- School of Medicine, Universidad Peruana Cayetano Heredia,
- Department of Neurosurgery, Instituto de Neurociencias de Lima,
- Clínica San Felipe, Lima, Perú.
Correspondence Address:
Marco Gonzales-Portillo Showing, M.D. IFAANS Instituto de Neurociencias de Lima, Av. Del Pinar 198 – Chacarilla del Estanque 15038, Lima, Perú.
DOI:10.25259/SNI_382_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Jhon E. Bocanegra-Becerra1, Marco Gonzales-Portillo Showing2,3, Luis A. Huamán Tanta2,3. Surgical management of giant cell tumor invading the occipital bone: A case report and literature review. 12-Aug-2022;13:351
How to cite this URL: Jhon E. Bocanegra-Becerra1, Marco Gonzales-Portillo Showing2,3, Luis A. Huamán Tanta2,3. Surgical management of giant cell tumor invading the occipital bone: A case report and literature review. 12-Aug-2022;13:351. Available from: https://surgicalneurologyint.com/surgicalint-articles/11795/
Abstract
Background: Giant cell tumor of bone (GCTB) rarely originates in the skull, particularly in the occipital bone. Although benign, it can severely destroy the surrounding tissue and undergo an unpredictable clinical course. We report the successful resection of a GCTB invading the occipital bone in a Hispanic adult woman and present a comprehensive review of the literature on this rare pathology by focusing on the occipital area.
Case Description: A 40-year-old Hispanic woman presented with a 3-month history of neck pain and a bulging lesion on the retromastoid area. Brain magnetic resonance imaging (MRI) revealed an extradural, expansive, and contrast-enhancing lesion in the right occipital bone with multiple thin septa and evidence of bleeding. The patient underwent an uneventful gross total resection (GTR) of the lesion. The histopathological examination findings included numerous scattered osteoclast-type giant multinucleated cells. At a 10-month follow-up, the patient has not developed any neurological deficits, impairment of life functioning, or signs of recurrence in MRI.
Conclusion: GCTB rarely originates in the skull, being the occipital bone the most infrequent site of presentation. When feasible, total surgical resection effectively reduces the risk of recurrence. Nonetheless, radiation and adjuvant therapies have been employed when GTR could not be achieved. A close follow-up with a brain MRI is advised to control recurrence.
Keywords: Case report, Giant cell tumor of bone, Occipital bone, Skull tumor, Surgical management
INTRODUCTION
Giant cell tumor of bone (GCTB), also known as “osteoclastoma,” represents 3–5% of primary bone tumors and 10–20% of those of benign origin.[
The risk factors for the origin of GCTB in the skull base or vault are still unknown.[
Despite the benign nature of this tumor, its clinical behavior may be unpredictable, and the treatment is highly dependent on location, especially in the skull.[
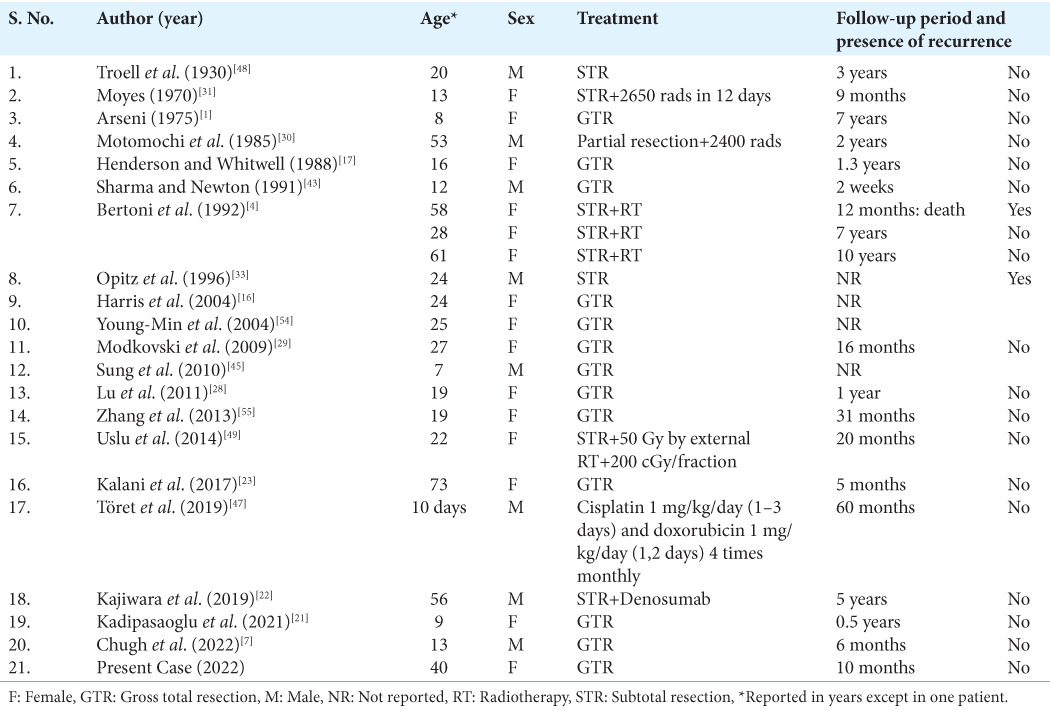
We conducted a review of the literature, which yielded 27 reported cases of GCTB originating in the occipital bone (retrieval of full-text information, including patient sex and age, type of treatment, and presence of recurrence during the follow-up was possible in 22 cases, and is shown in
CASE REPORT
A 40-year-old Hispanic woman presented to the clinic with a 3-month history of neck pain and a bulging lesion on the retromastoid area. The patient had no significant medical history. The physical examination showed a tender and swollen area on the right lateral side of the occipital bone, behind the mastoid process. Besides, the neurologic examination was intact without motor, visual, or sensory deficits.
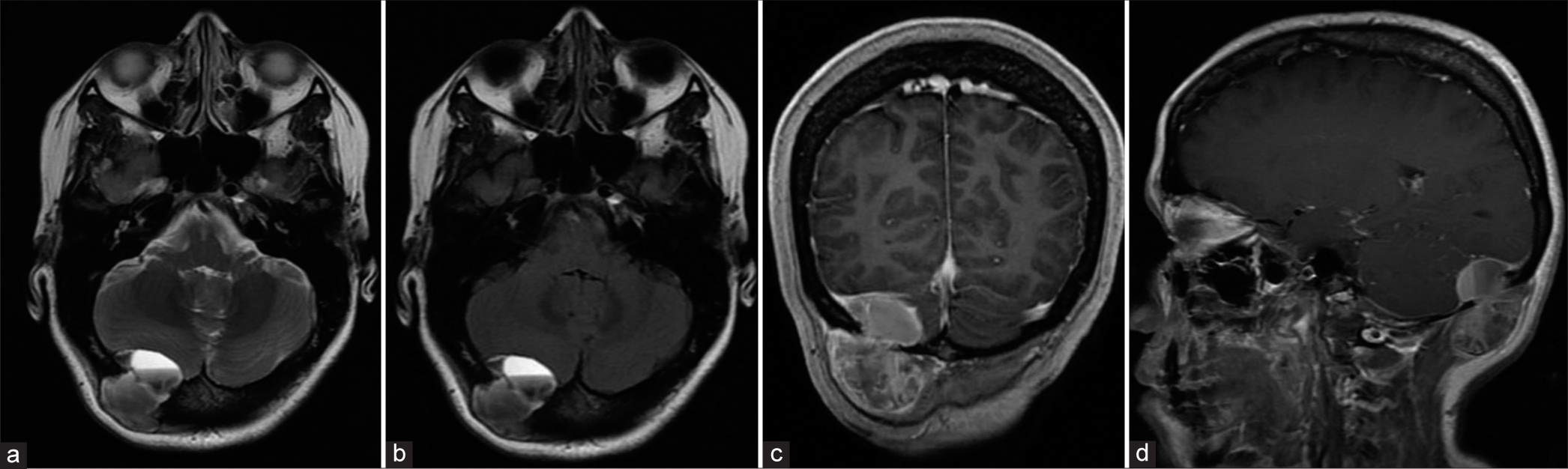
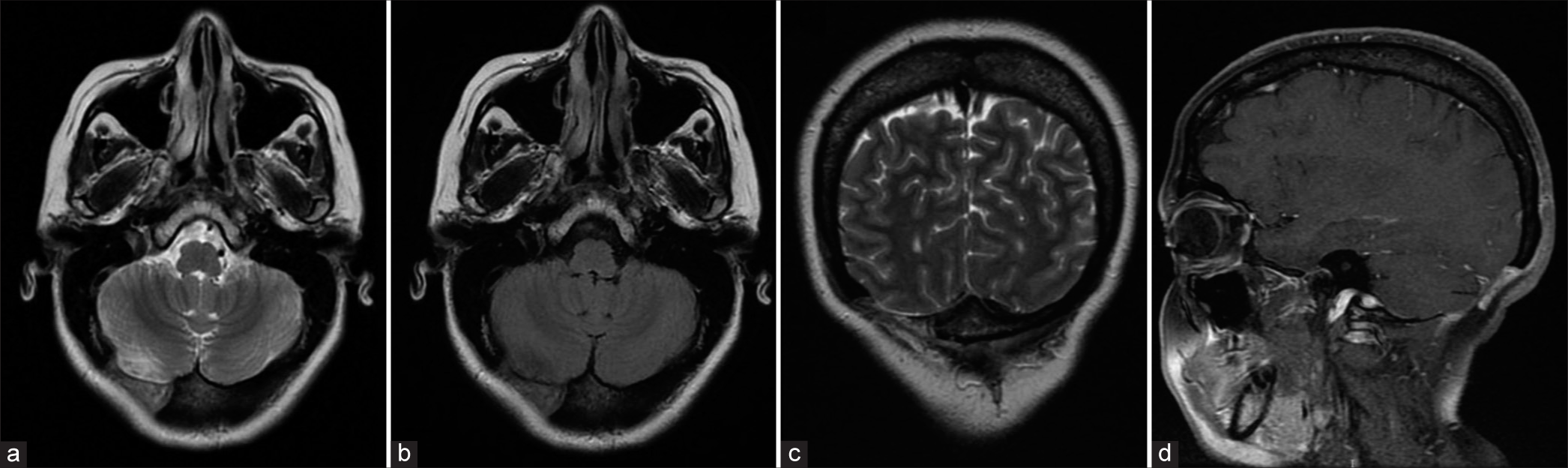
A brain magnetic resonance imaging (MRI) was obtained. The T1-weighted image with gadolinium showed an extradural and contrast-enhancing lesion destroying the inner and outer layers of the right occipital bone, which extended into the scalp and posterior fossa. It measured 42.5 × 33.5 × 39 mm. The T2-weighted image and the fluid-attenuated inversion recovery (FLAIR) sequence demonstrated a hypointense lesion with multiple thin septa, fluid-fluid levels, and signs of a hemorrhagic component [
Surgical management
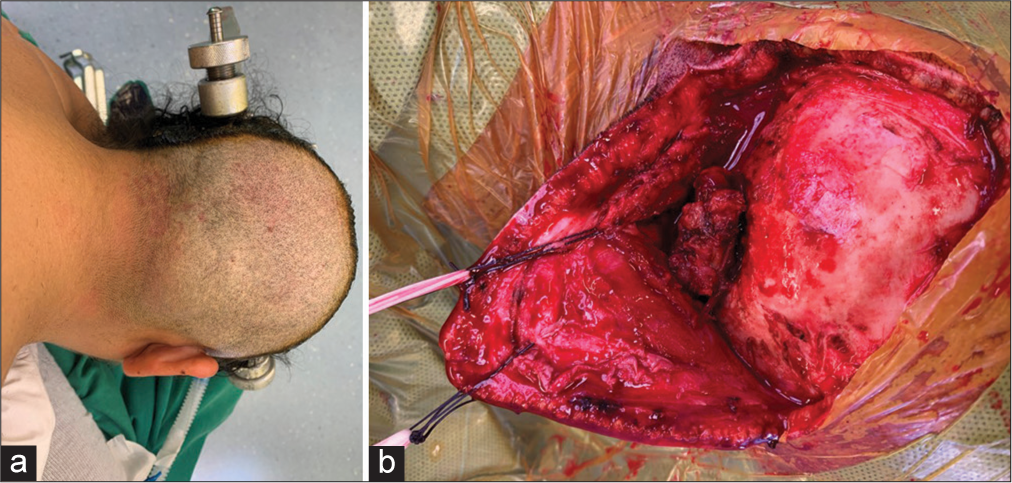
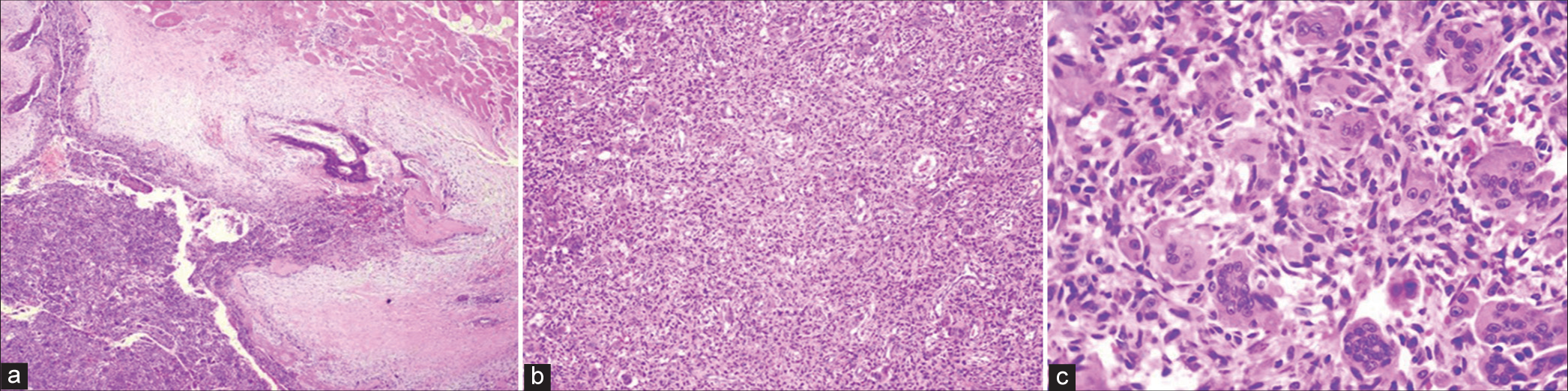
The patient was placed in a three-quarter prone position with flexion of the neck and slight head rotation. Then, a suboccipital craniotomy was performed with complete gross total resection (GTR) of the lesion. On lifting the scalp, an irregular, rounded, and brownish lesion was exposed at the surface of the right occipital bone [
Histopathological findings
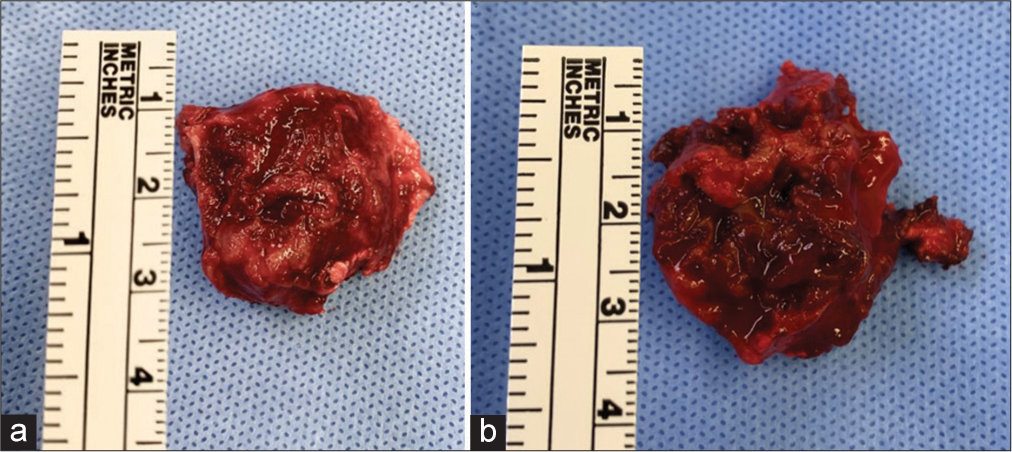
The histopathological examination of the tumor revealed fusocellular proliferation with fibrohistiocytic characteristics and hemorrhagic changes, zones of hemosiderin, and significant proliferation of scattered osteoclast-type giant multinucleated cells [
Follow-up
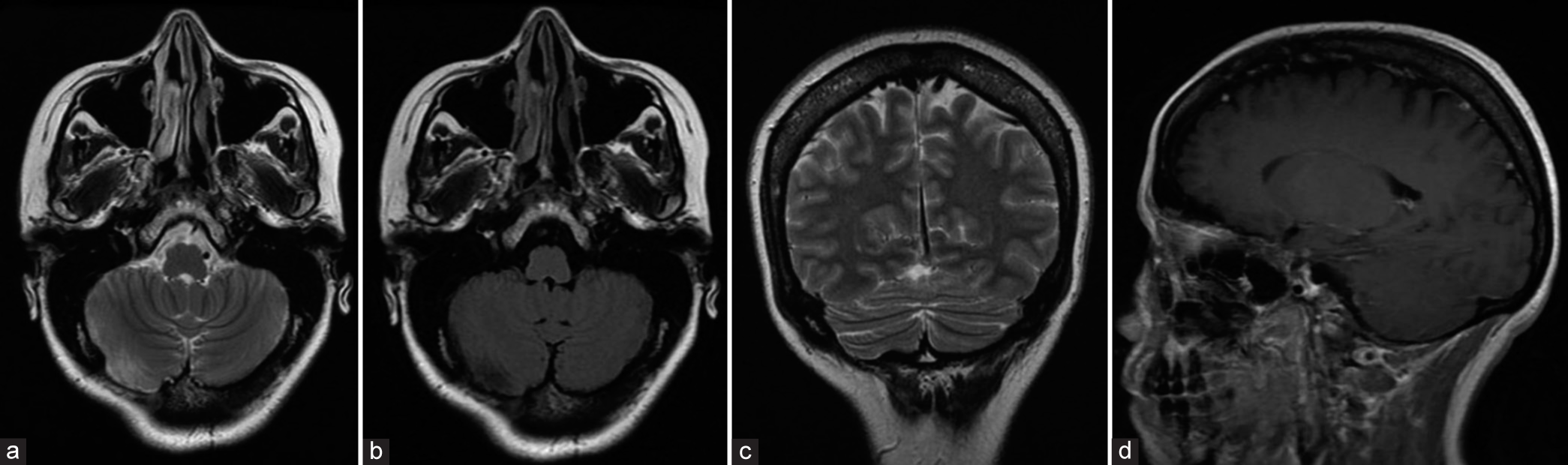
The patient has been followed up for 10 months, and she has not developed any neurological deficits or impairment of life functioning. In addition, a brain MRI has shown absent signs of recurrence or tumor proliferation in the occipital bone and surrounding tissue [
DISCUSSION
GCTB is a rare entity in the skull, particularly in the occipital area.[
GCTB is considered a benign pathology, yet it can be aggressive when invades the surrounding tissue. Although infrequent, it may also present as a malignant variant.[
The clinical presentation of GCTB in the occipital area is usually described as a tender and swollen lesion accompanied by headache, neck pain, vomiting or swelling of the affected area, and, less commonly, seizures.[
Differential diagnosis
The differential diagnosis of GCTB includes giant cell reparative granuloma, Paget’s disease of the bone, aneurysmal cyst bone, chondroblastoma, chondromyxoid fibroma, nonossifying fibroma, fibrous dysplasia, pigmented villonodular synovitis, foreign body reactions, and brown tumors from hyperparathyroidism.[
Imaging assessment modalities include computed tomography (CT) and magnetic resonance imaging (MRI). CT scan evaluates better periosteal reaction, pathologic fractures, and absence of matrix mineralization.[
Treatment
GTR has been considered the main modality of treatment and warrants careful preoperative planning to provide the maximal extent of resection.[
GTR and RT are favorable factors for progression-free survival of intracranial GCTB.[
Denosumab, a monoclonal antibody, decreases osseous destruction by inhibiting RANKL-expressing cells.[
Doxycycline sclerotherapy, adriamycin, and other chemotherapeutic agents have also shown to be effective when surgical resection is not possible, although in isolated cases.[
Zoledronic acid, a bisphosphonate agent, has been used less commonly in the skull compared to cases located in long bones.[
As a result of the unpredictable tumor recurrence even after surgical and nonsurgical modalities of treatment, patients must undergo close surveillance with follow-up MRIs every 3–6 months for the first 5 years, for example.[
CONCLUSION
GCTB rarely originates in the skull, being the occipital bone the most infrequent site of presentation. The gender distribution of this tumor in the skull is equal among adults; however, in the occipital area, females are more commonly affected. Besides, risk factors are still unknown and merit further investigation. A thorough clinical history, brain imaging, and histopathological analysis are essential for the diagnosis.
When feasible, total surgical resection effectively reduces the risk of recurrence. Nonetheless, radiation and adjuvant therapies have been employed when GTR could not be achieved. Ultimately, a close follow-up with brain MRIs is advised to control recurrence and further destruction of neighboring structures.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Arseni C, Horvath L, Maretsis M, Nicolae C. Giant cell tumors of the calvaria. J Neurosurg. 1975. 42: 535-40
2. Baena-Ocampo LD, Ramirez-Perez E, Linares-Gonzalez LM, Delgado-Chavez R. Epidemiology of bone tumors in Mexico City: Retrospective clinicopathologic study of 566 patients at a referral institution. Ann Diagn Pathol. 2009. 13: 16-21
3. Bardakhchyan S, Kager L, Danielyan S, Avagyan A, Karamyan N, Vardevanyan H. Denosumab treatment for progressive skull base giant cell tumor of bone in a 14 year old female a case report and literature review. Ital J Pediatr. 2017. 43: 32
4. Bertoni F, Unni KK, Beabout JW, Ebersold MJ. Giant cell tumor of the skull. Cancer. 1992. 70: 1124-32
5. Chan J, Gannon FH, Thompson LD. Malignant giant cell tumor of the sphenoid. Ann Diagn Pathol. 2003. 7: 100-5
6. Chatterjee D, Gupta K, Singla N, Kapoor A. Sphenoid bone: A rare site for giant cell tumor case report with literature review. Clin Neuropathol. 2016. 35: 385-8
7. Chugh A, Mohapatra A, Punia P, Gotecha SS, Choudhury P. Giant cell tumour of the occipital bone in a 13-year old male. J Ayub Med Coll Abbottabad. 2022. 34: 378-80
8. Dai WY, Tian C, Liu L. Case reports of a giant cell reparative granuloma and a giant cell tumor on temporal bone. Chin Med J (Engl). 2018. 131: 2254-6
9. Elder JB, Berry C, Gonzalez-Gomez I, Kreger MD, McComb JG. Giant cell tumor of the skull in pediatric patients. Report of two cases. J Neurosurg. 2007. 107: 69-74
10. Feigenberg SJ, Marcus RB, Zlotecki RA, Scarborough MT, Berrey BH, Enneking WF. Radiation therapy for giant cell tumors of bone. Clin Orthop Relat Res. 2003. 411: 207-16
11. Feng Z, Wang C, Li B, Cheng A, Mao M, Han Z. Surgical management of giant cell tumor involving the lateral skull base. J Craniofac Surg. 2019. 30: 1794-7
12. Freeman JL, Oushy S, Schowinsky J, Sillau S, Youssef AS. Invasive giant cell tumor of the lateral skull base: A systematic review, meta-analysis, and case illustration. World Neurosurg. 2016. 96: 47-57
13. Giffin ME, Love JG. Giant-cell tumor of occipital bone with increased intracranial pressure: Report of a case. Proc Staff Meet Mayo Clin. 1945. 20: 284-7
14. Gilani A, Kleinschmidt-DeMasters BK. Denosumab therapy obscures histological features of giant cell tumor of bone. J Neuropathol Exp Neurol. 2019. 78: 1171-3
15. Gupta RK, Batra VV, Pahwa S, Bodeliwala S, Jagetia A, Singh D. Skull-based giant cell tumor with atypical location highlighting the importance of intraoperative cytological examination: Report of four cases. Neurol India. 2018. 66: 1507-9
16. Harris AE, Beckner ME, Barnes L, Kassam A, Horowitz M. Giant cell tumor of the skull: A case report and review of the literature. Surg Neurol. 2004. 61: 274-7
17. Henderson BT, Whitwell H. Giant cell tumor of the skull: Case report. Neurosurgery. 1988. 23: 120-2
18. Huh A, Villelli N, Martinez D, Ting J, Birhiray R, Payner TD. Denosumab treatment for a residual giant cell tumor of the clivus: A case report and review of the literature. World Neurosurg. 2018. 118: 98-101
19. Jadidi S, D’Abarno A, Barkley JF, Abusuwwa RF. Giant cell tumor of the frontal bone: A case report and literature review. Cureus. 2018. 10: e3353
20. Jin SW, Sim KB, Kim SD. Development and growth of the normal cranial vault: An embryologic review. J Korean Neurosurg Soc. 2016. 59: 192-6
21. Kadipasaoglu C, Wahba A, Bhattacharjee MB, Cuglievan B, Fletcher SA. Hemorrhagic giant cell tumor of the occipital skull base: A case report and literature review. Cureus. 2021. 13: e13832
22. Kajiwara Y, Takechi A, Watanabe Y, Miyoshi H, Shiraishi T. CS-01 giant cell tumor in the skull base bone treated with anti-rankl inhibitor. Neurooncol Adv. 2019. 1: ii38
23. Kalani A, Lovett M, Stewart L, Popovic S, Panju A. A remote metastatic giant cell tumour to the skull. JRSM Open. 2017. 8: 2054270417702567
24. Karamanakos PN, Jaaskelainen JE, Alafuzoff I, Pirinen E, Vanninen R, Silvennoinen S. Malignant giant cell tumor in the posterior fossa of a neonate. J Neurosurg Pediatr. 2010. 5: 277-82
25. Kaya İ, Benzer M, Turhal G, Sercan G, Bilgen C, Kirazlı T. Giant cell tumor of the temporal bone and skull base: A case report. J Int Adv Otol. 2018. 14: 151-4
26. Kubat R. Unusual presence of osteoclastoma in the occipital bone in children. Acta Chir Orthop Traumatol Cech. 1961. 28: 246-7
27. Larsson SE, Lorentzon R, Boquist L. Giant-cell tumor of bone. A demographic, clinical, and histopathological study of all cases recorded in the Swedish cancer registry for the years 1958 through 1968. J Bone Joint Surg. 1975. 57: 167-73
28. Lu ZH, Yao ZW. Giant cell tumour of the posterior cranial fossa: A case report. Br J Radiol. 2011. 84: 208-11
29. Modkovski R, Elliott R, Rubin B, Zagzag D, Jafar J, Mikolaenko I. Giant cell tumor of the occipital bone and secondary aneurysmal bone cyst: case report and review of literature. Intern J Neurosurg. 2009. 7:
30. Motomochi M, Handa Y, Makita Y, Hashi K. Giant cell tumor of the skull. Surg Neurol. 1985. 23: 25-30
31. Moyes PD, Bratty PJ, Dolman CL. Osteoclastoma of the jugular foramen. Case report. J Neurosurg. 1970. 32: 255-7
32. Murphey MD, Nomikos GC, Flemming DJ, Gannon FH, Temple HT, Kransdorf MJ. From the archives of AFIP. Imaging of giant cell tumor and giant cell reparative granuloma of bone: Radiologic-pathologic correlation. Radiographics. 2001. 21: 1283-309
33. Opitz H, Petersen D, Heiss E, Duffner F, Meyermann R. Giant cell tumor of the occipital bone in a case of von Recklinghausen neurofibromatosis. Clin Neuropathol. 1996. 15: 226-30
34. Osaka S, Sugita H, Osaka E, Yoshida Y, Ryu J, Hemmi A. Clinical and immunohistochemical characteristics of benign giant cell tumour of bone with pulmonary metastases: Case series. J Orthop Surg (Hong Kong). 2004. 12: 55-62
35. Palmerini E, Picci P, Reichardt P, Downey G. Malignancy in giant cell tumor of bone: A review of the literature. Technol Cancer Res Treat. 2019. 18: 1533033819840000
36. Patibandla MR, Thotakura AK, Rao MN, Addagada GC, Nukavarapu MC, Panigrahi MK. Clival giant cell tumor a rare case report and review of literature with respect to current line of management. Asian J Neurosurg. 2017. 12: 78-81
37. Pousti BT, Andera L, Haugen TW. Sphenoid sinus giant cell tumor: A case report and literature review. ORL J Otorhinolaryngol Relat Spec. 2020. 82: 168-74
38. Prasad SC, Piccirillo E, Nuseir A, Sequino G, De Donato G, Paties CT. Giant Cell Tumors of the Skull Base: Case Series and Current Concepts. Audiol Neurotol. 2014. 19: 12-21
39. Seider MJ, Rich TA, Ayala AG, Murray JA. Giant cell tumors of bone: Treatment with radiation therapy. Radiology. 1986. 161: 537-40
40. Sekar A, Rudrappa S, Gopal S, Ghosal N, Gupta V, Ts L. Preoperative cytoreduction of clival giant cell tumor: An effective replication of the systemic modality in the skull base. World Neurosurg. 2018. 119: 97-102
41. Sepulveda I, Alzerreca J, Villalobos P, Ulloa JP. Giant cell tumor of the temporal bone with skull base and middle ear extension. J Med Cases. 2021. 12: 149-51
42. Shah SR, Keshri A, Behari S, Patadia S, Kumari N. Giant cell granuloma of the anterior skull base: Need for early, maximal surgical excision: A short series of 3 cases with review of literature. Indian J Otolaryngol Head Neck Surg. 2015. 67: 347-52
43. Sharma V, Newton G. Osteoclastoma of occipital bone. Yonsei Med J. 1991. 32: 169-71
44. Stagner AM, Sajed DP, Nielsen GP, Ebb DH, Faquin WC, Chebib I. Giant cell lesions of the maxillofacial skeleton express RANKL by RNA in situ hybridization regardless of histologic pattern. Am J Surg Pathol. 2019. 43: 819-26
45. Sung J, Jin K, Jae J, Young K, Hook S. A case report of giant cell tumor of the occipital bone. Arch Craniofac Surg. 2010. 11: 103-6
46. Tamura R, Miwa T, Shimizu K, Mizutani K, Tomita H, Yamane N. Giant cell tumor of the skull: Review of the literature. J Neurolog Surg A Cent Eur Neurosurg. 2016. 77: 239-46
47. Töret E, Demirağ B, Çalakvur Ş, Doğanavşargil B, Turhan T. Case report a newborn with giant cell tumor of the occipital bone: Case report address for correspondence. J Pediatr Res. 2019. 6: 256-64
48. Troell A. Two cases of giant cell tumor in bone observed 3½ and 18 years. Acta Chir Scand. 1930. 67: 906-13
49. Uslu GH, Canyilmaz E, Yöney A, Aydin S, Sahbaz A, Sari A. Giant cell tumor of the occipital bone: A case report and review of the literature. Oncol Lett. 2014. 8: 151-4
50. Viswanathan S, Jambhekar NA. Metastatic giant cell tumor of bone: Are there associated factors and best treatment modalities?. Clin Orthop Relat Res. 2010. 468: 827-33
51. Weng JC, Li D, Wang L, Wu Z, Wang JM, Li GL. Surgical management and long-term outcomes of intracranial giant cell tumors: A single-institution experience with a systematic review. J Neurosurg. 2018. 131: 695-705
52. Wong MN, Nicol K, Murakami JW. Image-guided percutaneous management of skull and spine giant cell tumors: Case report of 2 challenging cases successfully treated with doxycycline sclerotherapy. World Neurosurg X. 2020. 5: 100061
53. Yaprak Bayrak B, Özcan E, Vural Ç, Emengen A, Çabuk B, Ceylan S. A single-center experience with giant cell tumors of sphenoid bone and clivus. Tumori. 2021. 107: NP94-100
54. Young-Min K, Yong-Sook P, Se-Hoon K Jong-Hee C, YongGou P. Giant cell tumor of the occipital bone. J Korean Brain Tumor Soc. 2004. 3: 152-5
55. Zhang Z, Xu J, Yao Y, Chu S, Cheng H, Chen D. Giant cell tumors of the skull: A series of 18 cases and review of the literature. J Neurooncol. 2013. 115: 437-44
56. Zwolak P, Manivel JC, Jasinski P, Kirstein MN, Dudek AZ, Fisher J. Cytotoxic effect of zoledronic acid-loaded bone cement on giant cell tumor, multiple myeloma, and renal cell carcinoma cell lines. J Bone Joint Surg Am. 2010. 92: 162-8