- Department of Surgery and Biomedical Sciences, Faculty of Medicine, Universitas Khairun, Ternate, Indonesia
Correspondence Address:
Aryandhito Widhi Nugroho, Department of Surgery and Biomedical Sciences, Faculty of Medicine, Universitas Khairun, Ternate, Indonesia. aryandhitowidhinugroho@ gmail.com
DOI:10.25259/SNI_929_2024
Copyright: © 2025 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Aryandhito Widhi Nugroho, Nur Upik En Masrika. The epidemiology of motorcycle-related acute traumatic brain injury: The NOMADEN study. 31-Jan-2025;16:27
How to cite this URL: Aryandhito Widhi Nugroho, Nur Upik En Masrika. The epidemiology of motorcycle-related acute traumatic brain injury: The NOMADEN study. 31-Jan-2025;16:27. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13358
Abstract
Background: Although persisting to be a public health hazard in Indonesia, motorcycle-related traumatic brain injury (TBI) due to road traffic accidents (RTA) lacks comprehensive national data. We aim to study the epidemiological pattern of motorcycle-related TBI and analyze the determinants related to mortality in the only neurosurgical center in the rural province of North Maluku, Indonesia.
Methods: Using the North Maluku Database in Neurosurgery register, information regarding age, sex, health insurance, alcohol use, point of referral, degree of severity, brain computed tomography abnormalities, helmet use, surgery, injury-to-admission time (IAT), and relationship to the motorcycle were obtained from patients admitted to Chasan Boesoirie General Hospital, Ternate, in 2021–2022. Multivariable logistic regression analysis was performed to investigate associations with in-hospital mortality.
Results: Of all RTA-related TBI patients (n = 353), 91.8% (n = 324) were caused by motorcycle collision (mean age ± standard deviation of 30.5 ± 16.7 years old). The majority were motorcyclists (66.7%), male (64.8%), IAT >4 h (55.9%), financed by non-Jaminan Kesehatan Nasional mechanism (66.4%), not under alcohol influence (78.4%), referred from Ternate (55.2%), and suffered mild TBI (75%). Thirty patients (9.3%) succumbed to death. Moreover, 9.3% and 91.2% were ≤17 years old and helmetless. Glasgow coma scale and IAT were significantly associated with in-hospital mortality (odds ratio [95% confidence interval]: 0.58 [0.49–0.68] and 5.44 [1.00–30.34], respectively).
Conclusion: The young and productive males dominated the motorcycle-related TBI patients in North Maluku. Poor compliance with road traffic laws, as demonstrated by a considerable proportion of underage, alcohol-intoxicated, and helmetless patients, necessitated prompt actions from all related elements.
Keywords: Epidemiology, Motorcycle, Traumatic brain injury, Rural area
INTRODUCTION
Traumatic brain injury (TBI) is defined as an acquired assault to the brain due to external force, ranging from a mild head blow (concussion) to a violent penetrating attack on the skull and brain parenchyma.[
In 2021, RTA was estimated to be responsible for 1.19 million injury deaths and the predominant cause of mortality among children and productive generations aged 5–29 years worldwide.[
As one of the SEA LMICs with a population of ±277 million people, the fourth highest in the world, Indonesia has to tackle the triple burden of communicable diseases, noncommunicable diseases, and road injuries.[
Considering the importance of sound scientific justification as the basis for future public health decision-making in the region, this study, a follow-up of the North Maluku Database in Neurosurgery (NOMADEN), aims to investigate the epidemiological pattern of motorcycle-related TBI and analyze the demographic determinants that may be related to mortality among TBI patients in this rural province in the eastern part of Indonesia.[
MATERIALS AND METHODS
Subjects
The NOMADEN is a single-center and hospital-based registry created to be the database for all neurosurgical cases in North Maluku, an archipelagic region in Indonesia populated by 1.2 million.[
DETERMINATION OF TBI
All diagnoses of TBI were made solely by the neurosurgeon as it is the hospital policy to refer all TBI cases from the emergency department to neurosurgical care. Brain computed tomography (CT) scans were performed according to the Canadian Head CT Rule.[
Variables and outcome
Information about age, sex, health insurance, suspected alcohol use, point of referral, degree of severity, brain CT abnormalities, helmet use, surgery, mechanism of injury, injury-to-admission time (IAT), vehicle type, and their relationship to the vehicle was obtained. Seventeen was selected as the age cutoff point since this is the minimum age for Indonesians to be legally granted motorcycle driving licenses.[
Statistical analysis
Initially, all characteristics were described and compared according to the mortality status, followed by a similar analysis of the most prevalent cause of RTA-related TBI. Continuous variables were presented as mean ± standard deviation (SD) or median (Interquartile range [IQR]), and categorical variables as proportions. District-based case distribution, causal mechanism, and IAT were graphically depicted, together with the overall surgical diagnoses and neurosurgical procedures performed. Uni- and multivariable logistic regression analyses were conducted to investigate any significant association between predictors and the study outcome. IBM Statistical Package for the Social Sciences version 25 software was used in all statistical analyses. A two-tailed P < 0.05 was determined to be statistically significant.
RESULTS
Overview of acute TBI patients
Characteristics of all RTA- and motorcycle-related acute TBI patients
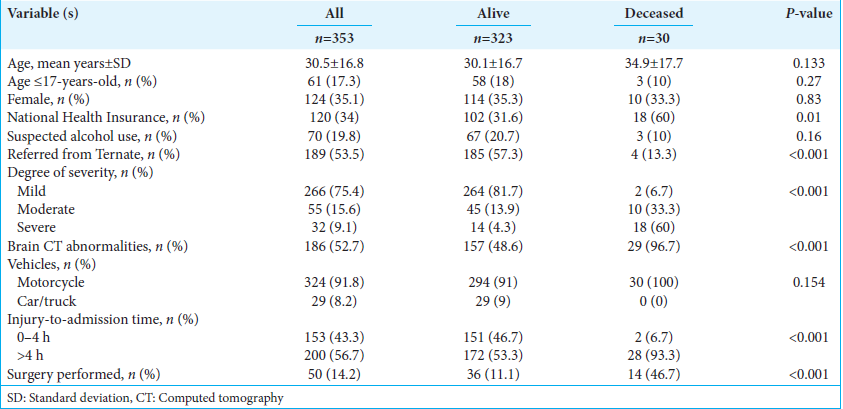
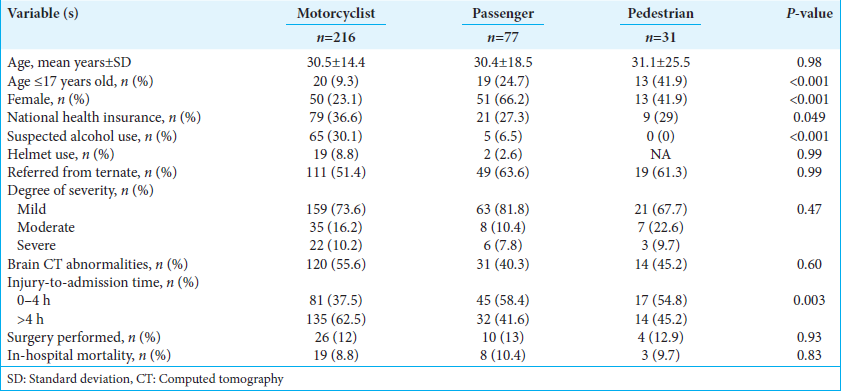
There were 353 patients admitted to the hospital following RTA [
Association between variables and in-hospital mortality
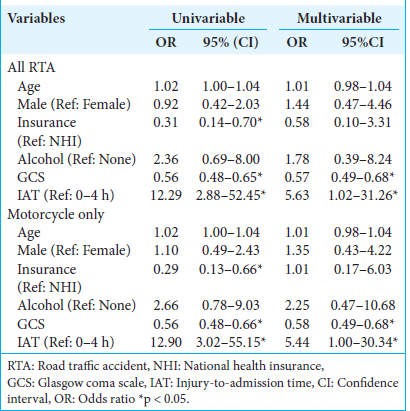
Among the RTA-related TBI patients, following uni- and multivariable analysis, GCS on admission (unadjusted odds ratio [OR] [95% confidence interval (CI)] of 0.56 [0.48–0.65] to multivariable-adjusted OR [95% CI] of 0.57 [0.49–0.68]) and IAT (unadjusted OR [95% CI] of 12.29 [2.88–52.45] to multivariable-adjusted OR [95% CI] of 5.63 [1.02–31.26] were found to be significantly associated with in-hospital mortality [
DISCUSSION
The efficiency and effectiveness of public health policy in reducing the burden of TBI depends on a thorough understanding of the disease’s epidemiology. Hitherto, the only national data source on TBI is the 2018 Basic Health Research study by the Indonesian Ministry of Health. According to this report, North Maluku was ranked ninth as the province with the highest TBI prevalence. Due to the dynamic and unique social, economic, cultural, and geographical circumstances around TBI epidemiology and management, a standard, upto-date, and real-world TBI registry tailored to every region in Indonesia is mandatory. As a response, we conducted a prospective cohort study of all motorcycle-related TBI patients managed at Dr. H. Chasan Boesoirie General Hospital in Ternate, North Maluku, Indonesia. Our main purpose was to elaborate on the epidemiology of motorcycle-related TBI, examine the determinants of in-hospital mortality among this particular group, and provide evidence-based suggestions for future policies to curtail this malady.
Similar to our finding, most, if not all, studies from other parts of Indonesia and other nations, particularly from LMICs, have identified male motorcyclists in their thirties, a productive population group, as the predominant group.[
Nearly a quarter of our motorcyclists and passengers were suspected of alcohol use. Alcohol has been shown to have a major role in global RTA, particularly in several LMICs.[
The 2018 Basic Health Research reported that about 23.9% of motorcyclists and passengers never/rarely wore helmets while commuting.[
Despite its success in attaining more than 90% coverage all across the country, the JKN, as Indonesia’s official universal healthcare coverage scheme, has limited utilization for RTA patients.[
The proportion of mild TBI in our study is higher than in two other Indonesian-based studies that included patients with all levels of consciousness during admission.[
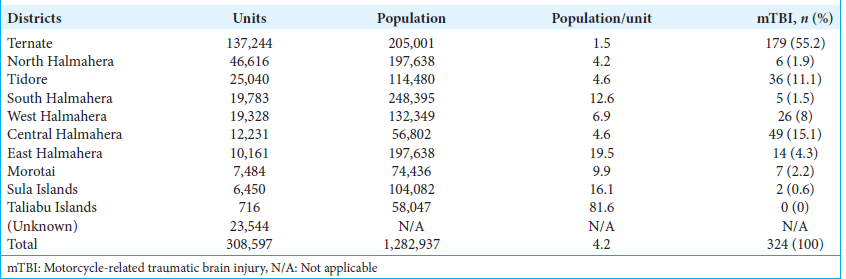
Less than half of all patients in the study were referred from outside Ternate. No patients were even recorded from Taliabu, the most distant district. The authors postulate several conditions that may complicate neurosurgical patient transfer in the region: (i) the challenging geographical situation of North Maluku, comprising 69% ocean and 805 islands, (ii) the differing distance of each district to the neurosurgery service from the nearest (Tidore, 14.2 km) to the farthest (Taliabu, 449.3 km), (iii) the worst road condition in areas outside Ternate, which were moderate-to-severely damaged in 56.4% of the total road, compared to those in Ternate that reached 19.9%, and (iv) the lack of neurosurgeons and their supporting facilities. These circumstances present serious challenges to improving the management of TBI in North Maluku and necessitate comprehensive cooperation from all related elements.
Underage motorcyclists are of particular concern. The Indonesian Law No. 22 of 2009 on Traffic and Road Transportation defines 17 years old as the minimum age for obtaining a driving license. Nevertheless, this study managed to identify that one per-tenth of all motorcyclists were underage. Of all underage motorcycle-related TBI patients, 38.5% were motorcyclists, and none wore helmets. Several underlying sociocultural and neuroscience factors may be responsible. Young motorcyclists are more overly confident, sensation-seeking, craving social acceptance, and impatient than older ones.[
The GCS has long been known as a simple, valid, and reproducible clinical tool to determine the severity of TBI ever since its introduction in 1974 by neurosurgery professors Teasdale and Jennett.[
High motorcycle volume is one of the profound challenges faced in reducing the burden of TBI due to RTA. Motorcycles are the primary means of land transportation in Indonesia. According to the Traffic Corps National Police Republic Indonesia data, by the end of February 2023, motorcycle volume has reached 127,976,339 units or 87% of all means of land transportation.[
Table 4:
The volume of motorcycle units, population, and population/motorcycle unit ratio across North Maluku districts in 2023, and the incidence of mTBI in this study.[
As the first attempt to map TBI incidence in the region, the authors realize that future development is necessary to enhance the register’s functionality and generalizability. Regionally, international collaboration and standardization with renowned TBI registries, namely, the International TBI Research and the Global Epidemiology and Outcomes following TBI registry, will benefit the people of North Maluku.[
Limitations
Apart from the drawbacks mentioned earlier in this study and our primary study, particular limitations are critical to note. Precise information on the type of motorcycles involved in the RTA, for example, small versus large engines, new versus used, and the form of collision, for example, motorcycle versus motorcycle, motorcycle versus car collision, were not obtained. Lists of the healthcare facilities visited, and the transportation modes utilized before reaching our facility were absent. Other related abnormalities in the brain CT during the 1st year of the study might be overlooked due to the shortage of radiologists. Finally, due to poor recording of medical records, the actual duration from patients’ arrival until the administration of definite care was unavailable.
CONCLUSION
Our study presents the epidemiology pattern of TBI caused by motorcycle RTAs and the variables associated with inhospital mortality in the only neurosurgical center in Ternate, North Maluku. In general, the dominant characteristics of the study population were male motorcyclists around their thirties who did not wear helmets, paid their medical expenses using the non-JKN mechanism, suffered accidents in/referred from Ternate, diagnosed with mild TBI, and arrived at the hospital in >4 h after injury. IAT and GCS on admission were significantly related to both in-hospital mortality among RTA-related and motorcycle-related TBI patients. Of particular attention, one per-tenth of motorcyclists were <17 years old, a group forbidden by law to operate motor vehicles. These are hard evidence for a major overhaul of road safety in North Maluku. Improved medical service capacity, better governance, reinforced law, and persistent education to society are imperative. Finally, neurosurgeons are obliged to take the battle to reduce the burden of TBI outside of the operating theater and actively participate in deciding the best policy for TBI management.
Ethical approval
Ethical clearance for this study has been obtained from the Institutional Review Board, Universitas Khairun (No. 57/UN27.06.11/KEP/EC/2023). The approval date of the ethical clearance is November 6th 2023.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
The Higher Education Outstanding and Competitive Research grant for Khairun University No. 606/PENPKUPT/UN44.C9/2023.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Ahmad S, Rehman L, Afzal A, Javeed F. Outcome of head injury in motorbike riders. Pak J Med Sci. 2023. 39: 390-4
2. Ahmadi S, Sarveazad A, Babahajian A, Ahmadzadeh K, Yousefifard M. Comparison of Glasgow Coma Scale and Full Outline of UnResponsiveness score for prediction of in-hospital mortality in traumatic brain injury patients: A systematic review and meta-analysis. Eur J Trauma Emerg Surg. 2023. 49: 1693-706
3. Ahmed N, Kuo YH, Sharma J, Kaul S. Elevated blood alcohol impacts hospital mortality following motorcycle injury: A National Trauma Data Bank analysis. Injury. 2020. 51: 91-6
4. Ashraf M, Ashraf N. Underage motorbike driving in Pakistan: A neurosurgical burden heading towards societal disaster. Surg Neurol Int. 2022. 13: 37
5. Banerjee A, Finkelstein A, Hanna R, Olken BA, Ornaghi A, Sumarto S. The challenges of universal health insurance in developing countries: Evidence from a large-scale randomized experiment in Indonesia. TWERPS. 2019. 111: 37
6. Barthélemy EJ, Spaggiari R, Corley J, Lepard JR, Staffa SJ, Iv V. Injury-to-admission delay beyond 4 hours is associated with worsening outcomes for traumatic brain injury in Cambodia. World Neurosurg. 2019. 126: e232-40
7. Basak D, Chatterjee S, Attergrim J, Sharma MR, Soni KD, Verma S. Glasgow coma scale compared to other trauma scores in discriminating in-hospital mortality of traumatic brain injury patients admitted to urban Indian hospitals: A multicentre prospective cohort study. Injury. 2023. 54: 93-9
8. Bhattarai HK, Bhusal S, Barone-Adesi F, Hubloue I. Prehospital emergency care in low-and middle-income countries: A systematic review. Prehosp Disaster Med. 2023. 38: 495-512
9. Breeding T, Martinez B, Katz J, Nasef H, Santos RG, Zito T. The Association between gender and clinical outcomes in patients with moderate to severe traumatic brain injury: A systematic review and meta-analysis. J Surg Res. 2024. 295: 791-9
10. Capizzi A, Woo J, Verduzco-Gutierrez M. Traumatic brain injury: An overview of epidemiology, pathophysiology, and medical management. Med Clin North Am. 2020. 104: 213-38
11. Chu MY, Law TH, Hamid H, Law SH, Lee JC. Examining the effects of urbanization and purchasing power on the relationship between motorcycle ownership and economic development: A panel data. Int J Transp Sci Technol. 2020. 11: 72-82
12. Clarke DD, Ward P, Bartle C, Truman W. The role of motorcyclist and other driver behaviour in two types of serious accident in the UK. Accid Anal Prev. 2007. 39: 974-81
13. Dewan MC, Rattani A, Gupta S, Baticulon RE, Hung YC, Punchak M. Estimating the global incidence of traumatic brain injury. J Neurosurg. 2019. 130: 1080-97
14. Faried A, Bachani AM, Sendjaja AN, Hung YW, Arifin MZ. Characteristics of moderate and severe traumatic brain injury of motorcycle crashes in Bandung, Indonesia. World Neurosurg. 2017. 100: 195-200
15. Georges A, Das JM, editors. Traumatic brain injury (archive). StatPearls. Treasure Island, FL: StatPearls Publishing; 2024. p. Available from: https://pubmed.ncbi.nlm.nih.gov/29083790/ [Last accessed on 2024 Nov 01]
16. Giedd JN. The digital revolution and adolescent brain evolution. J Adolesc Health. 2012. 51: 101-5
17. Gjerde H, Huestis MA, Mulima G, Kajombo C, Sundet M, Pechansky F. Recommendations for effective collaboration and capacity building in epidemiological studies on the effect of alcohol and drug use on traffic safety in low-and middle-income countries. Traffic Inj Prev. 2024. 25: 313-21
18. Gomez D, Haas B, de Mestral C, Sharma S, Hsiao M, Zagorski B. Gender-associated differences in access to trauma center care: A population-based analysis. Surgery. 2012. 152: 179-85
19. Guan B, Anderson DB, Chen L, Feng S, Zhou H.. A systematic analysis for the Global Burden of Disease Study 2019. BMJ Open. 2023. 13: e075049
20. Harmon KJ, Marshall SW, Proescholdbell SK, Naumann RB, Waller AE. Motorcycle crash-related emergency department visits and hospitalizations for traumatic brain injury in North Carolina. J Head Trauma Rehabil. 2015. 30: 175-84
21. Heydari S, Hickford A, McIlroy R, Turner J, Bachani AM. Road safety in low-income countries: state of knowledge and future directions. Sustainability. 2019. 11: 6249
22. Hooley B, Afriyie DO, Fink G, Tediosi F. Health insurance coverage in low-income and middle-income countries: Progress made to date and related changes in private and public health expenditure. BMJ Glob Health. 2022. 7: e008722
23. Indonesian Ministry of Finance. Peraturan menteri keuangan republik Indonesia nomor 141/PMK.02/2018 tentang koordinasi antar penyelenggara jaminan dalam pemberian manfaat pelayanan kesehatan, Jakarta. Available from: https://peraturan.bpk.go.id/Details/113358/pmk-no-141pmk022018 [Last accessed on 2024 Nov 01].
24. Indonesian Ministry of Health. Basic Health Research 2018. Available from: https://layanandata.kemkes.go.id/katalog-data/riskesdas/ketersediaan-data/riskesdas-2018 [Last accessed on 2024 Nov 02].
25. Joannides AJ, Korhonen TK, Clark D, Gnanakumar S, Venturini S, Mohan M. Consensus-Based development of a global registry for traumatic brain injury: Establishment, protocol, and implementation. Neurosurgery. 2024. 94: 278-88
26. Kim CY, Wiznia DH, Averbukh L, Dai F, Leslie MP. The economic impact of helmet use on motorcycle accidents: A systematic review and meta-analysis of the literature from the past 20 years. Traffic Inj Prev. 2015. 16: 732-8
27. Korps Lalu Lintas Kepolisian Negara Republik Indonesia. Jumlah data kendaraan di Kepolisian Daerah Maluku Utara. Available from: http://rc.korlantas.polri.go.id:8900/eri2017/laprekappolda.php [Last accessed on 2024 Nov 02].
28. Korps Lalu Lintas Kepolisian Negara Republik Indonesia. Undang-undang Republik Indonesia no. 22 Tahun 2009 tentang lalu lintas dan angkutan jalan. Available from: https://pusdiklantas.polri.go.id/web/index.php/perundang-undangan-lalulintas [Last accessed on 2024 Nov 02].
29. Kortbeek JB, Al Turki SA, Ali J, Antoine JA, Bouillon B, Brasel K, editors. Advanced trauma life support, 8th edition the evidence for change. J Trauma. 2008. 64: 1638-50
30. Laksono AD, Wulandari RD, Rohmah N, Rukmini R, Tumaji T. Regional disparities in hospital utilisation in Indonesia: A cross-sectional analysis data from the 2018 Indonesian Basic Health Survey. BMJ Open. 2023. 13: e064532
31. Maas AIR, Menon DK, Manley GT, Abrams M, Åkerlund C, Andelic N. Traumatic brain injury: Progress and challenges in prevention, clinical care, and research. Lancet Neurol. 2022. 21: 1004-60
32. Meara JG, Leather AJ, Hagander L, Alkire BC, Alonso N, Ameh EA. Global Surgery 2030: Evidence and solutions for achieving health, welfare, and economic development. Lancet. 2015. 386: 569-624
33. Mediratta S, Lepard JR, Barthélemy EJ, Corley J, Park KB. Barriers to neurotrauma care in low-to middle-income countries: An International Survey of Neurotrauma providers. J Neurosurg. 2022. 137: 789-98
34. Niryana IW, Junior IW, Darmawan R, Widyadharma IP. Characteristics of traumatic brain injury in Sanglah hospital, Bali, Indonesia: A retrospective study. Biomed Pharmacol J. 2020. 13: 3
35. Noya F, Carr S, Thompson S, Clifford R, Playford D. Factors associated with the rural and remote practice of medical workforce in Maluku Islands of Indonesia: A cross-sectional study. Hum Resour Health. 2021. 19: 126
36. Nugroho AW. The start-up of a neurosurgical service in an East Indonesian archipelagic province: The first 2-year experience of North Maluku Database in Neurosurgery (NOMADEN). Surg Neurol Int. 2024. 15: 53
37. Okruhlica L, Slezakova S. Clinical signs of alcohol intoxication and importance of blood alcohol concentration testing in alcohol dependence. Bratisl Lek Listy. 2013. 114: 136-9
38. Oliveira TA, Andrade SM, Prado GO, Fernandes RB, Gusmão MS, Gomes EGF. Epidemiology of spine fractures in motorcycle accident victims. Columna. 2016. 15: 65-7
39. Ong HB, Wasiuzzaman S, Chong LL, Choon SW. Digitalisation and financial inclusion of lower middle-income ASEAN. Heliyon. 2023. 9: e13347
40. Peters R. Motorbike-taxi-drivers as infrastructure in the Indonesian City. Ethnos. 2019. 85: 471-90
41. Prawiroharjo P, Pangeran D, Supriawan H, Lastri D, Mayza A, Zairinal RA. Increasing traumatic brain injury incidence during COVID-19 pandemic in the emergency department of Cipto Mangunkusumo National General Hospital-a national referral hospital in Indonesia. Neurology. 2020. 95: S11
42. Raharja J. Jumlah santunan. Available from: https://www.jasaraharja.co.id [Last accessed on 2024 Nov 01].
43. Riany YE, Meredith P, Cuskelly M. Understanding the influence of traditional cultural values on Indonesian parenting. Marriage Fam Rev. 2016. 53: 207-26
44. Romero DL, de Barros DM, Belizario GO, Serafim AP. Personality traits and risky behavior among motorcyclists: An exploratory study. PLoS One. 2019. 14: e0225949
45. Rosyidi RM, Priyanto B, Laraswati NK, Islam AA, Hatta M, Bukhari A. Characteristics and clinical outcome of traumatic brain injury in Lombok, Indonesia, Interdiscip Neurosurg. 2019. 18: 100470
46. Rosyidi RM, Wisnu Wardhana DP, Apriawan T, Al Fauzi A, Priyanto B, Gunawan K. Algorithm of traumatic brain injury management at Indonesia in the COVID 19 pandemic ERA. Retrospective cohort study. Ann Med Surg (Lond). 2021. 62: 98-103
47. Rubiano AM, Vera DS, Montenegro JH, Carney N, Clavijo A, Carreño JN. Recommendations of the Colombian Consensus Committee for the management of traumatic brain injury in Prehospital, Emergency Department, Surgery, and Intensive Care (Beyond One option for treatment of traumatic brain injury: A stratified protocol [BOOTStraP]). J Neurosci Rural Pract. 2020. 11: 7-22
48. Stiell IG, Wells GA, Vandemheen K, Clement C, Lesiuk H, Laupacis A. The Canadian CT head rule for patients with minor head injury. Lancet. 2001. 357: 1391-6
49. Tangkudung E, Ernani B. Motorcycle helmet situation in Indonesia. EASTS. 2009. 7: 1-12
50. Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974. 2: 81-4
51. Valadka AB, Narayan RK, editors. Emergency room management of the head-injured patient. Neurotrauma. New York: McGraw-Hill; 1996. p. 120
52. Weil ZM, Corrigan JD, Karelina K. Alcohol use disorder and traumatic brain injury. Alcohol Res. 2018. 39: 171-80
53. Widayanti AW, Green JA, Heydon S, Norris P. Health-seeking behavior of people in Indonesia: A narrative review. J Epidemiol Glob Health. 2020. 10: 6-15
54. Wong JT, Chung YS, Huang SH. Determinants behind young motorcyclists’ risky riding behavior. Accid Anal Prev. 2010. 42: 275-81
55. World Health Organization. Global health estimates: Leading causes of death, cause-specific mortality, 2000-2021. Available from: https://www.who.int [Last accessed on 2024 Nov 01].
56. World Health Organization. Global status report on road safety 2023. Available from: https://iris.who.int/handle/10665/375016 [Last accessed on 2024 Nov 01].
57. World Health Organization. Indonesia’s success in achieving 90 percent coverage and minimizing out-of-pocket expenses through national health insurance expansion. Available from: https://www.who.int [Last accessed on 2024 Nov 01].
58. World Health Organization. Road traffic injuries. Available from: https://www.who.int/news-room/fact-sheets/detail/road-traffic-injuries [Last accessed on 2024 Nov 01].