- HEAVEN/GEMINI International Collaborative Group, Turin, Italy
- Neurosurgery Department, Sklifosovsky Clinical and Research Institute for Emergency Medicine, Moscow, Russian Federation
- College of Veterinary Medicine, Konkuk University, Seoul, Republic of Korea
Correspondence Address:
Sergio Canavero, MD HEAVEN/GEMINI International Collaborative Group, Turin, Italy.
DOI:10.25259/SNI_945_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Canavero S1, Lebenstein-Gumovski MV2, Kim C3. The rise of transplantation neurosurgery: Spinal cord, eye, brain. Surg Neurol Int 27-Dec-2024;15:478
How to cite this URL: Canavero S1, Lebenstein-Gumovski MV2, Kim C3. The rise of transplantation neurosurgery: Spinal cord, eye, brain. Surg Neurol Int 27-Dec-2024;15:478. Available from: https://surgicalneurologyint.com/surgicalint-articles/13304/
TO THE MEMORY OF VD DEMIKHOV (1916–1998)
Since 1954, almost any organ or tissue or body part of the human body has been transplanted, with the notable exception of the central nervous system (CNS).[
Nerve fusion technology developed over the past 40 years, including the GEMINI SC fusion (SCF) protocol,[
MENDING NEURAL DAMAGE
The GEMINI SCF protocol, first introduced in 2013, has been reviewed in depth in several publications to which the interested reader is referred (e.g., Canavero et al. and Canavero and Ren[
GEMINI exploits the rapid application of special substances that act as Fusogens or Sealants (e.g., Polyethylene Glycol [PEG] and Chitosan) (reviewed in Ryan and Henderson[
The final result is further accelerated by combined electrical stimulation (ES) of the SC overlying the fusion interface and the primary motor cortex (M1). This can be effected either invasively by positioning electrodes over MI and the SC or noninvasively by combining Transcranial Magnetic Stimulation of MI and simultaneous Trans Spinal Direct Current Stimulation. Protocols already exist.[
During SC, eye, and brain transplantation, cranial nerves and spinal roots will have to be reconnected. The olfactory nerve and the ON, unlike the other ten cranial nerves and the spinal roots, are considered to be extensions of the CNS because oligodendrocytes myelinate them, whereas the ten other cranial nerves and the spinal roots are myelinated by Schwann cells.[
As such, one would consider standard microsurgical suturing of these nerves as the preferred option. Unfortunately, as De Medinaceli, the surgeon who introduced the concept of cell surgery for the repair of peripheral nerves in the 1970s, noted: [
Starting with Bittner’s demonstration in 1986 that a severed axon can be refused with PEG, the promise of fusogens in restoring lost function after peripheral nerve section is becoming a clinical reality (reviewed in Bittner et al.[
SCT
As is well known, SCI is generally due to localized tissue disruption at C4–5 or T11–12; multilevel injuries are a distinct minority.[
The feasibility of SCT has been confirmed recently. A Chinese group[
However, this study has several shortcomings. First, the time to revascularize the transplanted segment was 2 h, during which ischemia exerts deleterious effects. Although extreme damage is seen at 4 h, 2 h is still excessive.[
In light of these data, a human trial of SCT incorporating the above suggestions is warranted. Actually, over the past few decades, attempts have been made to remove the damaged segment of the cord and replace it with segments of peripheral nerves, e.g., the sural nerve, both in animals and men, with some level of recovery. However, it was only with the deployment of fusogens that a recent study in swine led to remarkable motor recovery in animals[
EYE TRANSPLANTATION
On May 27, 2023, a human eye transplantation took place as part of a facial transplant.[
The combined whole eye and face transplant procedure commenced with donor and recipient surgical procedures performed simultaneously in adjacent operating rooms. Induction immunosuppression was initiated with thymoglobulin and rituximab. Among other steps, the left-sided vascular dissection in the donor also included harvesting a long anterior branch of the superficial temporal artery and vein in continuity with the left external carotid and internal jugular vascular system. This was followed by entry into the cranial vault and orbital dissection with identification of the ophthalmic artery, internal carotid artery, ophthalmic veins, and the motor nerves to the extraocular muscles. The ON was dissected all the way back to the optic chiasm, where it was divided. The origins of the ophthalmic artery and superior ophthalmic vein were then each divided and anastomosed to the left superficial temporal artery and vein, respectively. Significant back bleeding from the divided ophthalmic artery end, which was attached to the eye, suggested significant collateral flow and, hence, oxygenation to the retina, likely from branches of the facial artery. Total warm ischemia time (or low flow) from division to completion of the anastomosis was 25 min. Robust perfusion of the anterior and posterior tissues of the allograft, including the globe, was confirmed. The allograft anastomosis of the superficial temporal artery to the ophthalmic artery was intact. Concurrently, after isolation of the recipient vessels for allograft anastomosis and resection of craniofacial bone, the orbit of the recipient was debrided of scarred tissue, and the intraorbital ON end was identified and dissected free up to the optic canal. The allograft was then brought into the recipient field, followed by bony fixation of the geniotomy segment and coaptation of the ON ends with interrupted 8–0 nylon epineural sutures through the nerve sheath. Prior traumatic injury, subsequent enucleation, and resultant scar precluded precise fascicular alignment to the recipient ON end. Previously processed donor-derived CD34+ enriched bone marrow stem/progenitor fraction was then directly injected into the ON epineurium proximal and distal to the coaptation as a neuroprotectant. The allograft was then revascularized, and the remainder of the allograft components were attached to the recipient in a standard fashion. Total cold ischemia time for the facial allograft (and of the retina) was 2 h 59 min, with a total operative time of approximately 21 h. Postoperative maintenance immunosuppression consisted of standard triple therapy with tacrolimus, mycophenolate mofetil, and prednisone with infectious prophylaxis.
In reality, this cannot be construed as the first true human eye transplantation but more like a surgical experiment, as the nerves were not functionally reconnected. Actually, the first such experiment took place in Paris on May 5, 1885, when Chibret transplanted a rabbit eye to a young girl who had lost her left eye. No return of sight was mentioned.[
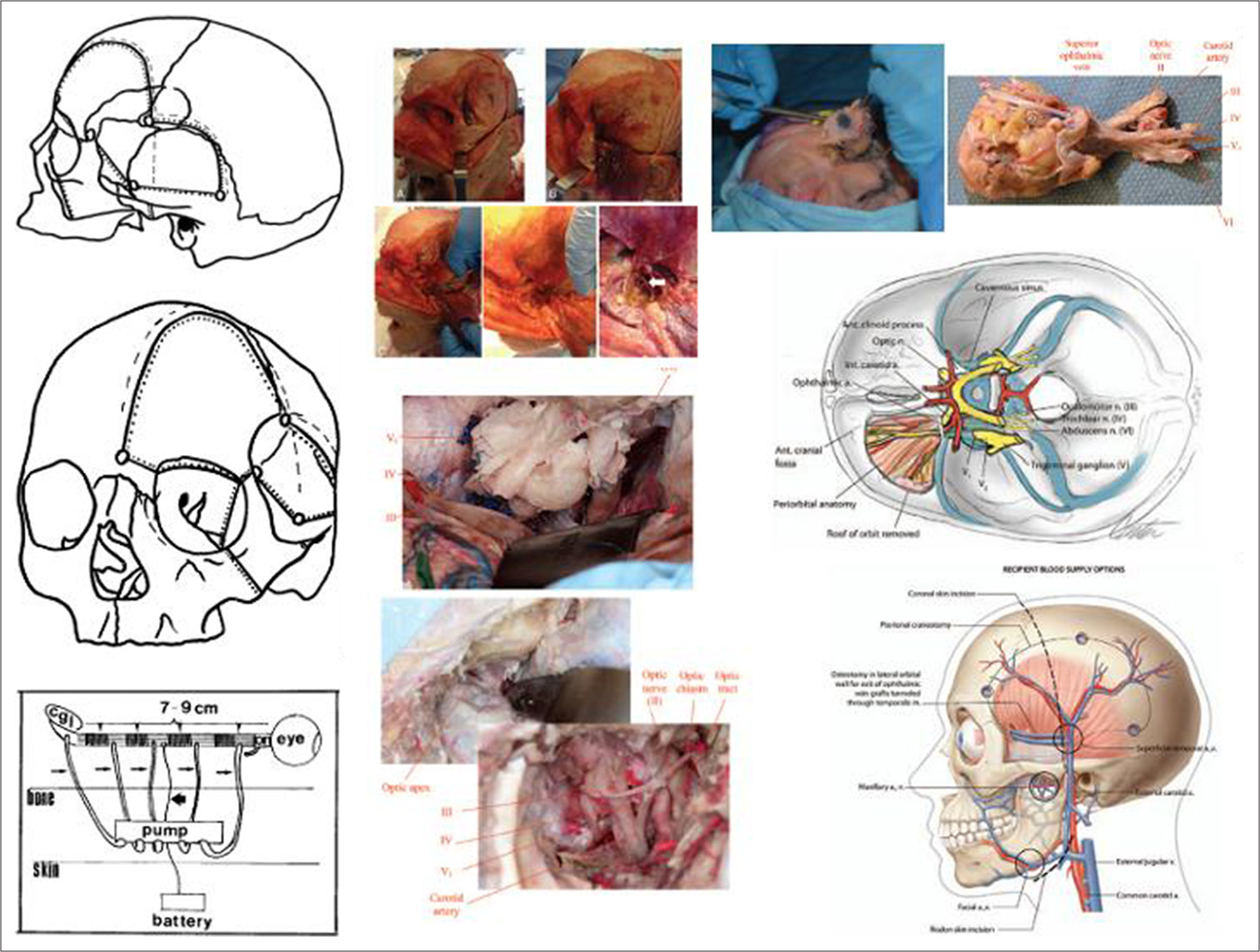
In 1992, one of us (SC) published a cadaveric-based protocol for whole eye transplantation that also included the tubulization of the ON stump with segments of the sural nerve to boost Schwann cell-enabled growth and avoid shrinkage, infusion of growth factors through a minipump directly into the tubular guide and ES through embedded wires attached to an external battery.[
That early work has been recently expanded with cadaveric rehearsals by another group[
In conclusion, eye transplantation is surgically feasible. Coaptation of the cranial nerves is carried out as discussed earlier in this article.
CONCLUSION
It is clear from the above discussion that both SC and eye transplantation represent the low hanging fruit of nerve fusion waiting for someone to start a clinical trial. The surgical approaches are clear. As regards cranial nerves and nerve roots, microsuturing remains burdensome and, as De Medinaceli so poignantly wrote, suboptimal. Instead, recent work shows that nerve fusion can be effected successfully by simple approximation with just two epineural sutures.[
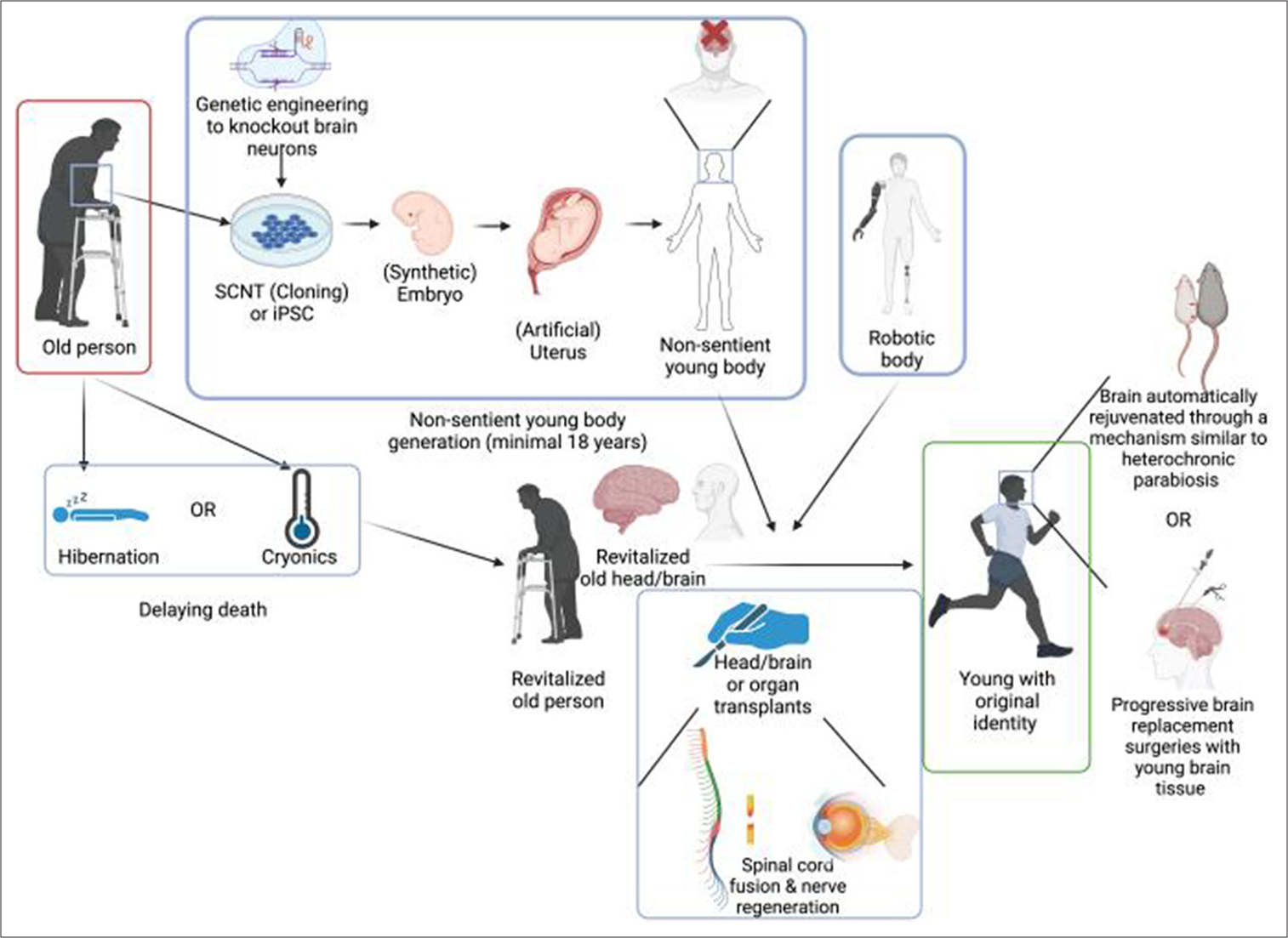
Brain transplantation[
As the father of astronautics, Konstantin Ėduardovič Tsiolkovsky (1857–1935), once said, “The impossible today will be the possible of tomorrow.” For transplantation neurosurgery, the future is now.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Bitar Alatorre WE, Garcia Martinez D, Rosales Corral SA, Flores Soto ME, Velarde Silva G, Portilla de Buen E. Critical ischemia time in a model of SC section. A study performed on dogs. Eur Spine J. 2006. 16: 563-72
2. Bittner GD, Tuffaha S, Shores JT. Polyethylene glycol-fusion repair of peripheral nerve injuries. Hand Clin. 2024. 40: 389-97
3. Canavero S. Heaven: The head anastomosis venture project outline for the first human head transplantation with spinal linkage (GEMINI). Surg Neurol Int. 2013. 4: S335-42
4. Canavero S, Ren X, Kim CY, Rosati E. Neurologic foundations of spinal cord fusion (GEMINI). Surgery. 2016. 160: 11-9
5. Canavero S, Ren XP, editors. The technology of head transplantation. Hauppage, NY: Nova Science Publishers; 2020. p.
6. Canavero S, editors. The technology of brain transplantation. Seattle, WA: Amazon Digital Services LLC; 2020. p.
7. Canavero S. Whole brain transplantation in man: Technically feasible. Surg Neurol Int. 2022. 13: 594
8. Canavero S, Ren XP. The spark of life: Engaging the corticotruncoreticulo-propriospinal pathway by electrical stimulation. CNS Neurosci Ther. 2016. 22: 260-1
9. Canavero S, Ren X, Kim C. Heterologous spinal cord transplantation in man. Surg Neurol Int. 2021. 12: 295
10. Canavero S, editors. The Frankenstein effect. Extreme brain reanimation. Seattle, WA: Amazon DS LLC; 2019. p.
11. Canavero S. Total eye transplantation for the blind: A challenge for the future. Med Hypotheses. 1992. 39: 201-11
12. Ceradini DJ, Tran DL, Dedania VS, Gelb B, Cohen OD, Flores RL. Combined whole eye and face transplant: Microsurgical strategy and 1-year clinical course. JAMA. 2024. 332: e2412601
13. Chibret PM. Transplantation of an eye from the rabbit to man. JAMA. 1885. 4: 713
14. Davidson EH, Wang EW, Yu JY, Fernandez-Miranda JC, Wang DJ, Li Y. Clinical considerations for vascularized composite allotransplantation of the eye. J Craniofac Surg. 2016. 27: 1622-8
15. Davidson EH, Wang EW, Yu JY, Fernandez-Miranda JC, Wang DJ, Richards N. Total human eye allotransplantation: Developing surgical protocols for donor and recipient procedures. Plast Reconstr Surg. 2016. 138: 1297-308
16. De Medinaceli L, editors. Cell surgery to repair divided nerves. France: C.A.S.I.S.-C.I.D; 1994. p.
17. Emborg ME, Gambardella JC, Zhang A, Federoff HJ. Autologous vs heterologous cell replacement strategies for Parkinson disease and other neurologic diseases. Handb Clin Neurol. 2024. 205: 41-56
18. Gupta A, el Masri WS. Multilevel spinal injuries. Incidence, distribution and neurological patterns. J Bone Joint Surg Br. 1989. 7: 692-5
19. Hakim N, Haberal M, Maluf D, editors. Transplantation surgery. Germany: Springer Nature; 2021. p.
20. He S, Xi C, Li X, Jia K, Xiao Z, Dai J. Transplantation of adult spinal cord grafts into spinal cord transected rats improves their locomotor function. Sci China Life Sci. 2019. 62: 725-33
21. Hebert JM. Could an old brain be made young again?. Surg Neurol Int. 2022. 13: 595
22. Kim CY, Baek J, Canavero S, Ren XP, editors. SC fusion in rodents and dogs. The Technology of head transplantation. Hauppage, NY: Nova Science Publishers; 2020. p. 83-92
23. Lain D, editors. Advancing conversations: Aubrey de grey-advocate for an indefinite human lifespan. England: Zero Books, John Hunt Publishing Ltd.; 2016. p.
24. Lebenstein-Gumovski M, Rasueva T, Zharchenko A, Bashahanov R, Kovalev DA, Zhirov A. Chitosan/PEG-mediated Spinal Cord fusion after complete dorsal transection in rabbits-functional results at 30 days. Surg Neurol Int. 2023. 14: 423
25. Lebenstein-Gumovski M, Zharchenko A, Rasueva T, Bashahanov R, Kovalev DA, Zhirov A. PEG-chitosan (Neuro-PEG) induced restoration of motor function after complete transection of the dorsal spinal cord in swine. A pilot study. Surg Neurol Int. 2023. 14: 424
26. Lebenstein-Gumovski MV, Zharchenko AV, Rasueva TS, Kovalev DA, Zhirov AM, Shatokhin AA. Comparison of clinical effectiveness of intraoperative and combined fusogen therapy for the treatment of spinal cord injury in experiment. Ross Neirokhirurgicheskii Zh Im. 2023. 15: 12
27. Lee M, Kiernan MC, Macefield VG, Lee BB, Lin CS. Short-term peripheral nerve stimulation ameliorates axonal dysfunction after spinal cord injury. J Neurophysiol. 2015. 113: 3209-18
28. Liao Z, Zhang J, Sun S, Li Y, Xu Y, Li C. Reprogramming mechanism dissection and trophoblast replacement application in monkey somatic cell nuclear transfer. Nat Commun. 2024. 15: 5
29. Liu Z, Cai Y, Wang Y, Nie Y, Zhang C, Xu Y. Cloning of macaque monkeys by somatic cell nuclear transfer. Cell. 2018. 172: P881-7
30. Newcombe R. Brain transplantation?. BMJ. 1968. 1: 178
31. Nourbakhsh A, Takawira C, Barras E, Hampton C, Carossino M, Nguyen K. A novel reconstruction model for thoracic spinal cord injury in swine. PLoS One. 2024. 19: e0308637
32. Pappolla Ma, Wu P, Fang X, Poeggeler B, Sambamurti K, Wisniewski T. Stem cell interventions in neurology: From bench to bedside. J Alzheimer’s Dis. 2024. 101: S395-416
33. Ren X, Li M, Zhao X, Liu Z, Ren S, Zhang X, Canavero S, Ren XP, editors. Spinal cord fusion in primates. The Technology of Head Transplantation. Hauppage, NY: Nova Science Publishers; 2020. p. 93-101
34. Ren X, Kim CY, Canavero S. Bridging the gap: Spinal cord fusion as a treatment of chronic spinal cord injury. Surg Neurol Int. 2019. 10: 51
35. Ren X, Zhang W, Mo J, Qin J, Chen Y, Han J. Partial restoration of spinal cord neural continuity via sural nerve transplantation using a technique of spinal cord Fusion. Front Neurosci. 2022. 16: 808983
36. Rueda-Lopes F. The cranial nerves: Extensions of the central nervous system or components of the peripheral nervous system-how should we evaluate them?. Radiol Bras. 2021. 54: 5-6
37. Ryan I, Henderson PW, Canavero S, Ren XP, editors. GEMINI: Overview of fusogens. The technology of head transplantation. Hauppage, NY: Nova Science Publishers; 2020. p. 51-68
38. Scarabosio A, Surico PL, Tereshenko V, Singh RB, Salati C, Spadea L. Whole-eye transplantation: Current challenges and future perspectives. World J Transplant. 2024. 14: 95009
39. Shkarubo AN, Ogurtsova AA, Yakupova ZF, Revishchin AV, Shishkina LV, Pronin IN. Experimental reconstruction of the optic nerve with a sural nerve graft: An in vivo experimental study. World Neurosurg. 2024. 188: e631-41
40. Shirres DA. Regeneration of the axones of spinal neurones in man. Montreal Med J. 1905. p. 1-11
41. Simon A, Gilbert GV, Fisher AH, Johnsen PH, Herb B, Vega SL. A comparison of two versus five epineural sutures to achieve successful polyethylene glycol (PEG) nerve fusion in a rat sciatic nerve repair model. Surg Neurol Int. 2024. 15: 152
42. Tomsia M, Ciesla J, Smieszek J, Florek S, Macionga A, Michalczyk K. Long-term space missions’ effects on the human organism: What we do know and what requires further research. Front Physiol. 2024. 13:15: 1284644
43. Williams PT, Schelbaum E, Ahmanna C, Alexander H, Kanté K, Soares S. Combined biomaterial scaffold and neuromodulation strategy to promote tissue repair and corticospinal connectivity after spinal cord injury in a rodent model. Exp Neurol. 2024. 382: 114965
44. Woolsey D, Minckler J, Rezende N, Klemme R. Human spinal cord transplantation. Exp Med Surg. 1944. 2: 93-102
45. Zhang W, Lan R, Shen T, Qin J, Wang Z, Chen J. A novel strategy for spinal cord reconstruction via vascularized allogeneic spinal cord transplantation combine spinal cord fusion. CNS Neurosci Ther. 2024. 30: e70020
46. Zipser CM, Curt A. Disease-specific interventions using cell therapies for spinal cord disease/injury. Handb Clin Neurol. 2024. 205: 263-82
47. Zor F, Karagoz H, Kapucu H, Kulahci Y, Janjic JM, Gorantla VS. Immunological considerations and concerns as pertinent to whole eye transplantation. Curr Opin Organ Transplant. 2019. 24: 726-32