- Department of Neurosurgery, Japanese Red Cross Kumamoto Hospital, Kumamoto City, Japan.
Correspondence Address:
Shimpei Tsuboki, Department of Neurosurgery, Japanese Red Cross Kumamoto Hospital, Kumamoto City, Japan.
DOI:10.25259/SNI_334_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Shimpei Tsuboki, Yukihiro Imaoka, Tatemi Todaka. Successful stent-assisted coil embolization for a recurrent distal posterior inferior cerebellar artery aneurysm: A case presentation. 05-Jul-2024;15:236
How to cite this URL: Shimpei Tsuboki, Yukihiro Imaoka, Tatemi Todaka. Successful stent-assisted coil embolization for a recurrent distal posterior inferior cerebellar artery aneurysm: A case presentation. 05-Jul-2024;15:236. Available from: https://surgicalneurologyint.com/surgicalint-articles/12973/
Abstract
Background: Distal posterior inferior cerebellar artery (PICA) aneurysms are exceedingly rare intracranial aneurysms. In the acute phase of rupture, interventions commonly involve parent artery occlusion through endovascular treatment or direct trapping surgery. There is no consensus on the best treatment of chronic ruptured or unruptured aneurysms, and stent-assisted coil embolization has not yet been reported in the chronic phase of rupture.
Case Description: We present a case of a 46-year-old female with a recurrent distal PICA aneurysm at 18 months following the initial treatment for subarachnoid hemorrhage and was treated by stent-assisted coil embolization with Neuroform Atlas (Stryker, USA), with a favorable outcome.
Conclusion: Distal PICA aneurysms occur at the apical curvature, where primitive arterial anastomoses existed during development, pointing to the potential vulnerability of the vessel wall at these sites. Stent-assisted coil embolization has shown effectiveness in preserving the parent artery for chronic ruptured and unruptured distal PICA aneurysms. Nonetheless, the narrowness and tortuosity of the PICA present obstacles to treatment. In our case, the procedure was feasible utilizing the Neuroform Atlas (Stryker, USA) with the Transcell approach. A thorough grasp of the characteristics of stents and their application is pivotal for achieving effective treatment outcomes.
Keywords: Endovascular treatment, Peripheral aneurysm, Posterior inferior cerebellar artery aneurysm, Stent-assisted coil embolization
INTRODUCTION
Aneurysms originating from the distal posterior inferior cerebellar artery (PICA) are exceedingly uncommon, and the intricate positioning and tortuosity of the PICA present challenges in the utilization of stent-assisted coil (SAC) embolization. Previously, only three instances have been documented, confined to two case series reports.[
CASE REPORT
A 46-year-old female presented with a recurrent aneurysm located televelotonsillar segment of PICA at 18 months following the initial coiling procedure for subarachnoid hemorrhage [
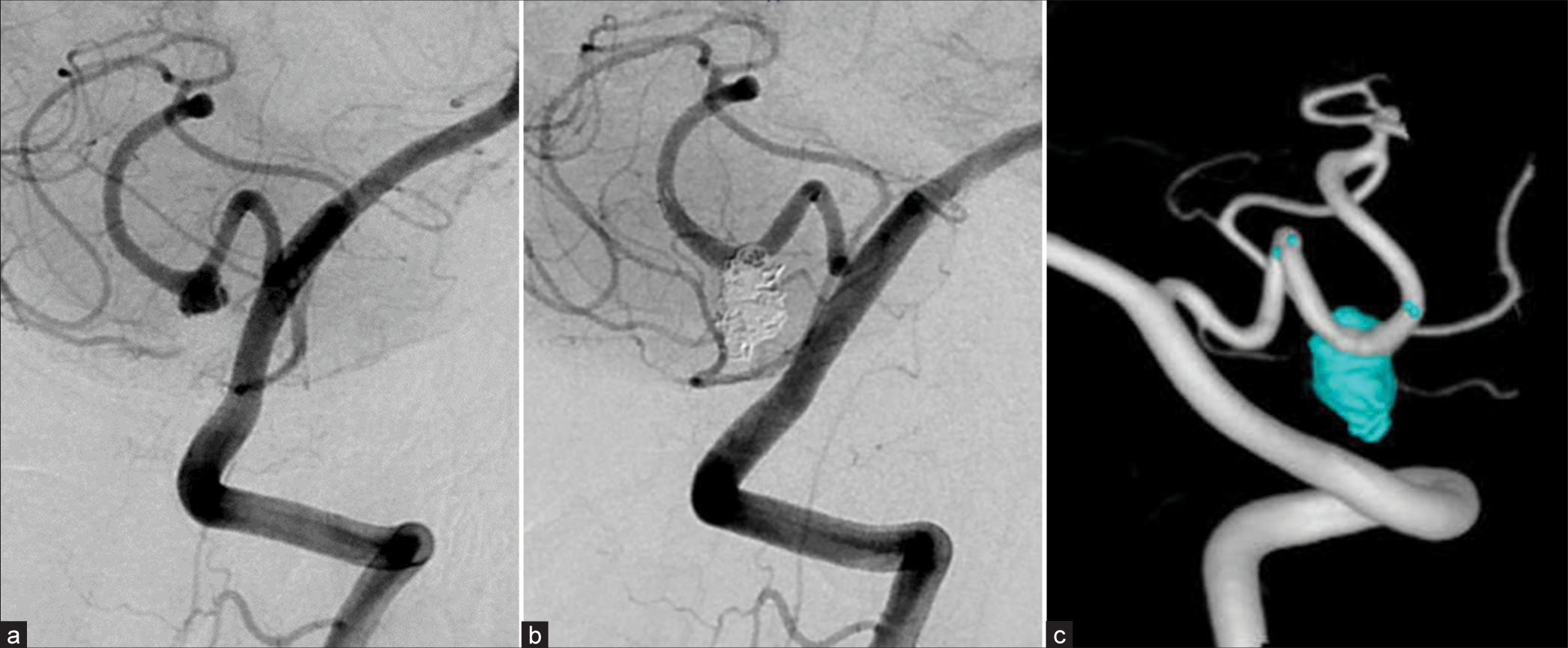
Figure 1:
(a) Digital subtraction angiography performed 18 months post initial operation revealed the recurrence of an aneurysm situated at the telovelotonsillar segment of the posterior inferior cerebellar artery. (b) Subsequent to the reoperation, digital subtraction angiography evidenced the complete occlusion of the aneurysm, concurrently affirming the preservation of the posterior inferior cerebellar artery. (c) A three-dimensional digital subtraction angiography, conducted 6 months postoperation, disclosed the absence of any recurrence.
Endovascular treatment using stent-assisted coil embolization was performed under general anesthesia. A 5 Fr FUBUKI Dilator kit (ASAHI intecc, Japan) was inserted into the right vertebral artery. An Excelsior SL-10 microcatheter (Stryker, USA) was inserted into the PICA and advanced distal to the aneurysm, which was navigated by a CHIKAI Black 14 micro guidewire (Asahi intecc, Japan). A Neuroform Atlas 3.0 mm * 15mm (Stryker, USA) was deployed to cover the aneurysmal neck from the Excelsior SL-10 microcatheter. The Excelsior SL-10 on the CHIKAI Black 14 was navigated into the aneurysm through the Neuroform Atlas. The aneurysm was occluded with four coils without any periprocedural complications, and the patency of the PICA was preserved [
DISCUSSION
The incidence of distal PICA aneurysms is much rarer than that of the proximal segment, constituting <30% of all PICA aneurysms, accounting for 0.5–1.7% of all intracranial aneurysms.[
A previous study has indicated a lack of significant difference in outcomes between parent artery occlusion (PAO) and selective coil embolization for acutely ruptured aneurysms.[
While a total of three stent-coil cases for distal PICA aneurysms have been reported through two case series studies focusing on acute ruptured aneurysms, this is the first report detailing SAC of a chronic ruptured distal PICA aneurysm.
CONCLUSION
Stent-assisted coil embolization is a reasonable treatment for distal PICA aneurysms when attempting to preserve the PICA and more experiences are expected to be accumulated in the future.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Anil G, Sein L, Nga V, Teo K, Chou N, Yeo TT. Dissecting distal cerebellar artery aneurysms: Options beyond a parent vessel sacrifice. Neurosurg Rev. 2020. 43: 771-80
2. Chen X, Sun Z, Shi L, Xu L, Yu J, Fang B. Endovascular management of ruptured distal posterior inferior cerebellar artery aneurysms A retrospective cohort study. Medicine (United States). 2018. 97: e13300
3. Fujiwara K, Ito J, Kanayama S. Multiple aneurysms of the PICA communicating artery : A case report. No Shinkei Geka. 1999. 27: 177-82
4. Funakoshi Y, Imamura H, Tani S, Adachi H, Fukumitsu R, Sunohara T. Effect of straightening the parent vessels in stent-assisted coil embolization for anterior communicating artery aneurysms. World Neurosurg. 2019. 126: e410-6
5. Horiuchi T, Tanaka Y, Hongo K, Nitta J, Kusano Y, Kobayashi S. Characteristics of distal posteroinferior cerebellar artery aneurysms. Neurosurgery. 2003. 53: 589-95 discussion 595-6
6. Hou K, Yu J. Application of the neuroform atlas stent in intracranial aneurysms: Current status. Front Neurol. 2022. 13: 829143
7. Iwakami T, Fujii N, Son J. Comparison of the physical characteristics of support stents for cerebral aneurysm embolization. J Neuroendovasc Ther. 2021. 15: 778-86
8. Lewis SB, Chang DJ, Peace DA, Lafrentz PJ, Day AL. Distal posterior inferior cerebellar artery aneurysms: Clinical features and management. J Neurosurg. 2002. 97: 756-66
9. Ozaki T, Fujinaka T, Kidani T, Nishimoto K, Yamazaki H, Sawada H. Coil embolization of unruptured cerebral aneurysms using stents in small arteries less than 2 mm in diameter. Neurosurgery. 2022. 90: 538-46
10. Shin H, Lee S, Koh J. Endovascular treatment of ruptured distal posterior inferior cerebellar artery aneurysm, report of two exemplary cases and retrospective analysis of 11 cases. J Neurol Surg A Cent Eur Neurosurg. 2014. 75: 343-9