- Department of Neurosurgery, Kanazawa University, Kanazawa, Japan,
- Department of Neurosurgery, Kanazawa Medical University, Uchinada, Japan,
- Department of Neurosurgery, Kanazawa Medical Center, Kanazawa, Japan.
Correspondence Address:
Kouichi Misaki, Department of Neurosurgery, Kanazawa University, Kanazawa, Japan.
DOI:10.25259/SNI_1087_2022
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Taishi Tsutsui1, Kouichi Misaki1, Akifumi Yoshikawa2, Kenshu Nogami1, Iku Nambu1, Tomoya Kamide1, Naoki Muramatsu3, Mitsutoshi Nakada1. Targeted transvenous embolization of a dural arteriovenous fistula at the jugular tubercle venous complex. 03-Feb-2023;14:44
How to cite this URL: Taishi Tsutsui1, Kouichi Misaki1, Akifumi Yoshikawa2, Kenshu Nogami1, Iku Nambu1, Tomoya Kamide1, Naoki Muramatsu3, Mitsutoshi Nakada1. Targeted transvenous embolization of a dural arteriovenous fistula at the jugular tubercle venous complex. 03-Feb-2023;14:44. Available from: https://surgicalneurologyint.com/surgicalint-articles/12135/
Abstract
Background: Dural arteriovenous fistulas (dAVFs) occurring near the hypoglossal canal are rare. Detailed evaluation of vascular structures can identify shunt pouches at the jugular tubercle venous complex (JTVC) in the bone near the hypoglossal canal. Although the JTVC has several venous connections, including the hypoglossal canal, there have been no reports of transvenous embolization (TVE) of a dAVF at the JTVC using an approach route other than the hypoglossal canal. This report describes the first case of complete occlusion with targeted TVE using an alternative approach route in a 70-year-old woman presenting with tinnitus diagnosed with dAVF at the JTVC.
Case Description: The patient had no history of head trauma or other preexisting conditions. Magnetic resonance imaging (MRI) showed no abnormal findings in the brain parenchyma. Magnetic resonance angiography (MRA) revealed a dAVF near the ACC. The shunt pouch was located in the JTVC, near the left hypoglossal canal, with feeders from the bilateral ascending pharyngeal arteries and occipital arteries, left meningohypophyseal trunk, and odontoid arch of the left vertebral artery. TVE was performed near the shunt pouch. Localized packing of the shunt point was achieved. The patient’s tinnitus improved. Postoperative MRI showed disappearance of the shunt without any complications. No recurrence was observed on MRA 6 months after treatment.
Conclusion: Our results suggest targeted TVE is an effective treatment for dAVFs at the JTVC.
Keywords: Dural arteriovenous fistula, Hypoglossal canal, Jugular tubercle venous complex, Transvenous embolization
INTRODUCTION
Dural arteriovenous fistula (dAVF) is a condition, in which the dural artery shunts into intracranial dural structures. Although dAVFs are relatively uncommon, with an incidence of 0.16/100,000 individuals per year, treatment prospects are increasing due to advances in imaging technology.[
The hypoglossal canal is an important structure for the passage of nerves and arteries including the hypoglossal nerve, the neuromeningeal branch of the ascending pharyngeal artery, and the anterior condylar vein (ACV), which is connected medially to the intracranial marginal sinus and laterally to the jugular vein. The confluence of the ACV and the jugular vein is known as the anterior condylar confluence (ACC). The ACC is also confluent anteriorly with the inferior petrosal sinus and posteriorly with the lateral condylar vein. The jugular tubercle venous complex (JTVC) is a vein near the hypoglossal canal that is connected to several veins including the ACV, the posterior condylar vein, the jugular vein, and surrounding venous channels. In recent years, there have been reports of dAVFs at the JTVC.[
There are several treatment options for dAVFs. In dAVFs around the hypoglossal canal, transvenous embolization (TVE) through the ACV is often chosen over transarterial embolization (TAE) to avoid embolization of the arteries feeding the lower cranial nerves. However, TVE must be limited to a localized area to avoid complications and reduce treatment costs.[
CASE REPORT
A 70-year-old woman presented with pulsating tinnitus without neurological deficits. The patient had no history of head trauma or other preexisting conditions. Magnetic resonance imaging (MRI) showed no abnormal findings in the brain parenchyma. Magnetic resonance angiography (MRA) revealed a dAVF near the ACC. The shunt pouch was located in the JTVC, near the left hypoglossal canal, with feeders from the bilateral ascending pharyngeal arteries and occipital arteries, left meningohypophyseal trunk, and odontoid arch of the left vertebral artery [
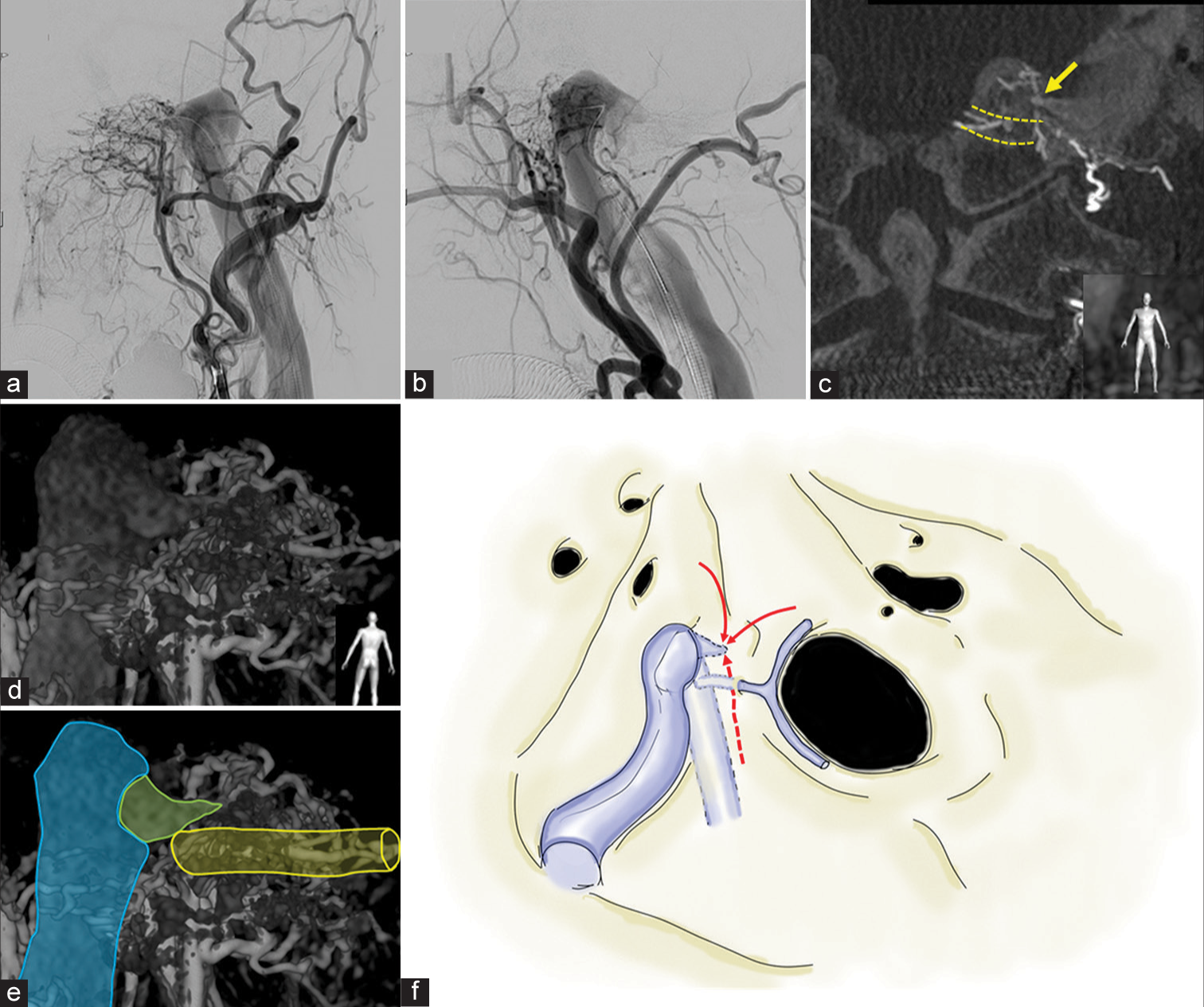
Figure 1:
Angiography images (a-e) and ]schematic diagram (f) of the dural arteriovenous fistula (a and b) frontal and lateral view of the left external carotid angiography images showing a dural arteriovenous fistula near the anterior condylar confluence with outflow to the jugular vein and no backflow to the sinus or cortical vein. (c) A coronal view of cone-beam computed tomography reconstructed from 3D-rotational angiography (3D-RA) through the left external carotid artery showing the fistula (arrow) within the bone superomedially to the hypoglossal canal (yellow line), just under the jugular tubercle. (d and e) 3D-RA images showing a shunt pouch (green) in the bone near the hypoglossal canal (yellow), which drains into the jugular vein (blue). (f) A schematic diagram shows that several feeders (red arrows and dashed arrow) are flowing into a shunt pouch located within a bone near the hypoglossal canal.
TVE was performed near the shunt pouch [
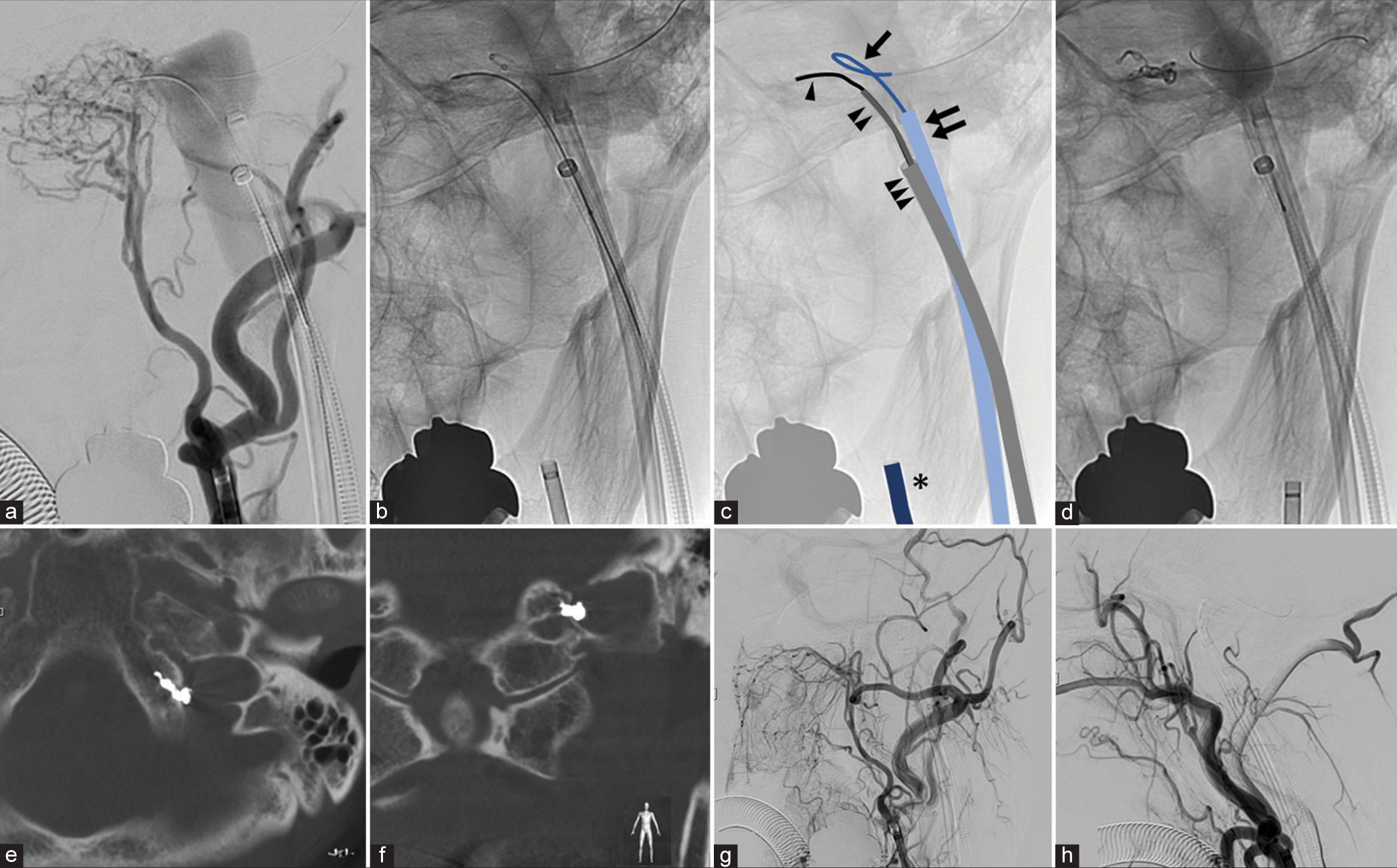
Figure 2:
Endovascular treatment of dural arteriovenous fistula (a-d) and postoperative imaging (e-h) (a) Working angle view of the left external carotid angiography through a 4 Fr. guiding sheath (as seen in panel c: *) showing a dural arteriovenous fistula. (b and c) A microcatheter (single arrowhead) is guided to the shunt point using a 45° pre-shaped distal access catheter (double arrowhead) through a 6 Fr guiding sheath (triple arrowhead) which is placed in the left internal jugular vein. Another 6 Fr guiding sheath (double arrow) is also placed in the left internal jugular vein to guide a balloon catheter (single arrow) near the shunt. (d) The balloon catheter is inflated to support the microcatheter and to avoid deviation of the coil to the jugular vein. Coiling into the shunt pouch is performed through the catheter. (e and f) Axial and coronal view from cone-beam computed tomography images showing the detachable coils implanted in the shunt pouch within the bone. (g and h) Frontal and lateral view of the left external carotid angiography showing that the shunt is completely occluded.
In the early postoperative period, the patient’s tinnitus improved. Postoperative MRI showed disappearance of the shunt without any complications, such as intracranial infarction or hemorrhage. No recurrence was observed on MRA 6 months after treatment.
DISCUSSION
It has been reported that dAVFs at the ACC are rare, accounting for 1.8–3.6% of intracranial dAVFs;[
The structures around the hypoglossal canal are complex, and it is important to fully evaluate and understand them in detail to determine the treatment strategy. In cases of dAVF around the hypoglossal canal, the feeding artery is often related to the feeding vessel of the nerve. TAE with liquid embolization has low complete occlusion rate (70%) and is not recommended.[
In the case presented here, we chose to treat the fistula with TVE because it was a dAVF with a shunt in the JTVC near the hypoglossal canal. We managed to completely occlude the shunt through localized embolization using minimal coils. This is the first report of complete occlusion of a dAVF with a shunt at the JTVC by localized point packing using a coil. Our results suggest that localized TVE is an effective treatment for dAVFs at the JTVC near the hypoglossal canal.
CONCLUSION
We report the first case of a dAVF with a shunt at the JTVC that was treated with minimal coil embolization. Our results suggest targeted TVE is an effective treatment for dAVFs at the JTVC.
Statement of ethics
Written informed consent was obtained from the patients for publication of this case series and any accompanying images. Ethical approval is not required for this study in accordance with local or national guidelines.
Data availability statement
Data and materials comply with standards and available on request. All data generated or analyzed during this study are included in this article. Further enquiries can be directed to the corresponding author.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Ernst R, Bulas R, Tomsick T, van Loveren H, Aziz KA. Three cases of dural arteriovenous fistula of the anterior condylar vein within the hypoglossal canal. AJNR Am J Neuroradiol. 1999. 20: 2016-20
2. Hsu YH, Lee CW, Liu HM, Wang YH, Chen YF. Endovascular treatment and computed imaging follow-up of 14 anterior condylar dural arteriovenous fistulas. Interv Neuroradiol. 2014. 20: 368-77
3. Kiyosue H, Tanoue S, Okahara M, Mori M, Mori H. Ocular symptoms associated with a dural arteriovenous fistula involving the hypoglossal canal: Selective transvenous coil embolization. Case report. J Neurosurg. 2001. 94: 630-2
4. Manabe S, Satoh K, Matsubara S, Satomi J, Hanaoka M, Nagahiro S. Characteristics, diagnosis and treatment of hypoglossal canal dural arteriovenous fistula: Report of nine cases. Neuroradiology. 2008. 50: 715-21
5. Misaki K, Uchiyama N, Mohri M, Aida Y, Uno T, Nakada M. Unique venous drainage of a sphenoid wing dural arteriovenous fistula with ocular symptoms. World Neurosurg. 2017. 97: 753.e1-5
6. Mizutani K, Akiyama T, Minami Y, Toda M, Fujiwara H, Jinzaki M. Intraosseous venous structures adjacent to the jugular tubercle associated with an anterior condylar dural arteriovenous fistula. Neuroradiology. 2018. 60: 487-96
7. Nambu K, Misaki K, Yoshikawa A, Kamide T, Nambu I, Sasagawa Y. Cavernous sinus dural arteriovenous fistula with an enhanced lesion in the brainstem mimicking a malignant tumor. World Neurosurg. 2020. 140: 13-7
8. Okahara M, Kiyosue H, Tanoue S, Sagara Y, Hori Y, Kashiwagi J. Selective transvenous embolization of dural arteriovenous fistulas involving the hypoglossal canal. Interv Neuroradiol. 2007. 13: 59-66
9. Shi ZS, Ziegler J, Gonzalez NR, Feng L, Tateshima S, Jahan R. Transarterial embolization of clival dural arteriovenous fistulae using liquid embolic agents. Neurosurgery. 2008. 62: 408-15 discussion 415
10. Tanoue S, Goto K, Oota S. Endovascular treatment for dural arteriovenous fistula of the anterior condylar vein with unusual venous drainage: Report of two cases. AJNR Am J Neuroradiol. 2005. 26: 1955-9