- Department of Neurological Surgery, University of Wisconsin School of Medicine and Public Health, Madison, Wisconsin, United States.
Correspondence Address:
Amgad S. Hanna, Department of Neurological Surgery, University of Wisconsin School of Medicine and Public Health, Madison, Wisconsin, United States.
DOI:10.25259/SNI_806_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Garret P. Greeneway, Paul S. Page, Miguel Angel Navarro, Amgad S. Hanna. Supraclavius muscle observed during anterior scalenectomy for thoracic outlet syndrome: A report of two cases and review of the literature. 30-Dec-2022;13:600
How to cite this URL: Garret P. Greeneway, Paul S. Page, Miguel Angel Navarro, Amgad S. Hanna. Supraclavius muscle observed during anterior scalenectomy for thoracic outlet syndrome: A report of two cases and review of the literature. 30-Dec-2022;13:600. Available from: https://surgicalneurologyint.com/surgicalint-articles/supraclavius-muscle-observed-during-anterior-scalenectomy-for-thoracic-outlet-syndrome-a-report-of-two-cases-and-review-of-the-literature/
Abstract
Background: Thoracic outlet syndrome (TOS) is a clinical diagnosis caused by compression of neurovascular structures in the thoracic outlet. There are a variety of structures that cause compression implicated in TOS. TOS patients frequently require surgical decompression. Various structural anomalies encountered during decompression have been reported in the literature.
Case Description: We present two females (ages 42 and 45) that each underwent anterior scalenectomy for thoracic outlet decompression through a supraclavicular approach. A supraclavius muscle anomaly was observed in both patients. Analogous to the two reports previously described in the literature, the muscle inserted, along the medial superior undersurface of the clavicle and originated dorsally along the trapezius muscle. This is not to be confused with the subclavius posticus muscle, which originates from the first rib and inserts on the upper border of the scapula.
Conclusion: These two cases represent just the third and fourth ever descriptions of a supraclavius muscle anomaly encountered during TOS surgery. Due to the wide variety of anatomical variations encountered during TOS surgery, it is not only crucial for continued reporting of such anatomical variations to be reported in the literature but equally important for clinicians that treat TOS to be aware of such variations.
Keywords: Anterior scalenectomy, Muscle anomaly, Supraclavius, Thoracic outlet syndrome
INTRODUCTION
Thoracic outlet syndrome (TOS) was first described by Peet et al. as a clinical diagnosis in 1956.[
Conservative management, such as physical therapy, is the first line of therapy in patients presenting with TOS. However, surgery is often indicated in patients that fail conservative management. The surgical approach in patients with TOS depends on what structure causes compression and where compression of the neurovascular structures occurs. At our institution, we routinely perform anterior scalenectomy through a supraclavicular approach in patients that present with signs and symptoms consistent with TOS and fail conservative management.
There have been multiple reports in the literature of anomalous muscles and other connective tissue structures described anatomically when performing surgical approaches for thoracic outlet syndrome.[
CASE REPORTS
Case 1
A 42-year-old female with an unremarkable medical history presented to the neurosurgery clinic with complaints of the left arm weakness and numbness. She also reported a perception of the left arm heaviness exacerbated with arm elevation. Physical examination revealed positive thoracic outlet maneuvers in the left upper limb. A Tinel sign was positive over the left supraclavicular area. The patient demonstrated a positive scratch collapse test in the left supraclavicular region. She manifested a Medical Research Council grade 4/5 of the left triceps, handgrip, interossei, and thenar eminence. There was evidence of decreased light touch sensation over the fourth and fifth digits of the left hand, the ulnar aspect of the left hand, and the ulnar aspect of the left distal forearm both anteriorly and posteriorly. Deep tendon reflexes were 2+ and symmetric in the bilateral upper limbs.
Electromyography (EMG)/nerve conduction studies were unremarkable. A computerized tomography (CT) scan of the cervical spine did not reveal a cervical rib but did demonstrate a mildly elongated left C7 transverse process. Vascular ultrasound studies revealed arterial impingement with thoracic outlet maneuvers in the left subclavian artery with her left arm positioned at 90°, hyperextended, and head hyperextended to both the right and left. Given the patient’s reported signs and symptoms, physical examination findings, and diagnostic imaging findings, she was clinically diagnosed with TOS. Due to her persistent symptoms despite nonoperative management, she was offered a left anterior scalenectomy through a supraclavicular approach for thoracic outlet decompression.
The patient was taken to the operating room and positioned supine. A curvilinear incision was planned two finger breadths superior to the left clavicle, lateral to the posterior border of the sternocleidomastoid muscle, and anterior to the anterior border of the trapezius muscle. From here, a standard dissection was performed down to the level of the superficial fat pad. An anomalous muscle, distinct from the sternocleidomastoid muscle, was immediately identified traversing the supraclavicular space [
Case 2
A 45-year-old female with an unremarkable medical history presented to the neurosurgery clinic complaining of a 15-year history of progressively worsening right arm weakness and numbness, exacerbated by activities that required her to elevate her arm. Of note, roughly 1 year before presentation, she underwent a diagnostic workup under the direction of a vascular surgeon and was diagnosed with the right-sided TOS. Vascular ultrasound studies at that time revealed right subclavian arterial impingement with one provoking maneuver, compression of the subclavian vein in four positions, and a nonocclusive deep vein thrombosis of the right subclavian vein. EMG performed at that time was unremarkable. CT of the cervical spine was unremarkable for a cervical rib. An initial procedure at that time was performed by vascular surgery for rib resection and pectoralis minor release through an infraclavicular approach. The patient did not get symptomatic relief from this and was, therefore, offered an anterior scalenectomy by neurosurgery.
The patient was taken to the operating room and positioned supine with her head turned to the left. A curvilinear incision was planned superior to the left clavicle and lateral to the sternocleidomastoid muscle. Incision was made and the subcutaneous and superficial tissues were dissected in a standard fashion. On mobilization of the supraclavicular fat pad, an anomalous muscle was identified in the supraclavicular space. This muscle was itself distinct from the sternocleidomastoid, inserted on the superior aspect of the medial clavicle, and tracked posteriorly across the supraclavicular space before diving deep to the trapezius muscle [
At her 6-week follow-up, she reported at least a 50% improvement in her numbness and complete resolution of pain.
DISCUSSION
TOS is a rare clinical diagnosis with an incidence most recently reported to range between 0.5 and 3/100,000 people/year.[
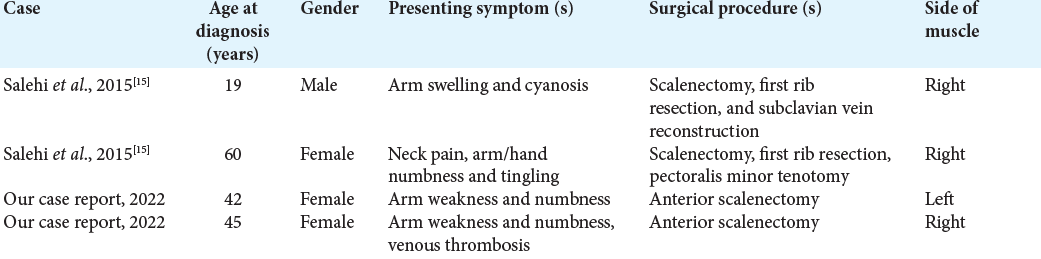
This report describes a supraclavicular muscle anomaly encountered during thoracic outlet decompression through anterior scalenectomy. Before our report, there have been just two reports of this supraclavicular muscle anomaly encountered during thoracic outlet decompression.[
In our cases and the cases previously identified in the literature, the supraclavius muscle anomaly appears to have a rather consistent relationship with its surrounding anatomical structures. Salehi et al., initially, described this muscle as attaching obliquely to the medial superior undersurface of the clavicle and just lateral to the clavicular portion of the sternocleidomastoid muscle. In their description of the muscle, they note the muscle traversing deep to the scalene fat pad, yet just anterior to the brachial plexus, where the nerves emerge from the scalene triangle. The origin of the supraclavius muscle in their report was described as lateral along the trapezius muscle. Likewise, an analogous anatomical relationship of the supraclavius muscle and its surrounding structures was appreciated in the two cases that we present [
Furthermore, the supraclavius muscle is not to be confused with the subclavius posticus muscle described in other reports.[
Among the now four cases of a supraclavius muscle anomaly reported in the literature, three out of four have been identified in a female [
In addition to reporting the third and fourth ever cases of the supraclavius muscle in the literature, we describe the second and third ever cases of a female found to have a supraclavius muscle. We also present the youngest female, 42 years of age, to date in which a supraclavius muscle was identified. We, additionally, report the first two patients to present with arm weakness as their manifesting symptom, in which a supraclavius muscle was identified. Moreover, we present the first case to date of a supraclavius muscle found on the left side of the body.
CONCLUSION
TOS is a rare clinically diagnosed entity resulting from a wide variety of compressive pathologies. Numerous structural anomalies encountered during TOS surgery have been described in the literature. Here, we present the third and fourth cases ever of a supraclavius muscle anomaly encountered during an anterior scalenectomy through a supraclavicular approach for thoracic outlet syndrome. It is vital for clinicians who diagnose and treat TOS to possess knowledge of such anatomical anomalies so that they can provide the best possible care for their patients.
Declaration of patient consent
Patients’ consent not required as patients’ identities were not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Atasoy E. A Hand surgeon’s further experience with thoracic outlet compression syndrome. J Hand Surg. 2010. 35: 1528-38
2. Brantigan CO, Roos DB. Etiology of neurogenic thoracic outlet syndrome. Hand Clin. 2004. 20: 17-22
3. Cogar AC, Johnsen PH, Potter HG, Wolfe SW. Subclavius posticus: An anomalous muscle in association with suprascapular nerve compression in an athlete. Hand (N Y). 2015. 10: 769
4. Forcada P, Rodríguez-Niedenführ M, Llusá M, Carrera A. Subclavius posticus muscle: Supernumerary muscle as a potential cause for thoracic outlet syndrome. Clin Anat. 2001. 14: 55-7
5. Grunebach H, Arnold MW, Lum YW. Thoracic outlet syndrome. Vasc Med. 2015. 20: 493-5
6. Hanna A, Bodden LO, Siebiger GR. Neurogenic thoracic outlet syndrome caused by vascular compression of the brachial plexus: A report of two cases. J Brachial Plex Peripher Nerve Inj. 2018. 13: e1-3
7. Harry WG, Bennett JD, Guha SC. Scalene muscles and the brachial plexus: Anatomical variations and their clinical significance. Clin Anat. 1997. 10: 250-2
8. Illig KA, Rodriguez-Zoppi E, Bland T, Muftah M, Jospitre E. The Incidence of thoracic outlet syndrome. Ann Vasc Surg. 2021. 70: 263-72
9. Juvonen T, Satta J, Laitala P, Luukkonen K, Nissinen J. Anomalies at the thoracic outlet are frequent in the general population. Am J Surg. 1995. 170: 33-7
10. Makhoul RG, Machleder HI. Developmental anomalies at the thoracic outlet: An analysis of 200 consecutive cases. J Vasc Surg. 1992. 16: 534-45
11. Martin RM, Vyas NM, Sedlmayr JC, Wisco JJ. Bilateral variation of subclavius muscle resembling subclavius posticus. Surg Radiol Anat. 2008. 30: 171-4
12. Peet RM, Henriksen JD, Anderson TP, Martin GM. Thoracic-outlet syndrome: Evaluation of a therapeutic exercise program. Proc Staff Meet Mayo Clin. 1956. 31: 281-7
13. Redenbach DM, Nelems B. A comparative study of structures comprising the thoracic outlet in 250 human cadavers and 72 surgical cases of thoracic outlet syndrome1. Eur J Cardiothorac Surg. 1998. 13: 353-60
14. Roos DB. Congenital anomalies associated with thoracic outlet syndrome: Anatomy, symptoms, diagnosis, and treatment. Am J Surg. 1976. 132: 771-8
15. Salehi P, Pratt WB, Joseph MF, McLaughlin LN, Thompson RW. The supraclavius muscle is a novel muscular anomaly observed in two cases of thoracic outlet syndrome. J Vasc Surg Cases. 2015. 1: 84-6
16. Sanders RJ, Illig KA, Thompson RW, Freischlag JA, Donahue DM, Jordan SE, Edgelow PI, editors. Anatomy of the thoracic outlet and related structures. Thoracic Outlet Syndrome. Berlin: Springer; 2013. p. 17-24









José Lomelí
Posted January 5, 2023, 9:14 am
I’ve red with great interest your papaer, congratulations., I always performed a cervical spine MRI in my TOS patients and I’ve found cervical disc hernia in some of them (Double Crush Syndrome). I highly recommend you do the same in your cases.