- Department of Neurosurgery, University of Baghdad, Baghdad, Iraq
- Department of Neurosurgery, University of Al-Mustansiriyah, Baghdad, Iraq
- Department of Neurosurgery, Neurosurgery Teaching Hospital, Baghdad, Iraq
- Department of Neurosurgery, Imam Abdulrahman Bin Faisal University, Dammam, Saudi Arabia
- Department of Neurosurgery, University of Pittsburgh, Pittsburgh, United States
Correspondence Address:
Samer S. Hoz, Department of Neurosurgery, University of Pittsburgh, Pittsburgh, United States.
DOI:10.25259/SNI_440_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Mustafa Ismail1, Ahmed Muthana1, Teeba A. Al-Ageely1, Fatimah Oday Ahmed2, Rania H. Al-Taie2, Aktham O. Al-Khafaji1, Mahmood F. Al-Zaidy1, Hayder R. Salih3, Mohammed A. Alrawi3, Awfa Aktham3, Hosam Al-Jehani4, Samer S. Hoz5. Teleproctoring in therapeutic neurointervention: Experience from Iraq-Saudi Arabia collaboration. 09-Aug-2024;15:280
How to cite this URL: Mustafa Ismail1, Ahmed Muthana1, Teeba A. Al-Ageely1, Fatimah Oday Ahmed2, Rania H. Al-Taie2, Aktham O. Al-Khafaji1, Mahmood F. Al-Zaidy1, Hayder R. Salih3, Mohammed A. Alrawi3, Awfa Aktham3, Hosam Al-Jehani4, Samer S. Hoz5. Teleproctoring in therapeutic neurointervention: Experience from Iraq-Saudi Arabia collaboration. 09-Aug-2024;15:280. Available from: https://surgicalneurologyint.com/surgicalint-articles/13030/
Abstract
Background: Proctoring in neuroendovascular surgery is one of the potential solutions for the shortage of personnel and experience, particularly in unstable and limited-resource areas such as Iraq.
Methods: The study was conducted at the Baghdad Neurovascular Center (BNC), the first Hybrid neurovascular institution in Iraq, where sequential online zoom-based meetings between the BNC team and the expert from the Kingdom of Saudi Arabia were used for teleproctoring for neurointerventional procedures.
Results: A total of 28 sessions were conducted, four sessions for each case. Seven cases with various intracranial vascular lesions were operated for neuroendovascular procedures from July/2021 to March/2022. The teleproctoring for each case included four sequential sessions: (1) preoperative planning, (2) device selection and preparation, (3) intraoperative live-stream proctoring, and (4) postoperative reflection and follow-up planning. The procedures include coiling for dural arteriovenous fistula; preoperative tumor embolization; preoperative, partial, and staged embolization for arteriovenous malformation; coiling for intracranial aneurysm; and attempted Giant aneurysm flow-diversion. Major complications were avoided through teleproctoring, and all patients had good outcomes. In addition, the teleproctoring provided an effective training experience to the local neuroendovascular team that is otherwise not feasible.
Conclusion: Teleproctoring is an effective and feasible tool to improve patient outcomes and provide a training experience to the local neuroendovascular teams in resource-limited regions.
Keywords: Limited-resource area, Low- and middle-income countries, Medical Education, Neuroendovascular, Telemedicine, Teleproctoring
INTRODUCTION
Surgical proctoring, encompassing the practices of observation, supervision, and instruction provided by field experts, plays a pivotal role in various domains.[
MATERIALS AND METHODS
Participants
The proctor is an Assistant Professor, Hossam Al-Jehani, who is a highly qualified neurosurgeon with expertise in open vascular/neuroendovascular/neurocritical care. The field surgical team operating within the center comprises five vascular neurosurgeons with dual training. Notably, the head of the team possesses a 3-month fellowship experience in Japan, while the remaining team members have acquired their expertise through self-training within the team. In addition, the team includes two residents, one radiology assistant, three nurses, and three medical students who contribute to the collective effort.
Setting
The proctor is based in Dammam, Saudi Arabia, which is located at a distance of 944 km (587 miles) from Baghdad, where the surgical team is operating. All preoperative screening, operative procedures, and postoperative care were conducted in the Baghdad Neurovascular Center (BNC), which stands as the inaugural hybrid neurovascular institution in Iraq, having been established in 2021. Within the BNC, a wide range of neurovascular procedures are conducted, encompassing both open cerebrovascular surgeries and diagnostic/therapeutic interventions. The BNC itself comprises two fully equipped operative rooms. One room is specifically dedicated to open vascular neurosurgeries, while the other functions as a catheterization laboratory equipped with a GE Innova Cath Lab®, specifically designed for neurointerventional procedures. Over the past 18 months, the BNC has successfully performed over 200 diagnostic cerebral and spinal angiography procedures, in addition to 23 therapeutic neurointerventional procedures.
Technological preparations
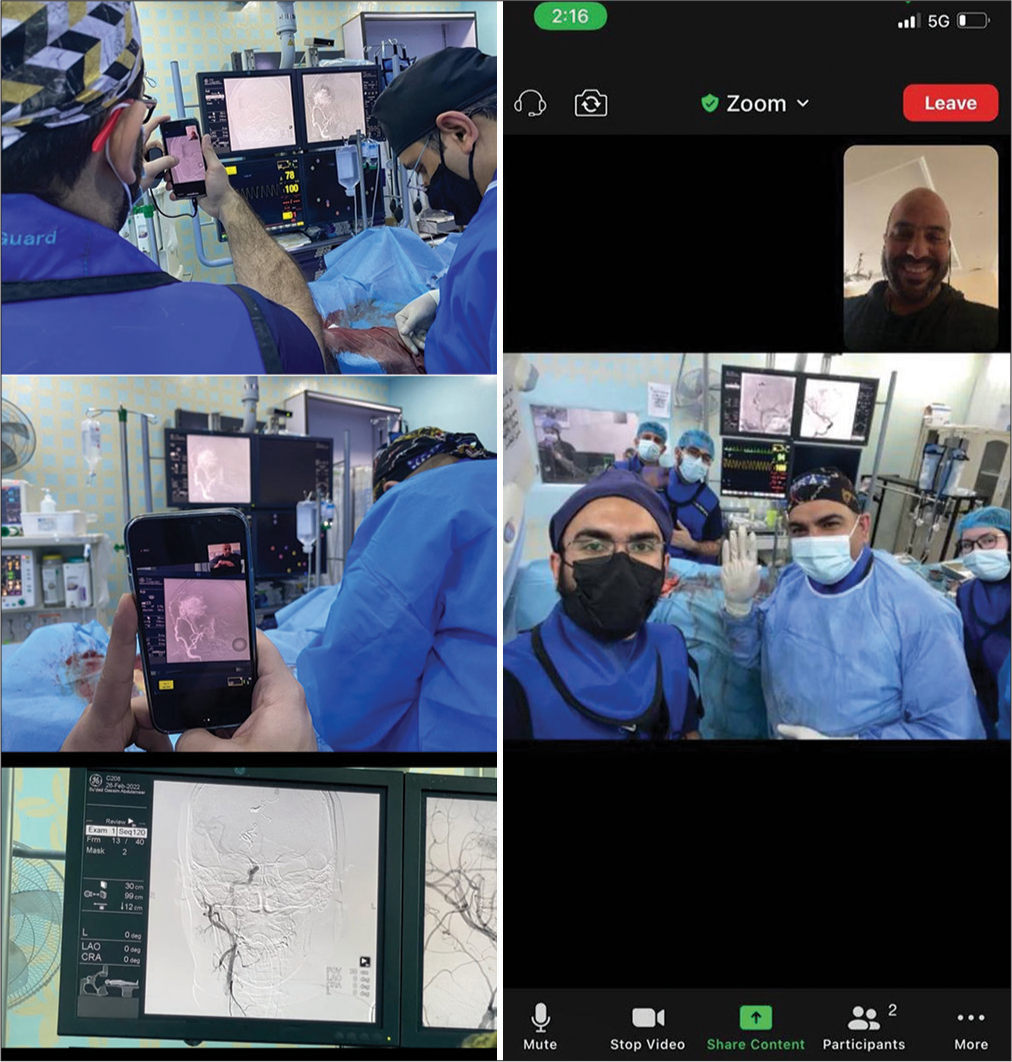
A web conferencing platform (ZoomR) was used for communication between the proctor and the proctee’s team. All hardware and software requirements were tested and ensured at the time of operation. Internet connection was tested before each procedure and meeting to be at a minimum of 10 Mbps. Both the proctor and field surgeon had 4G Wi-Fi hotspots. Two-way audio was provided through a speaker, and a portable smartphone stream in the operating room provided a video feed of the angiogram screen for the proctor. Within the angiography suite, a designated member of the BNC team was responsible for securely holding a phone attached to a stand. This arrangement enabled the proctor to remotely assess and monitor the pre-procedural preparations and provide guidance as needed, both before and during the procedure [
Preoperative preparations
The operating room was ensured to be extremely quiet, a situation which is not that usual with the involvement of multiple team members. Before commencing the interventional procedures for the enrolled patients, the BNC team established a seamless online meeting with the proctor. These meetings served as a platform for comprehensive discussions regarding the treatment strategies and the specific type of intervention required for each patient. The discussions were based on a thorough analysis of the patient’s diagnostic images, including computed tomography (CT) scans, CT angiography, magnetic resonance imaging, and catheter angiography. It is important to note that all selected patients were informed about the decision-making process and the implementation of teleproctoring as part of their treatment journey.
Teleproctoring procedure
During the operation, the teleprocotor followed the field surgeon through the procedure in a step-by-step fashion. The navigation was through one-to-one anatomy-based conversation. Occasionally, it was necessary to relocate to the angiography station during the procedure to engage in discussions with the proctor regarding decisions related to the initial contrast runs. Moreover, the proctor offered invaluable advice and direction throughout the procedure, fostering ongoing discussions with the surgical team. The frequency of these discussions escalated as the surgeon approached critical steps and neared the finalization of the intervention.
RESULTS
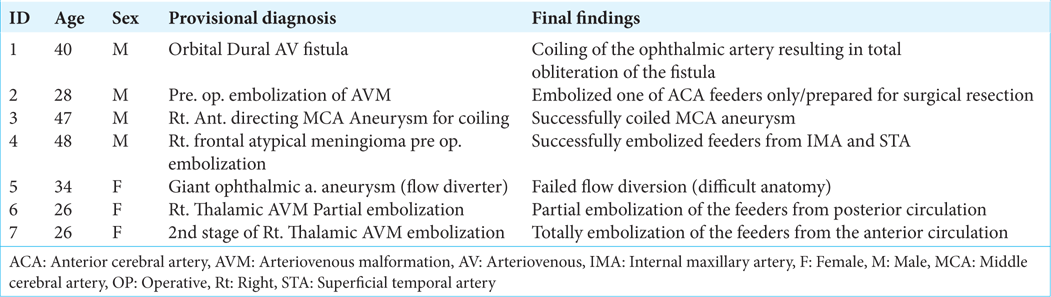
Throughout the pilot period, 28 teleproctoring sessions were conducted, spanning from July 2021 to March 2022. Seven cases with various intracranial vascular lesions were operated on for neuroendovascular procedures. The teleproctoring for each case includes four sequential sessions: (1) preoperative planning, (2) device selection and preparation, (3) intraoperative live-stream proctoring, and (4) postoperative reflection and follow-up planning. The seven cases included four males and three females with an age between 26 and 48 years old. Diverse intracranial vascular lesions were carefully selected for neuroendovascular procedures, including one case of dura arteriovenous fistula treated through coiling; one case involved pre-operative embolization of a meningioma; and two cases of intracranial aneurysms, including a giant aneurysm attempted through flow diversion. In addition, there were three cases of brain arteriovenous malformation (AVM), the first with preoperative embolization, the second needed partial embolization, and the last one required two stages of embolization for their AVMs. Further, details and indications for each of the seven cases are shown in [
Among the 28 teleproctoring sessions, all were successfully live-streamed in real time. There were no major technological issues, including any interruption in the stream, loss of video or audio, poor resolution, or significant lag time. Internet connection was stable throughout the procedures, and image quality was sufficient for the proctor to perceive and comment on pertinent anatomical structures, instrument handling, positioning, and technique. However, image distortion was encountered due to light overexposure and motion artifacts. Nevertheless, both the field surgeon and the proctor rated the overall video quality as good. They found the technology to be helpful for achieving better surgical results.
The teleproctoring sessions of our cases
The teleproctoring for each of our seven cases included four sequential online sessions. The first session was about the preoperative planning. This session involved case discussion and answering the question to treat or not, then selecting the appropriate treatment modality that can compensate for the patient’s need and the potential affordable cost.
The second session involved the device selection and preparation. Due to the unavailability of direct outlets for endovascular companies in Baghdad, limited types and sizes were available for the team. Thus, the selected modality of treatment should be modified according to the available kits and settings. An example is the use of coils for embolization whenever possible as the cost is much more affordable as compared to embolization agents. Those coils were selected to the maximum length acceptable to the case to decrease the potential number of coils required for the procedure.
The third session was the actual intraoperative live-stream teleproctoring. Throughout this session, continuous discussion and step-by-step confirmation between the operating team and the proctor were maintained. This included the navigation through unforeseen technical challenges using the immediate clinical-radiological feedback and how to bail out in complex situations. In addition, the discussion with the proctor provided the answer to the most challenging questions for the operating team, like when to stop and whether there are additional steps that can be done to optimize the outcome.
The fourth and last session was the postoperative reflection and follow-up planning. This critical session was usually done within 24 hours of the procedure or before the patient’s discharge from the hospital. The postoperative clinical status, long-term follow-up plan, medications, potential complications, and how to do better the next time were topics to be discussed in that session.
Illustrative cases
Case 5
A 34-year-old female presented with a giant ophthalmic aneurysm. Intraoperatively, the field surgical team encountered a difficult anatomical curve for the supraclinoid carotid while aiming to treat the aneurysm with flow diversion. The proctor navigates the operating team to troubleshoot the problem using variable catheters and wires and by reshaping the microwires. Due to the limited resources, several attempts were applied systematically, where all accessible options were fulfilled with no success. At that point, we decided to quit the procedure based on a discussion with the proctor and when all partners were convinced.
Case 6
A 26-year-old female with right thalamic AVM, the case was the first reported coil migration during the pressure cooker technique with coil-augmented Onyx injection technique in Iraq. The size and location of the AVM led to the decision to use onyx for multistage endovascular embolization. During the operation, the coil detached and migrated in the medial prefrontal branch through the anterior cerebral artery. The coil migrated distally before onyx insertion. After several attempts to retain the migrated coil, the decision with the proctor made as no intervention to retrieve the coil because the detachment piece is small and lodged distally [
Figure 2:
Digital subtraction angiography of AP view of the right internal carotid artery showing the coil migration in a distal branch of the anterior cerebral artery (Red arrow). It also shows the complete obliteration of the arteriovenous malformation nidus. Note: The callosomarginal artery, in this case, is a segmented artery with the two segments originating separately from the pericallosal artery.
DISCUSSION
Teleproctoring in surgery was first reported more than 20 years ago.[
Advantages of teleproctoring
One of the benefits of teleproctoring is eliminating the need for the proctor’s physical presence, which could reduce the scheduling delay for a procedure.[
The advantage incorporated in the online experience of the proctoring is that the neuroendovascular suite in the hospital did not change the regular setting that the field surgical team operates within.[
Several intraoperative advantages are provided by the teleproctoring as perceived by the local BNC team through the following examples.[
Challenges of teleproctoring
In the context of online proctoring neurointerventional cases, high image quality for the remote proctor is crucial.[
Time zone differences posed another logistical difficulty for live-streaming.[
Apart from technical issues, situational awareness is regarded as a crucial non-technical element of decision-making and can be applied to intricate medical procedures as a precondition for preventing complications.[
The ethical issue for preparing such proctoring in Iraq was another challenge and required peculiar communication with the patients before the procedures. The patients in Iraq may confront a societal issue as an external doctor participates in their case and advises the surgical team. Nonetheless, all the patients agreed on this point that an assistant professor from Saudi Arabia would be present online with the team in the case. Such straightforward consent from the patients is interesting as such online proctoring is not widespread in healthcare delivery in Iraq. Furthermore, their consent reflects their trust in the doctors who manage their cases.
From the proctor’s perspective, the continuous stress in every decision or advice the proctor gives during the procedure represents a major challenge. Furthermore, the pressure to understand all the possible details to make the best-informed decision is a highly demanding psychological state the proctor passes through. It is the inner fear of what if something goes wrong. Nevertheless, similar stress as a proctor will be present even if everything is in the right direction.
Finally, our study included a limited number of cases, rendering our experience to be less dependable. Expanding to include additional cases and surgeons will also be essential for proving the generalizability of our experience and findings.
In summary, lessons learned from Baghdad-KSA neuroendovascular teleproctoring included that teleproctoring accelerates the learning curve for the local neurosurgeon and simultaneity impacts the delivery of high-standard treatment in areas with limited resources. In BNC, seven patients were treated in the BNC center neuroendovascularly for various lesions using online proctoring with an assistant professor from Saudi Arabia. The post-procedural course of the seven patients was uneventful, and their follow-up period showed significant enhancement in their muscle power and level of consciousness. This experience consolidated the surgical team’s learning experience regarding neurointervention and ensured an excellent outcome for the patients. This experience can be replicated in areas with similar circumstances as it opens opportunities for future collaborations.
CONCLUSION
Within limited-resource areas, such as Iraq, there exists a significant demand for proctoring services. Our teleproctoring experience, facilitated by regular technology and fostering a high level of communication between the surgical team and the proctor, has demonstrated its potential to enhance the learning experience for all involved parties and generate positive outcomes for patients residing in resource-limited areas. This underscores the valuable role that teleproctoring can play in addressing the educational needs and health-care challenges faced by such regions.
Ethical approval
In Iraq, the institutional review committee is not there so the ethical approval from the institution manager, is received, number 13, dated February 11, 2022.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Artsen AM, Burkett LS, Duvvuri U, Bonidie M. Surgeon satisfaction and outcomes of tele-proctoring for robotic gynecologic surgery. J Robot Surg. 2022. 16: 563-8
2. Bechstein M, Elsheikh S, Wodarg F, Taschner CA, Hanning U, Buhk JH. Interhospital teleproctoring of endovascular intracranial aneurysm treatment using a dedicated live-streaming technology: First experiences during the COVID-19 pandemic. BMJ Case Rep. 2020. 13: e016722
3. Datta N, MacQueen IT, Schroeder AD, Wilson JJ, Espinoza JC, Wagner JP. Wearable technology for global surgical teleproctoring. J Surg Educ. 2015. 72: 1290-5
4. Erridge S, Yeung DK, Patel HR, Purkayastha S. Telementoring of surgeons: A systematic review. Surg Innov. 2019. 26: 95-111
5. Galvao Neto M, Jerez J, Brunaldi VO, Cabrera D, Benavides C, Moreno M. Learning process effectiveness during the COVID-19 pandemic: Teleproctoring advanced endoscopic skills by training endoscopists in endoscopic sleeve gastroplasty procedure. Obes Surg. 2021. 31: 5486-93
6. Gudelj M, Bruyère PJ, Tebache M, Collignon L, Lubicz B. Endovascular treatment of intracranial aneurysms: Initial experience in a low-volume center. J Belg Soc Radiol. 2020. 104: 19
7. Hanning U, Bechstein M, Kaesmacher J, Boulouis G, Chapot R, Andersson T. Remote training of neurointerventions by audiovisual streaming: Experiences from the European ESMINT-EYMINT E-Fellowship Program. Clin Neuroradiol. 2023. 33: 137-45
8. Hassan AE, Desai SK, Georgiadis AL, Tekle WG. Augmented reality enhanced tele-proctoring platform to intraoperatively support a neuro-endovascular surgery fellow. Interv Neuroradiol. 2022. 28: 277-82
9. Huang EY, Knight S, Guetter CR, Davis CH, Moller M, Slama E. Telemedicine and telementoring in the surgical specialties: A narrative review. Am J Surg. 2019. 218: 760-6
10. Ismail M, Talib SH, Albairmani S, Al-Khafaj AO, Al-Jehani H, Hoz SS. Coil migration during pressure-cooker technique for cerebral AVM: A case report. Roman Neurosurg. 2022. 36: 350-4
11. McCullough MC, Kulber L, Sammons P, Santos P, Kulber DA. Google glass for remote surgical tele-proctoring in low-and middle-income countries: A feasibility study from Mozambique. Plast Reconstr Surg Glob Open. 2018. 6: e1999
12. Nakhla J, Kobets A, De la Garza Ramos R, Haranhalli N, Gelfand Y, Ammar A. Use of google glass to enhance surgical education of neurosurgery residents: Proof-of-concept study. World Neurosurg. 2017. 98: 711-4
13. Orru’ E, Marosfoi M, Patel NV, Coon AL, Wald C, Repucci N. International teleproctoring in neurointerventional surgery and its potential impact on clinical trials in the era of COVID-19: Legal and technical considerations. J Neurointerv Surg. 2021. 13: 1022-6
14. Sachdeva AK. Preceptoring, proctoring, mentoring, and coaching in surgery. J Surg Oncol. 2021. 124: 711-21
15. Schulz CM, Endsley MR, Kochs EF, Gelb AW, Wagner KJ. Situation awareness in anesthesia: Concept and research. Anesthesiology. 2013. 118: 729-42
16. Wright MC, Taekman J, Endsley M. Objective measures of situation awareness in a simulated medical environment. Qual Saf Health Care. 2004. 13: i65-71