- Department of Neurosurgery, Neurosurgery Teaching Hospital, Baghdad, Iraq
- Department of Surgery, College of Medicine, Alnahrain University, Baghdad, Iraq
- Department of Neurosurgery, College of Medicine, University of Baghdad, Baghdad, Iraq,
- Department of Neurosurgery, College of Medicine, Prince Sattam bin Abdulaziz University, Riyadh, Saudi Arabia,
- Department of Neurosurgery, University of Cincinnati, Ohio, United States.
Correspondence Address:
Mustafa Ismail, Department of Neurosurgery, Neurosurgery Teaching Hospital , Baghdad, Iraq.
DOI:10.25259/SNI_388_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Aws Saad Msebawy1, Zinah A. Al-Araji2, Ahmed Nazar3, Abdulaziz Alayyaf4, Saleh Abdulkareem Saleh3, Saleh Mohammed Merie1, Mohammed A. Alrawi1, Mustafa Ismail1, Samer S. Hoz5. Surgical resection of pericallosal tuberculoma through contralateral approach: A case report. 10-Nov-2023;14:396
How to cite this URL: Aws Saad Msebawy1, Zinah A. Al-Araji2, Ahmed Nazar3, Abdulaziz Alayyaf4, Saleh Abdulkareem Saleh3, Saleh Mohammed Merie1, Mohammed A. Alrawi1, Mustafa Ismail1, Samer S. Hoz5. Surgical resection of pericallosal tuberculoma through contralateral approach: A case report. 10-Nov-2023;14:396. Available from: https://surgicalneurologyint.com/surgicalint-articles/12630/
Abstract
Background: Pericallosal tuberculoma, a rare form of intracranial tuberculoma, affects the corpus callosum and results from tuberculosis (TB), a bacterial infection that can cause a myriad of symptoms. Diagnosing this condition can be challenging but can be confirmed through imaging studies and biopsy. Treatment involves a combination of antitubercular medications and surgical removal of the lesion if it is in a critical location or causing significant symptoms. This article describes the surgical management and imaging characteristics approach to a patient with intracranial tuberculoma.
Case Description: A 17-year-old female with a history of TB meningitis nine years ago presented with one week of recurrent seizures and mild third nerve palsy, later diagnosed as a tuberculoma of the corpus callosum through radiological imaging and biopsies. A total surgical resection of the lesion was performed using a contralateral interhemispheric frontal parasagittal approach. The patient went under observation and suitable follow-up plans.
Conclusion: Surgical management can effectively treat cerebral granulomas and improve neurological deficits in patients with recurring TB. Despite the possibility of complications, the benefits of such measures are highlighted in this case, suggesting that surgical intervention can be a viable option for achieving optimal outcomes in these patients.
Keywords: Gross total resection, Mycobacterium tuberculosis, Seizure, Tuberculoma, Tuberculous meningitis
INTRODUCTION
Tuberculosis (TB) involving the central nervous system (CNS), a rare manifestation of the chronic infectious disease caused by Mycobacterium tuberculosis bacteria, poses significant mortality and morbidity risks. Accounting for only 1% of all TB cases, CNS TB typically manifests as meningitis, leading to severe neurological complications that necessitate immediate diagnosis and treatment to prevent permanent disability and death.[
Pericallosal tuberculoma, a scarcely encountered brain tuberculoma, results from TB meningitis (TBM) and refers specifically to mass growth within the corpus callosum. Extra-axial tuberculomas are commonly found in the frontal and parietal areas, though they may also emerge in the suprasellar, pontine, and pericallosal regions.[
This study delineates the surgical techniques and imaging characteristics employed in addressing intracranial tuberculoma patients. Furthermore, the study seeks to offer insights into diagnostic and therapeutic approaches for this unusual condition, which can enhance patient outcomes and inform future research in this domain.
CASE SCENARIO
Presentation and examination
A 17-year-old female from Iraq was diagnosed with tuberculous meningitis nine years ago. The patient was noncompliant with anti-TB medications. She experienced a recurrence of pulmonary TB 4 years ago. Three months before admission, the patient suffered recurrent seizures for one week. Neurological examination revealed mild right-sided Ferner palsy. The patient was conscious, and there were no other notable findings.
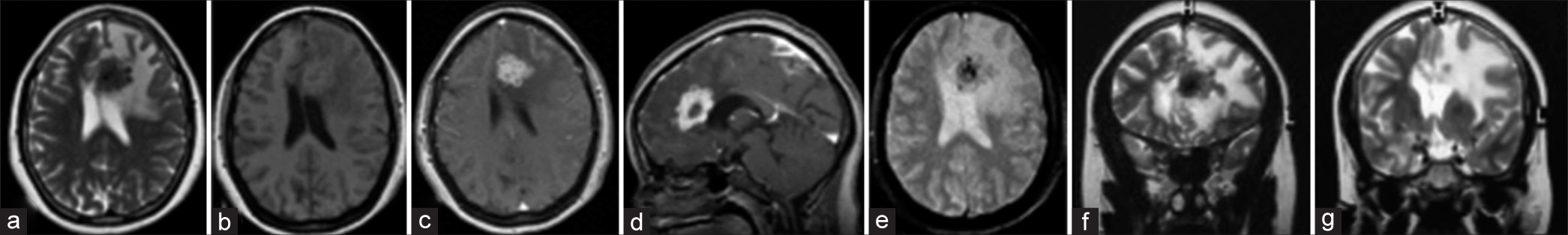
Magnetic resonance imaging (MRI) sequences displayed multiple intra-axial supratentorial lesions on the left frontal precentral area and a cluster of at least ten small lesions. These lesions exhibited a low signal on T1-weighted imaging and a complex signal on T2-weighted imaging with areas of low/iso signal surrounding vasogenic edema. They appeared as signal voids in gradient echo sequences. Postcontrast sequences revealed a peripheral cluster of ring enhancement of the small lesions (granulomas). A mass effect was noted on midline structures with right-sided subfalcine herniation [
Figure 1:
(a-g) The preoperation magnetic resonance imaging sequences demonstrate multiple intra-axial supratentorial lesions on the left of the frontal precentral location, and at least ten small lesions cluster together. These lesions are of low signal on T1-weighted imaging, the complex signal on T2-weighted imaging with areas of low/iso signal, surrounding vasogenic edema, and appear as a signal void in GRE. On postcontrast sequences, there is a peripheral cluster of ring enhancement of the small lesions (granulomas). (f and g) A mass effect is noted on the midline structures with subfalcine herniation.
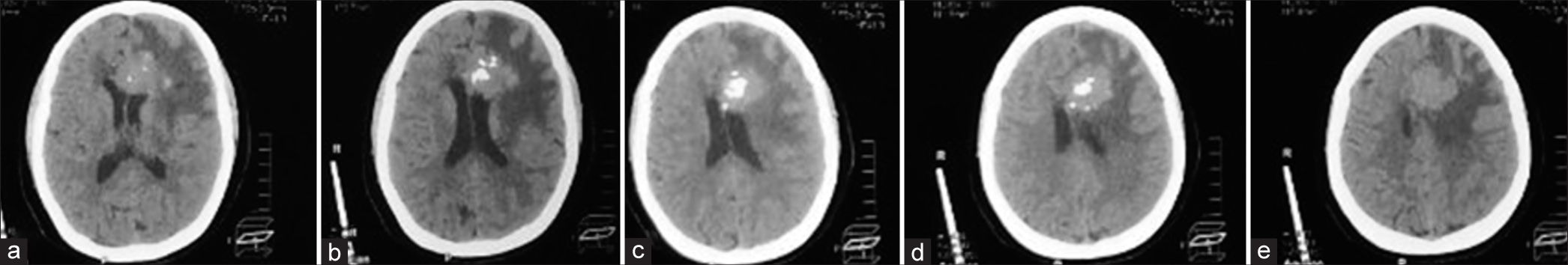
Figure 2:
(a-e) Axial brain computed tomography (CT) scans without contrast images, which demonstrate a left pericallosal isodense lesion with areas of hyperdensities. The lesion is ill-defined, round-shaped, and measures approximately 3 × 3 cm. It is causing a mass effect on the left frontal horn and minimal midline shift. Diffuse left frontotemporal vasogenic edema is noted.
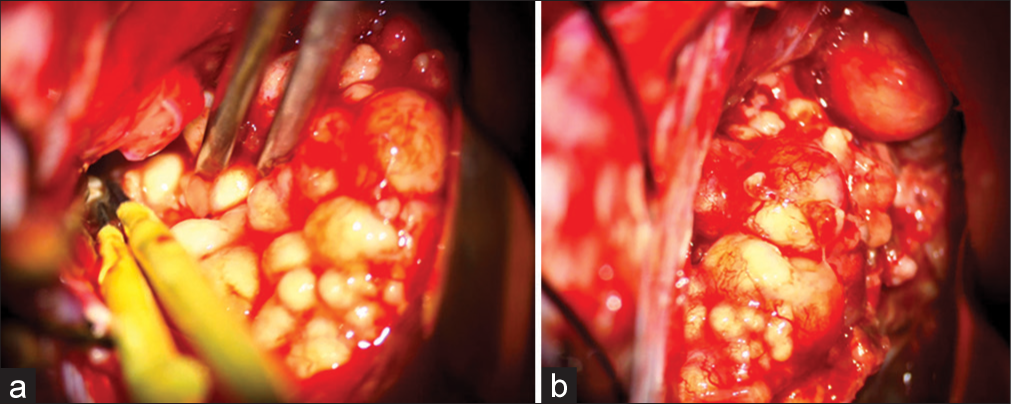
Operation
The patient underwent craniotomy through a contralateral interhemispheric right frontal parasagittal approach, which allowed for a gross total resection of the mass. Selecting this modification is mainly due to the lateral extension of pathology. The lesion had both pericallosal arteries entered and terminated inside it, which were atrophied and subsequently removed. The ventricle was dissected due to the involvement of the corpus callosum [
Postoperation course
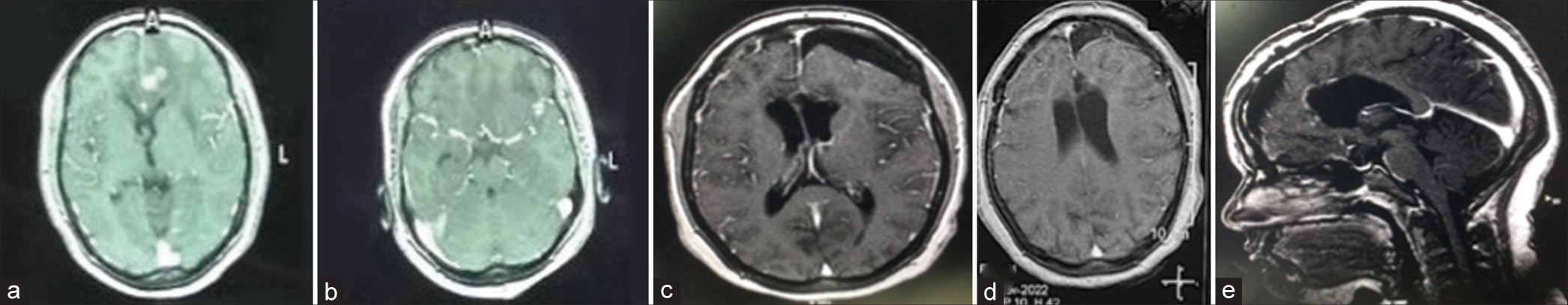
The patient was conscious and experienced a single seizure managed with antiepileptic medication. She also suffered mild left foot drop resulting from scarifying right bridging veins during surgery; however, it resolved over time through physiotherapy. It lasted for two months. The patient developed severe conjunctivitis, which was resolved with medication. She was discharged on a 12-month course of anti-TB medication, to which she adhered, and her neurological deficits improved. A follow-up MRI 12 months post-surgery [
DISCUSSION
Cerebral tuberculoma is a condition in which the brain parenchyma reacts to an M. tuberculosis infection, exhibiting stages such as granulomas, abscesses, and calcifications. Brain infection by M. tuberculosis can occur through bloodborne dissemination or during tuberculous meningitis. Furthermore, a cerebral tuberculoma can rupture and infect the subarachnoid space.[
CT and MRI are as sensitive when detecting intracranial tuberculomas in all patients. It was observed that MRI was slightly more effective in diagnosing brain stem tuberculomas as a result of its ability to assess the extent of the lesion accurately. Tuberculomas vary in appearance on a T2-weighted image according to the stage of evolution. Small tuberculomas appear to be scattered areas of varying intensity, whereas mature tuberculomas appear to be space-occupying lesions with a central area of low signal and surrounding edema. The lack of signal has probably been caused by thick fibrosis, calcification, and free radicals. It usually shows an enhancement of contrast, which is ring or annular. Ring enhancement is common. Caseation usually results in the “target sign” appearance.[
Medical management is appropriate for patients with communicating hydrocephalus and should be the first-line therapy in patients in Vellore Grades 1 and 2. Steroids are usually given to all patients with TBM and may reduce hydrocephalus. More than 70 % of patients may benefit from medical treatment to prevent shunting surgery. However, medical management should be discontinued if the patient does not respond to treatment or is starting to worsen despite medicines.[
The ipsilateral interhemispheric approach is the traditional approach for pericallosal lesions.[
The patient suffered from seizures in this case, and imaging showed at least ten small lesion clusters together. CT shows a hyperdense lesion in the left anterior part of the lateral ventricle with subfalcine herniation to the right, so we decided that the patient needs total gross resection. The common approach in surgery of pericallosal tuberculoma is the ipsilateral approach. However, the contralateral approach may be considered depending on the lesion’s depth, the patient’s age, and the surgeon’s preference.
CONCLUSION
Surgical management can effectively treat intracranial tuberculomas and ameliorate neurological deficits in patients experiencing recurrent TB. Despite the possibility of complications, the benefits of such measures are highlighted in this case, suggesting that surgical intervention can be a viable option for achieving optimal outcomes in these patients.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Ahmadi SA, Roozbeh H, Abbasi A, Bahadori M, Moghaddam KG, Ketabchi SE. Cerebral tuberculoma in pregnancy: Overview of the literature and report of a case. Acta Med Iran. 2011. 49: 64-9
2. Arseni C. Two hundred and one cases of intracranial tuberculoma treated surgically. J Neurol Neurosurg Psychiatry. 1958. 21: 308-11
3. Carmel PW. Tumours of the third ventricle. Acta Neurochir (Wien). 1985. 75: 136-46
4. Draouat S, Abdenabi B, Ghanem M, Bourjat P. Computed tomography of cerebral tuberculoma. J Comput Assist Tomogr. 1987. 11: 594-7
5. Gray F. Bacterial infections. Brain Pathol. 1997. 7: 629-47
6. Gupta RK, Kohli A, Gaur V, Lal JH, Kishore J. MRI of the brain in patients with miliary pulmonary tuberculosis without symptoms or signs of central nervous system involvement. Neuroradiology. 1997. 39: 699-704
7. Hamid Changal K, Raina AH. Central nervous system manifestations of tuberculosis: A review article. Mycobact Dis. 2014. 4: 146
8. Ishak B, Jenkins S, Bordes S, Mehta K, Iwanaga J, Loukas M. A contralateral transfalcine approach to the mesial frontoparietal region and cingulate gyrus: A cadaveric feasibility study. World Neurosurg. 2019. 127: e1127-31
9. Kioumehr F, Dadsetan MR, Rooholamini SA, Au A. Central nervous system tuberculosis: MRI. Neuroradiology. 1994. 36: 93-6
10. Marais S, Roos I, Mitha A, Patel V, Kalincik T, Bhigjee AI. Presentation and outcome of patients with intracranial tuberculoma in a high HIV prevalence setting. Int J Tuberc Lung Dis. 2020. 24: 224-32
11. Rajshekhar V. Surgery for brain tuberculosis: A review. Acta Neurochir (Wien). 2015. 157: 1665-78
12. Salgado P, Del Brutto OH, Talamás O, Zenteno MA, Rodríguez-Carbajal J. Intracranial tuberculoma: MR imaging. Neuroradiology. 1989. 31: 299-302