- Department of Neurosurgery, Izumi Regional Hospital, Kagoshima, Japan,
- Department of Radiology, Izumi Regional Hospital, Kagoshima, Japan,
- Department of Neurology, Uchiyama Hospital, Akune, Kagoshima, Japan,
- Department of Neurologic Surgery, Mayo Clinic, Rochester, Minnesota, United States,
- Department of Neurosurgery, Kagoshima University, Sakuragaoka, Kagoshima, Japan.
Correspondence Address:
Kazunori Arita
Department of Neurosurgery, Izumi Regional Hospital, Kagoshima, Japan,
Department of Neurosurgery, Kagoshima University, Sakuragaoka, Kagoshima, Japan.
DOI:10.25259/SNI_423_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Tomohisa Okada1, Kaisei Makimoto2, Kayoko Itoh3, FM Moinuddin4, Koji Yoshimoto5, Kazunori Arita1,5. The first 3-D volumetric analysis of mesencephalothalamic giant perivascular spaces showing steady and slow growth over 17 years. 18-Sep-2020;11:300
How to cite this URL: Tomohisa Okada1, Kaisei Makimoto2, Kayoko Itoh3, FM Moinuddin4, Koji Yoshimoto5, Kazunori Arita1,5. The first 3-D volumetric analysis of mesencephalothalamic giant perivascular spaces showing steady and slow growth over 17 years. 18-Sep-2020;11:300. Available from: https://surgicalneurologyint.com/surgicalint-articles/10262/
Abstract
Background: Giant perivascular spaces (PVSs) are very rare condition in the brain and can be associated with neurological symptoms. It often enlarges and causes obstructive hydrocephalus which requires surgical intervention. However, the growth velocity has never been investigated.
Case Description: Here, we report a woman in her early eighties with giant PVSs eventually followed up 17 years. She presented with dizziness and mild headache for a week and her neurological examination showed no abnormality. Her brain magnetic resonance imaging (MRI) showed a multiple cystic lesion, 28 mm in maximum diameter as a whole, in the left mesencephalothalamic region. There were no solid part, rim enhancement, or perilesional intensity change suggesting edema or gliosis. Smaller PVSs were also seen in bilateral-hippocampi, basal ganglia, white matter, and left frontal operculum. Retrospectively, five MRI studies over 17 years were analyzed using a 3-D volumetric software and found a very slow growth of the lesion, from 6.54 ml to 9.83 ml indicating gain of 0.1752 ml (2.68%) per year.
Conclusion: This is the first report verifying a gradual enlargement of giant PVSs in a natural course. The prospective 3-D volumetric analysis on PVSs may elucidate the true nature of these lesions.
Keywords: Giant perivascular spaces, Growth, Midbrain, Thalamus
INTRODUCTION
Perivascular spaces (PVSs) or Virchow-Robin spaces are pial-lined structures surrounding the vessels filled with interstitial/extracellular fluid. They are believed to serve as a lymphatic drainage pathway in the brain and play a significant role in the immune system in the brain.[
PVSs are more commonly seen in three locations.[
CASE REPORT
An woman in her early eighties was referred to the department of neurosurgery, Izumi Regional Hospital, Japan from a neurologist on June 2020. She was a known case of cystic brain lesion since 2003. She presented with mild headache and dizziness for a week. The patient’s history included diabetes and hypertension over 20 years. No abnormality was found on neurological examination including eye movement or cerebellar function.
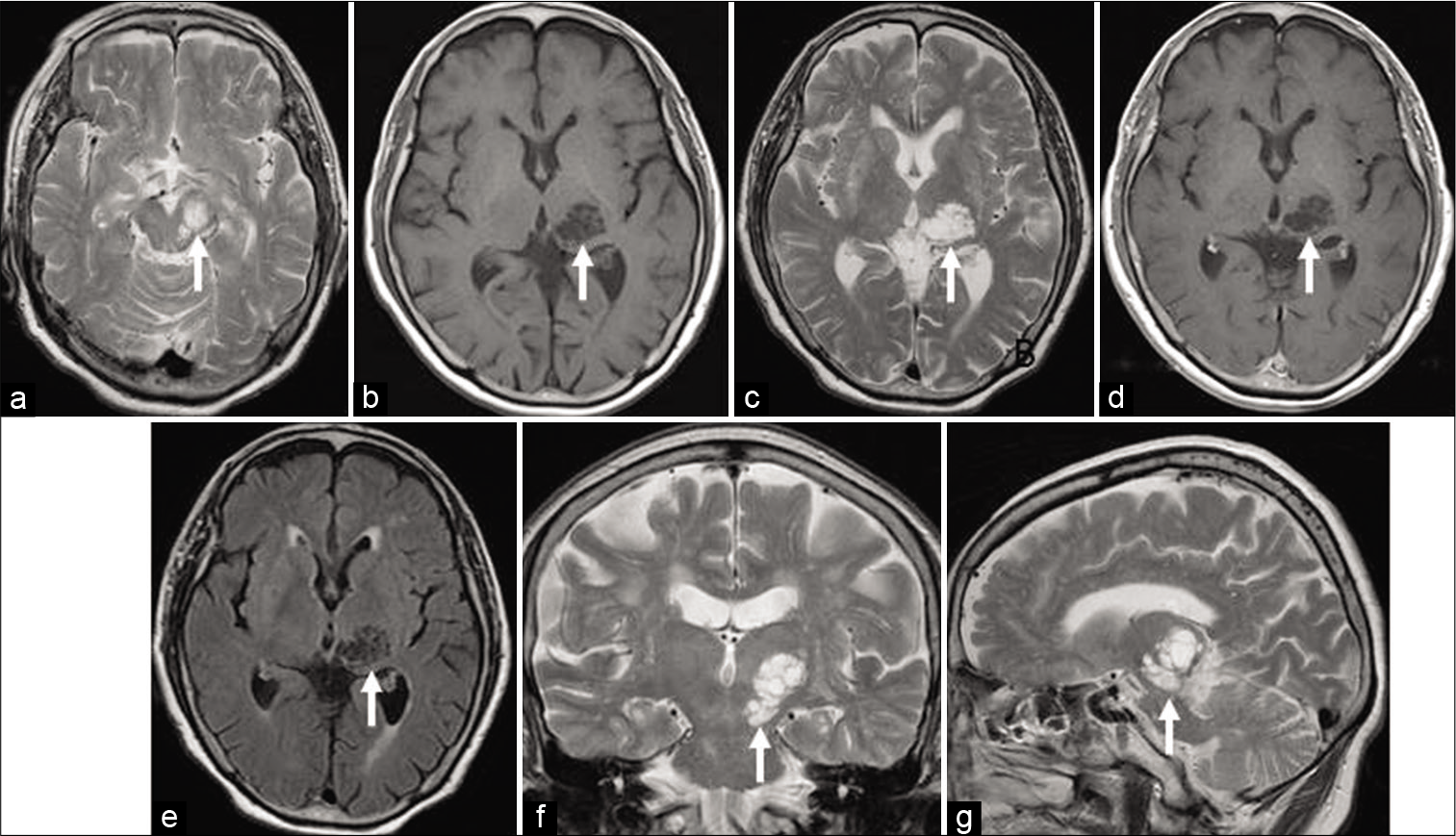
MRI on June 2020 showed a cluster of cystic lesion, 28 mm in diameter as whole, in the left mesencephalothalamic region [
Figure 1:
Magnetic resonance image (MRI) of giant perivascular spaces (PVSs) (arrows). (a) Axial T2-weighted image (T2WI) at the level of midbrain. (b-e) Axial images at the level of thalamus. (b) T1WI, (c) T2WI, (d) postgadolinium T1WI, (e) fluid-attenuated inversion recovery image. (f) Coronal T2WI. (g) Sagittal T2WI.
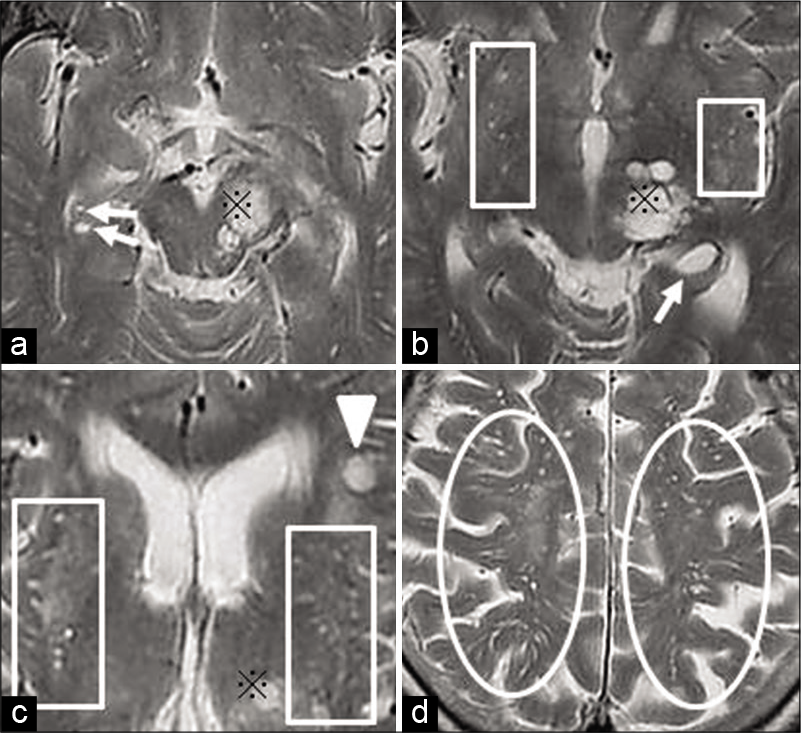
Figure 2:
Enlarged PVSs in other locations. ※: Part of the giant PVSs in the mesencephalothalamic region. (a) Right hippocampus (arrows). (b) Bilateral basal ganglia (boxes) and left hippocampus (arrow). (c) Bilateral basal ganglia (boxes) and left frontal operculum (arrowhead). (d) Subcortical white matter (circles).
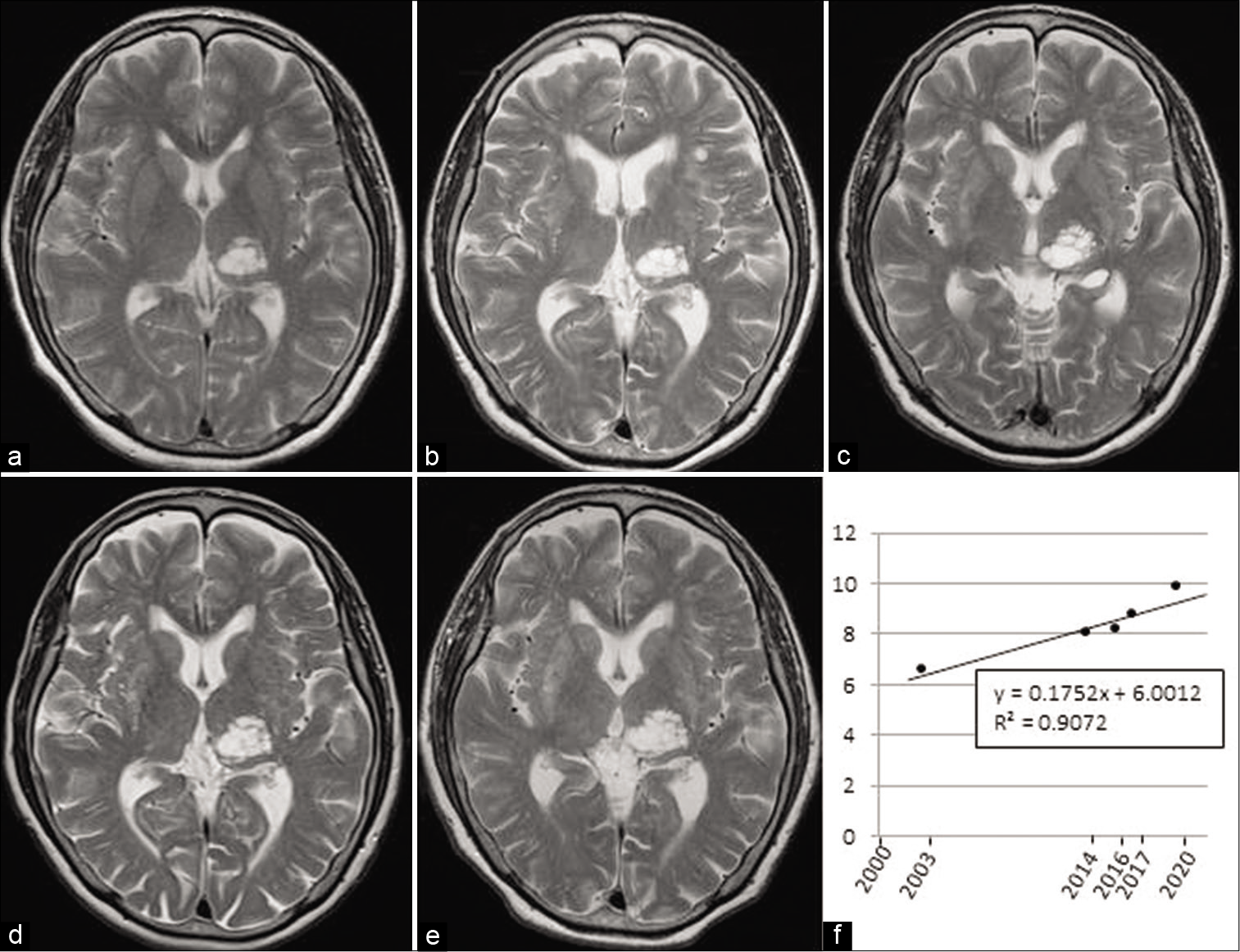
Figure 3:
Chronological changes in the volume of the giant perivascular spaces. (a) September 2003: 6.54 ml. (b) May 2014: 8.05 ml. (c) February 2016: 8.19 ml. (d) July 2017: 8.79 ml. (e) June 2020: 9.83 ml. (f) 3D volumetric analysis showing steady and slow growth with gentle slope of linear function: y (ml) = 0.1752x+6.0012, R2=0.9072.
The patient is now scheduled to have another MRI study 2 years later for early detection of symptomatic enlargement including obstructive hydrocephalus resulting from aqueductal stenosis.
DISCUSSION
Giant PVSs or tumefactive PVSs are very rare lesion in the brain commonly found in mesencephalothalamic region in the territory of the paramedical mesencephalothalamic artery and in the cerebral white matter.[
Pathologies mimicking giant PVSs include pilocytic astrocytomas, gangliogliomas, pleomorphic xanthoastrocytomas, and intraparenchymal schwannoma.[
Some rare infectious process results in multiple cyst formation.[
Although some giant PVSs must have grown to be symptomatic, no interim change was seen on repeat MRI in 17 cases in which follow-up MRI was studied 4.1 ± 3.7 (mean ± SD) years after the initial scan in Salzmann’s series.[
The exact etiology of giant PVS enlargement remains unknown, although several possible mechanisms have been suggested in the literature.[
This is the first ever reported case showing very gradual enlargement of giant PVSs in a natural course. It has grown steadily by 0.1752 ml/year over 17 years from initial of 6.54 ml. The volume increase rate was 2.68%/year.
Data accumulation of 3-D volumetric analysis may elucidate the true nature of the giant PVSs, which may support to predict the symptomatic growth of incidentally found PVSs.
CONCLUSION
We demonstrated the very slow but steady growth of giant PVSs in the mesencephalothalamic region based on longitudinal MRI follow-up. Data accumulation of 3-D volumetric analysis may elucidate the true nature of the giant PVSs, which may support to predict the symptomatic growth of incidentally found PVSs.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
The authors would like to thank Haibunsha Kagoshima for English editing.
References
1. Al Abdulsalam H, Alatar AA, Elwatidy S. Giant tumefactive perivascular spaces: A case report and literature review. World Neurosurg. 2018. 112: 201-4
2. Esiri MM, Gay D. Immunological and neuropathological significance of the Virchow-Robin space. J Neurol Sci. 1990. 100: 3-8
3. Fujimoto K, Kuroda J, Hide T, Hasegawa Y, Yano S, Kuratsu J. Giant tumefactive perivascular spaces that expanded and became symptomatic 14 years after initial surgery. Surg Neurol Int. 2012. 3: 127
4. Heier LA, Bauer CJ, Schwartz L, Zimmerman RD, Morgello S, Deck MD. Large Virchow-Robin spaces: MR-clinical correlation. AJNR Am J Neuroradiol. 1989. 10: 929-36
5. Kwee RM, Kwee TC. Virchow-Robin spaces at MR imaging. Radiographics. 2007. 27: 1071-86
6. Mascalchi M, Salvi F, Godano U, Nistri M, Taiuti R, Tosetti M. Expanding lacunae causing triventricular hydrocephalus. Report of two cases. J Neurosurg. 1999. 91: 669-74
7. McKinney AM.editors. Dilated perivascular spaces. Atlas of Normal Imaging Variations of the Brain Skull, and Craniocervical Vasculature. Cham, Switzerland: Springer; 2017. 1: 315-481
8. Muzzafar S, Ketonen L, Weinberg JS, Schellingerhout D. Imaging and clinical features of an intra-axial brain stem schwannoma. AJNR Am J Neuroradiol. 2010. 31: 567-9
9. Poirier J, Barbizet J, Gaston A, Meyrignac C. Thalamic dementia, Expansive lacunae of the thalamo-paramedian mesencephalic area, Hydrocephalus caused by stenosis of the aqueduct of Sylvius. Rev Neurol (Paris). 1983. 139: 349-58
10. Rudie JD, Rauschecker AM, Nabavizadeh SA, Mohan S. Neuroimaging of dilated perivascular spaces: From benign and pathologic causes to mimics. J Neuroimaging. 2018. 28: 139-49
11. Salzman KL, Osborn AG, House P, Jinkins JR, Ditchfield A, Cooper JA. Giant tumefactive perivascular spaces. AJNR Am J Neuroradiol. 2005. 26: 298-305
12. Schley D, Carare-Nnadi R, Please CP, Perry VH, Weller RO. Mechanisms to explain the reverse perivascular transport of solutes out of the brain. J Theor Biol. 2006. 238: 962-74
13. Weller RO, Djuanda E, Yow HY, Carare RO. Lymphatic drainage of the brain and the pathophysiology of neurological disease. Acta Neuropathol. 2009. 117: 1-14