in patients with AOA is rarely reported.[
Optimal management in this subset of patients is not clearly defined due to the rarity of the condition. Our case is unique in the successful application of a non-operative management strategy. In a normal patient without AOA, the force of injury at the atlanto-occipital joint produces a ligamentous disruption resulting in joint dislocation. In our patient, and presumably in others with AOA, the force may preferentially cause fracture at the rigid CVJ, with a decreased degree of ligamentous injury. In contrast to a primarily ligamentous injury, a fracture has a greater physiological predisposition to healing. For this reason, we attempted nonoperative management and achieved success – seeing an almost complete return to baseline atlanto-occipital fusion four weeks from the time of injury. This would suggest that nonoperative management is possible in a patient with AOA and AOD primarily due to fracture. It is important to evaluate for the presence of neurologic deficits, as operative management is still probably indicated in such cases.
An important consideration in this patient, and all patients with cervical spine trauma, is the difficulty of initial detection of AOD, especially in a patient with AOA. As shown in [
CONCLUSION
AOD is rare but highly morbid and often lethal. It is increasingly prevalent in the hospital setting, possibly due to improved prehospital care, advancements in surgical techniques, and modern emergency department management. There are now numerous case studies describing patient survival, sometimes with minimal or no permanent neurologic deficits. These positive outcomes have typically required surgical fixation at the CVJ to maintain stability and avoid worsening neurologic injury. AOA, a similarly rare condition, can carry its own risk of pathology at the CVJ. In patients with AOA presenting with AOD, the complex anatomy could compound the significance of injury at the CVJ and confound diagnosis. We have presented such a patient treated successfully with non-operative management, and while there is insufficient literature to standardize the treatment of AOD in patients with AOA, the results of this case suggest the potential for healing in patients who are treated with nonoperative management who have purely osseous injuries and no displacement. Regardless of management strategy, we suggest a high index of suspicion in patients with high-energy trauma, and the clinician should not be fooled by the deceptive appearance of AOD in patients with AOA should such a patient present to the emergency department.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
The view(s) expressed herein are those of the author(s) and do not reflect the official policy or position of Brooke Army Medical Center, the U.S. Army Medical Department, the U.S. Army Office of the Surgeon General, the Department of the Army, the Department of the Air Force and Department of Defense, or the U.S. Government.
References
1. Bellabarba C, Mirza SK, West GA, Mann FA, Dailey AT, Newell DW. Diagnosis and treatment of craniocervical dislocation in a series of 17 consecutive survivors during an 8-year period. J Neurosurg Spine. 2006. 4: 429-40
2. Bucholz RW, Burkhead WZ. The pathological anatomy of fatal atlanto-occipital dislocations. J Bone Joint Surg Am. 1979. 61: 248-50
3. Chandraraj S, Briggs CA. Failure of somite differentiation at the cranio-vertebral region as a cause of occipitalization of the atlas. Spine (Phila Pa 1976). 1992. 17: 1249-51
4. Chaput CD, Torres E, Davis M, Song J, Rahm M. Survival of atlanto-occipital dissociation correlates with atlanto-occipital distraction, injury severity score, and neurologic status. J Trauma. 2011. 71: 393-5
5. Chaput CD, Walgama J, Torres E, Dominguez D, Hanson J, Song J. Defining and detecting missed ligamentous injuries of the occipitocervical complex. Spine (Phila Pa 1976). 2011. 36: 709-14
6. Chaudhary N, Wang BH, Gurr KR, Bailey SI, Bailey CS. A rare case of atlantooccipital dissociation in the context of occipitalization of the atlas, with a 2-year follow-up. J Neurosurg Spine. 2013. 18: 189-93
7. Cooper Z, Gross JA, Lacey JM, Traven N, Mirza SK, Arbabi S. Identifying survivors with traumatic craniocervical dissociation: A retrospective study. J Surg Res. 2010. 160: 3-8
8. Fard SA, Avila MJ, Johnstone CM, Patel AS, Walter CM, Skoch J. Prognostic factors in traumatic atlanto-occipital dislocation. J Clin Neurosci. 2016. 33: 63-8
9. Fiester P, Soule E, Natter P, Rao D. Tectorial membrane injury in adult and pediatric trauma patients: A retrospective review and proposed classification scheme. Emerg Radiol. 2019. 26: 615-22
10. Gholve PA, Hosalkar HS, Ricchetti ET, Pollock AN, Dormans JP, Drummond DS. Occipitalization of the atlas in children. Morphologic classification, associations, and clinical relevance. J Bone Joint Surg Am. 2007. 89: 571-8
11. Gnanadev R, Ishak B, Iwanaga J, Loukas M, Tubbs RS. A traumatic dislocation of the atlas from the axis in a patient with atlantooccipital assimilation. Cureus. 2019. 11: e4402
12. Hall GC, Kinsman MJ, Nazar RG, Hruska RT, Mansfield KJ, Boakye M. Atlanto-occipital dislocation. World J Orthop. 2015. 6: 236-43
13. Horn EM, Feiz-Erfan I, Lekovic GP, Dickman CA, Sonntag VK, Theodore N. Survivors of occipitoatlantal dislocation injuries: Imaging and clinical correlates. J Neurosurg Spine. 2007. 6: 113-20
14. Horn EM, Lekovic GP, Feiz-Erfan I, Sonntag VK, Theodore N. Cervical magnetic resonance imaging abnormalities not predictive of cervical spine instability in traumatically injured patients. Invited submission from the joint section meeting on disorders of the spine and peripheral nerves,March 2004. J Neurosurg Spine. 2004. 1: 39-42
15. Kasliwal MK, Fontes RB, Traynelis VC. Occipitocervical dissociation-incidence, evaluation, and treatment. Curr Rev Musculoskelet Med. 2016. 9: 247-54
16. Kimchi G, Greenberg G, Traynelis VC, Witiw CD, Knoller N, Harel R. Integrity of the tectorial membrane is a favorable prognostic factor in atlanto-occipital dislocation. Br J Neurosurg. 2020:
17. Martinez-del-Campo E, Kalb S, Soriano-Baron H, Turner JD, Neal MT, Uschold T. Computed tomography parameters for atlantooccipital dislocation in adult patients: The occipital condyle-C1 interval. J Neurosurg Spine. 2016. 24: 535-45
18. Mendenhall SK, Sivaganesan A, Mistry A, Sivasubramaniam P, McGirt MJ, Devin CJ. Traumatic atlantooccipital dislocation: Comprehensive assessment of mortality, neurologic improvement, and patient-reported outcomes at a Level 1 trauma center over 15 years. Spine J. 2015. 15: 2385-95
19. Mueller FJ, Kinner B, Rosskopf M, Neumann C, Nerlich M, Fuechtmeier B. Incidence and outcome of atlanto-occipital dissociation at a level 1 trauma centre: A prospective study of five cases within 5 years. Eur Spine J. 2013. 22: 65-71
20. Osborn AG, Hedlund GL, Salzman KL.editors. Osborn’s Brain: Imaging, Pathology, and Anatomy. Philadelphia, PA: Elsevier; 2018. p.
21. Phuntsok R, Ellis BJ, Herron MR, Provost CW, Dailey AT, Brockmeyer DL. The occipitoatlantal capsular ligaments are the primary stabilizers of the occipitoatlantal joint in the craniocervical junction: A finite element analysis. J Neurosurg Spine. 2019. 30: 593-601
22. Radcliff KE, Ben-Galim P, Dreiangel N, Martin SB, Reitman CA, Lin JN. Comprehensive computed tomography assessment of the upper cervical anatomy: What is normal?. Spine J. 2010. 10: 219-29
23. Reis A, Bransford R, Penoyar T, Chapman J, Bellabarba C. Diagnosis and treatment of craniocervical dissociation in 48 consecutive survivors. Evid Based Spine Care J. 2010. 1: 69-70
24. Schellenberg M, Inaba K, Cheng V, Bardes JM, Heindel P, Matsushima K. Independent predictors of survival after traumatic atlanto-occipital dissociation. J Trauma Acute Care Surg. 2018. 85: 375-9
25. Sharma DK, Sharma D, Sharma V. Atlantooccipital fusion: Prevalence and its developmental and clinical correlation. J Clin Diagn Res. 2017. 11: AC01-3
26. Tavolaro C, Pulido H, Bransford R, Bellabarba C. Traumatic craniocervical dissociation in patients with congenital assimilation of the atlas to the occiput. Case Rep Orthop. 2019. 2019: 2617379
27. Tubbs RS, Hallock JD, Radcliff V, Naftel RP, Mortazavi M, Shoja MM. Ligaments of the craniocervical junction: A review. J Neurosurg Spine. 2011. 14: 697-709
28. Vaccaro AR, Lim MR, Lee JY. Indications for surgery and stabilization techniques of the occipito-cervical junction. Injury. 2005. 36: S44-53
29. Vakili ST, Aguilar JC, Muller J. Sudden unexpected death associated with atlanto-occipital fusion. Am J Forensic Med Pathol. 1985. 6: 39-43
30. Zong R, Yin Y, Qiao G, Jin Y, Yu X. Quantitative measurements of the skull base and craniovertebral junction in congenital occipitalization of the atlas: A computed tomography-based anatomic study. World Neurosurg. 2017. 99: 96-103