- Department of Neurosurgery, University of Kentucky,
- Department of Neurosurgery, Lexington Veterans Affairs Medical Center, Lexington, Kentucky, United States.
Correspondence Address:
Tripp Hines, Department of Neurosurgery, University of Kentucky, Lexington, Kentucky, United States.
DOI:10.25259/SNI_339_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Tripp Hines1, Catherine Wang1, Christine Duttlinger2, Jay Thompson2, Kevin Watford2, Benjamin Motley1, Greg Wheeler1,2. Thoracic dorsal arachnoid web with rapid onset of symptoms: A report of two cases and brief review of the literature. 06-Jul-2021;12:323
How to cite this URL: Tripp Hines1, Catherine Wang1, Christine Duttlinger2, Jay Thompson2, Kevin Watford2, Benjamin Motley1, Greg Wheeler1,2. Thoracic dorsal arachnoid web with rapid onset of symptoms: A report of two cases and brief review of the literature. 06-Jul-2021;12:323. Available from: https://surgicalneurologyint.com/surgicalint-articles/10955/
Abstract
Background: Thoracic arachnoid webs are a rare entity and can be challenging to diagnose with sometimes subtle radiographic findings. Arachnoid webs can cause severe cord compression with associated syrinx and resulting myelopathy, weakness, sensory loss, and bowel/bladder dysfunction. There have been a little over 60 cases total reported in the literature with only one systematic review. The cases presented here have unique features including rapid onset of symptoms, symptomatic syrinx extending into the cervical spine, and intraoperative syrinx drainage, all of which are quite rare in the current published literature for arachnoid webs.
Case Description: Here, we present two patients, a 73-year-old man and 58-year-old man presenting with different symptoms and timing of symptom progression but both with “scalpel sign” and associated syrinx present on their MRIs. Each patient underwent a laminectomy with resection of arachnoid web with complete resolution of symptoms in the first case and significant improvement in the second case. Postoperative imaging in both cases showed almost complete resolution of the syrinx.
Conclusion: Early clinical evaluation and workup followed by early surgical treatment can lead to dramatic improvement in outcomes after surgery. For patients that are symptomatic from an associated syrinx, a midline myelotomy to facilitate drainage can be considered to be done concomitantly with the arachnoid web resection.
Keywords: Arachnoid web, Dorsal, Review, Spine, Surgery, Thoracic
INTRODUCTION
Thoracic dorsal arachnoid webs of the spine are rare and often challenging to diagnose, with subtle radiographic findings. When left untreated, it can have devastating effects on a patient’s neurological function, causing insidious progression of weakness and myelopathy in otherwise healthy individuals. Here, we present two case reports, with descriptions of each patient’s presentation with comparisons to the published literature, to better understand this lesion. These cases have unique features including rapid symptom onset and symptomatic syrinx into the cervical spine, which are quite extraordinary.
ILLUSTRATIVE CASES
Case 1
History and examination
Patient is a 73-year-old gentleman who presented to the VA (Veterans Affairs) neurosurgery clinic with complaints of neck pain and bilateral leg weakness that started 10 days before. He had pain that radiated into both shoulders and generalized weakness and pain in both legs. He reported trouble walking, complaining “he walked like a 95-year-old.” He denied any trauma, falls, changes in balance, problems with fine motor skills, or any bowel or bladder incontinence. Before symptom onset, he was walking 3 miles a day and was regularly active.
Prior medical history includes hypertension, Stage III chronic kidney disease, esophageal invasive adenocarcinoma status postgastrectomy and resection 1 year prior requiring no adjuvant treatment, and diabetes mellitus type 2. He had no prior spine surgeries. Laboratories were unremarkable except for elevated glucose and serum creatinine of 1.99 mg/ dL. Hemoglobin A1c was 6.4%.
On examination, he was full strength in both arms and was four out of five strength in both legs. Sensation was intact to light touch throughout. He had 3+ DTRs (deep tendon reflexes) in his left arm, 2+ DTRs in the right arm, and 4+ DTRs in both legs. He had a negative Hoffman’s sign and 1–2 beats of clonus in both legs. He had a positive Romberg’s sign and broad-based unsteady gait.
Imaging
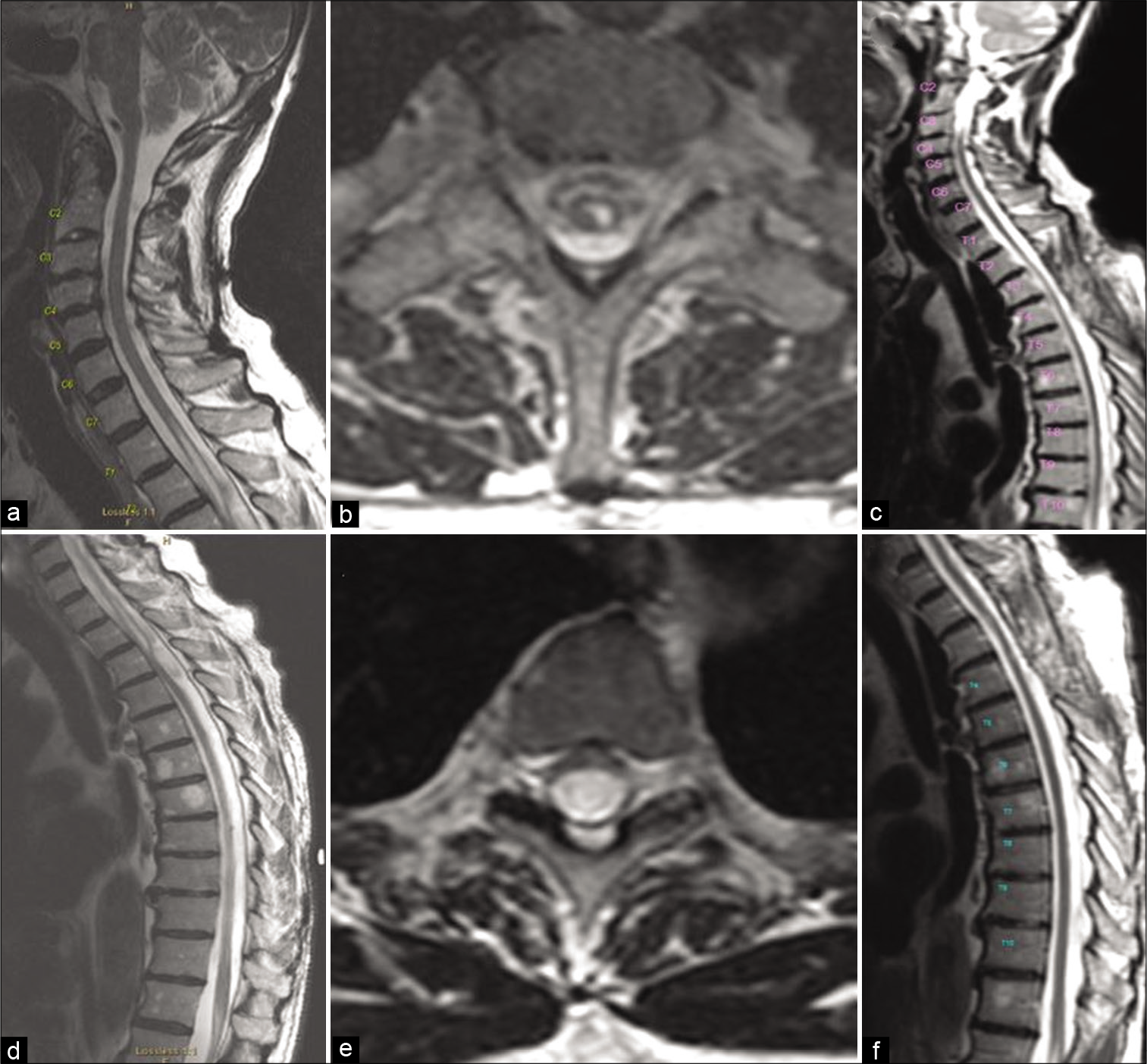
Initially, he had a MRI of the cervical spine without contrast [
Figure 1:
Preoperative (a, b, d, e) and postoperative (c, f) MR images obtained in case 1. Sagittal images (a, d) show syrinx extending up to C7-T1 with “scalpel” configuration at T3. Axial images at the level of C7-T1 (b) show syrinx and at the level of T3 (e) show severe spinal cord compression. Postoperative sagittal images (c and f) show complete resolution of syrinx and spinal cord compression.
Surgery
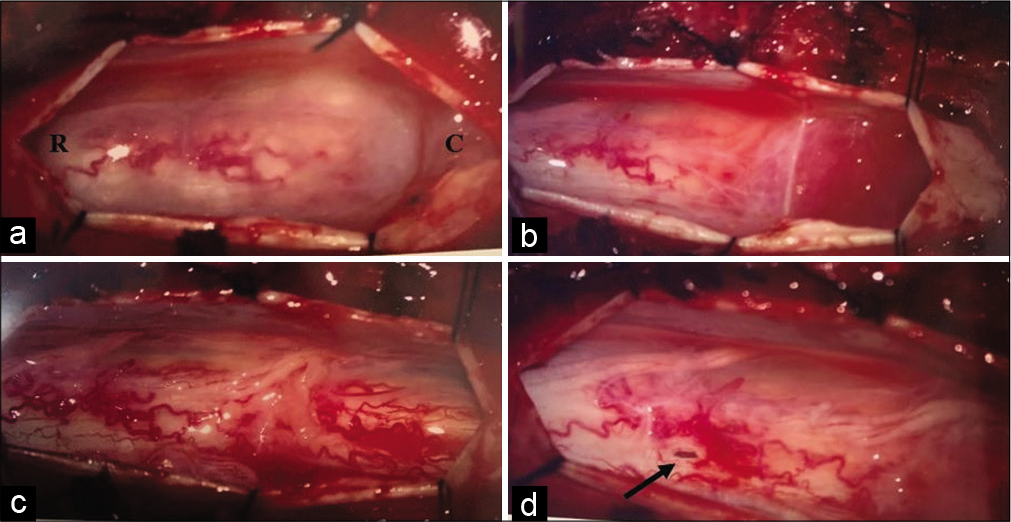
The patient underwent T2-T4 laminectomies with resection of arachnoid web and use of intraoperative neuromonitoring [
Figure 2:
Intraoperative photographs obtained in case 1. (a) The thickened white arachnoid web is apparent at approximately T3 with venous congestion in the spinal cord noted rostrally. (b) Microdissection of the band from the caudal side. (c) Partial resection of thickened arachnoid web with remaining attachment on the right side (top). (d) Complete resection of arachnoid web with resolution of spinal cord venous congestion. C: Caudal, R: Rostral.
Postoperative course
The patient was seen in clinic 2 weeks after surgery with complete resolution of his symptoms. He had returned to walking 3 miles daily by postoperative day 2. His incision was well healed; staples were removed and he was full strength on examination. He was cleared to return to work 2 weeks after that. He had a new MRI thoracic spine with and without contrast 1 month postoperative that showed complete resolution of syrinx and no further spinal cord compression [
Case 2
History and examination
Patient is a 58-year-old gentleman who presented to the VA neurosurgery clinic with complaints of neck pain and left arm pain. His symptoms started 4 months before his clinic visit. He had left-sided neck pain and severe pain down his entire left arm into all of his fingers. He described this pain as constant with slight improvement with hot showers and taking gabapentin 1200 mg 3 times daily. He also had pain and numbness along his left thorax and left ear and face numbness. He had noted some left arm weakness. He denied any recent trauma (prior MVC 15 years ago), falls, changes in balance, problems with fine motor skills, or any bowel or bladder incontinence.
Prior medical history includes gastroesophageal reflux disease with Barrett’s esophagus, generalized anxiety disorder, recurrent major depressive episodes, hypertension, restless legs syndrome, cocaine abuse, hepatitis C, diabetes mellitus type 2, and diabetic peripheral neuropathy. He had no prior spine surgeries.
Laboratories were unremarkable. On examination, he was full strength in his right arm and both legs and was three out of five strength in his left deltoid and four out of five strength in the rest of his left arm. Sensation was intact to light touch throughout, except decreased in the left arm, left hemithorax, and left jaw. He had diminished DTRs in his left arm. He had a negative Hoffman’s sign, no clonus and a negative Romberg’s sign. He had significant left arm muscle atrophy.
Imaging
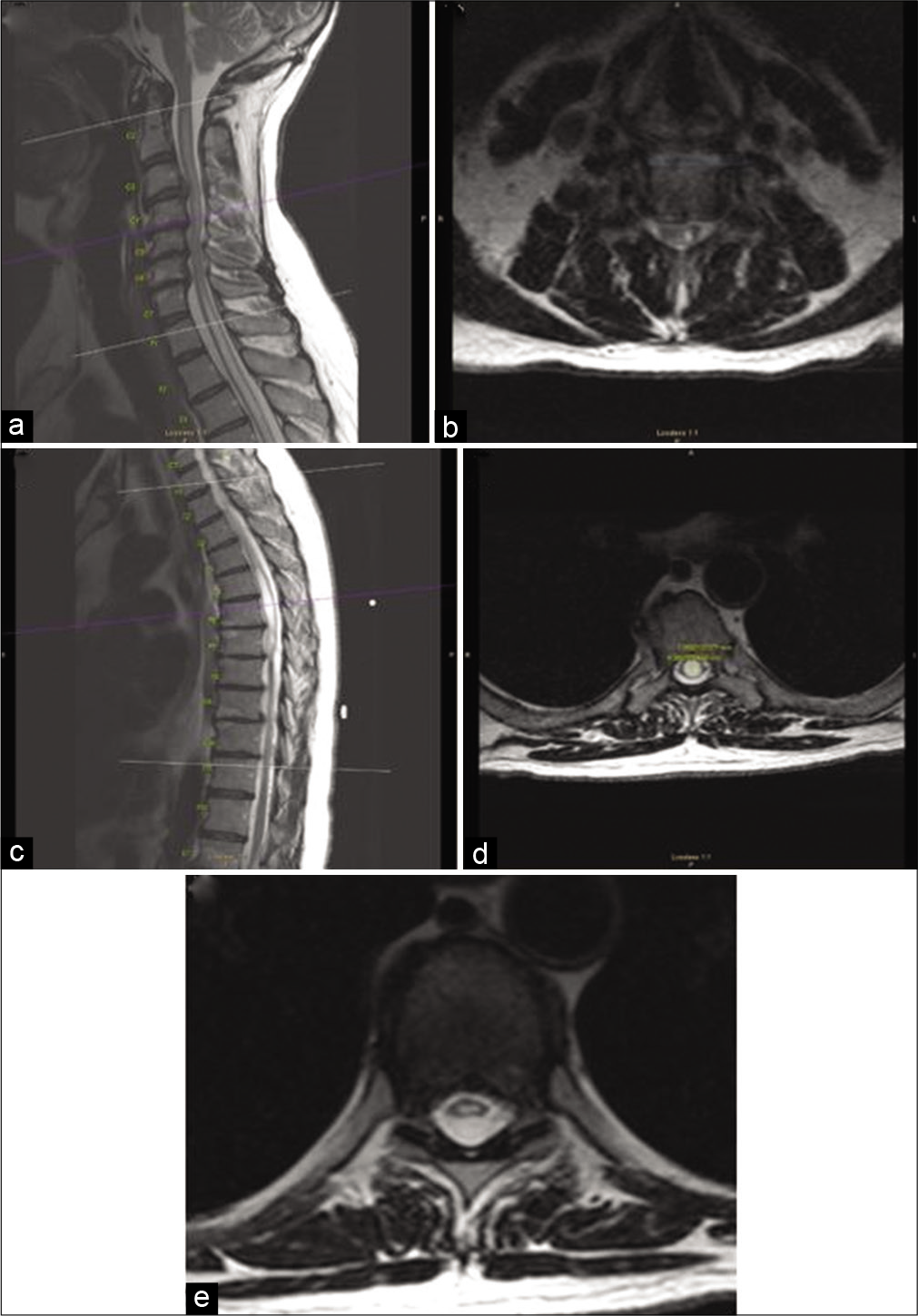
He underwent a MRI of his neuroaxis including MRI head without contrast that showed no acute pathology, incidental pineal gland cyst, and mild inflammatory changes along left mastoid. His MRI of the cervical spine with and without contrast [
Figure 3:
Preoperative MR images obtained in case 2. Sagittal and axial images (a and b) show large syrinx extending up through the cervical cord and primarily on the left side above C7. Thoracic sagittal (c) and axial images at the level of T6 (d) show large 9.4 × 7.1 mm syrinx at its maximum diameter and at the level of T7-T8 (e) show spinal cord compression due to the arachnoid web.
Surgery
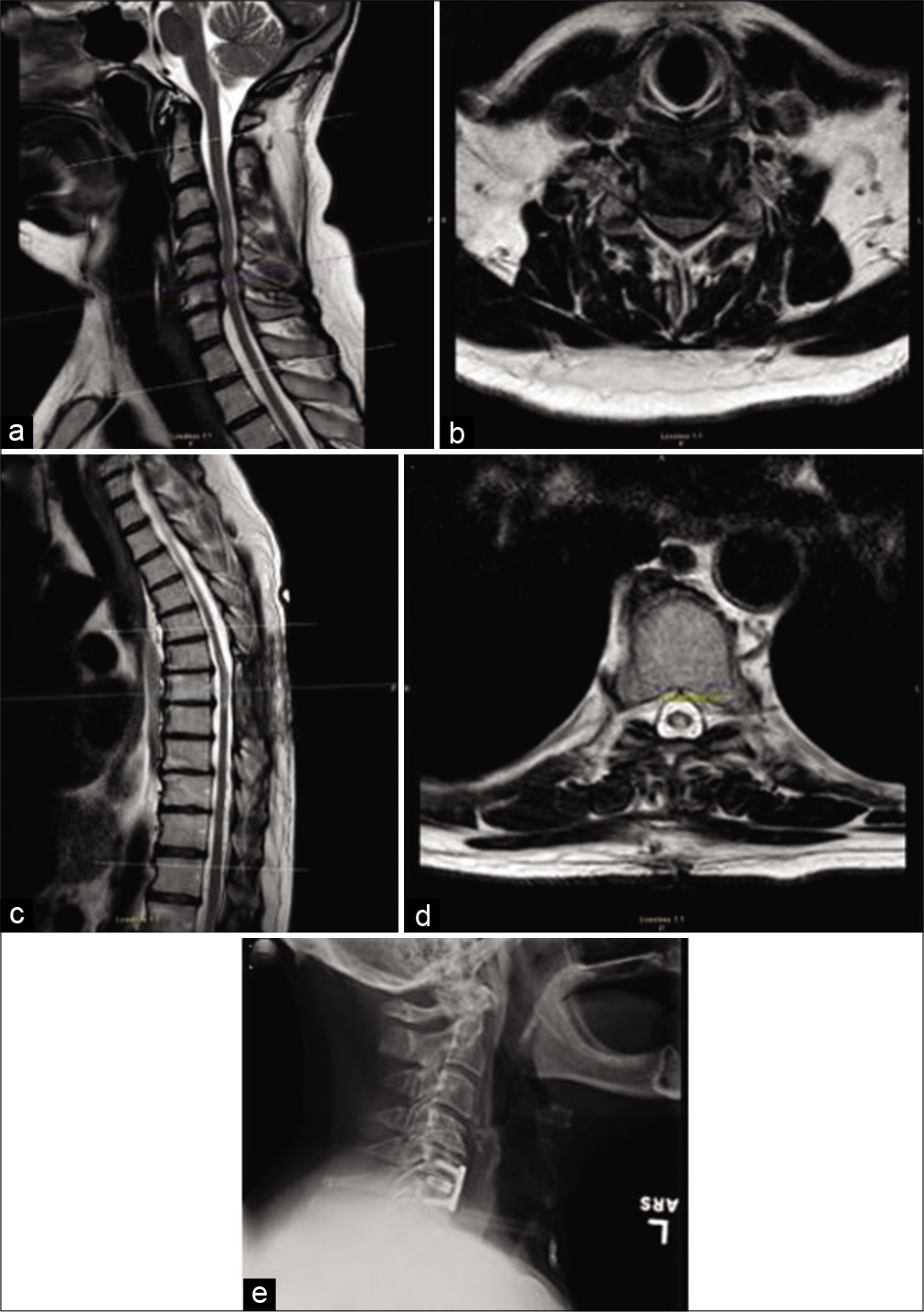
The patient underwent T7-T9 laminectomies with resection of arachnoid web, midline myelotomy with drainage of intramedullary syrinx, and use of intraoperative neuromonitoring [
Figure 4:
Intraoperative photographs obtained in case 2. (a) The cloudy thickened arachnoid web is seen caudally. (b) After slightly extending durotomy caudally, the full extent of arachnoid web is appreciated with spinal cord venous congestion inferiorly. (c) Complete resection of arachnoid bed with improvement of venous congestion. (d) Small midline myelotomy (arrow) to allow for drainage of large syrinx. C: Caudal, R: Rostral.
Postoperative course
The patient was seen in clinic 2 weeks after surgery with significant improvement of his symptoms, especially his numbness and tingling. He continued to have persistent left arm pain, but only in a C6 distribution after surgery. His incision was well healed, staples were removed and the patient was full strength on examination. He had a new MRI of the cervical and thoracic spine with and without contrast 1 month postoperative that showed near-complete resolution of syrinx and no further spinal cord compression at the level of the arachnoid web, but remaining severe stenosis at C5-C6 [
Figure 5:
Postoperative MR images (a-d) and X-rays (e) obtained in case 2. Cervical sagittal (a) and axial images (b) show complete resolution of cervical syrinx with residual severe C5-C6 stenosis. Thoracic images (c and d) show near-complete resolution of syrinx and resolution of spinal cord compression. (e) Interval anterior cervical discectomy and fusion at C5-C6.
DISCUSSION
Thoracic arachnoid webs are a rare entity with only 63 reports documented in the literature.[
Another unique aspect of our second case was that the patient was more symptomatic from the syrinx caused by the thoracic web rather than the compression from the web. He had significant left arm atrophy and pain due to the syrinx extending into his cervical spine up to C2, which is quite a rare finding. Only three cases documenting an associated syrinx extending into the cervical spine have been reported in literature.[
In reviewing the literature, all arachnoid webs were found exclusively in the thoracic spine with a syrinx associated with over two-thirds of cases.[
Imaging diagnosis
Imaging is extremely important in diagnosing arachnoid webs, especially when differentiating arachnoid cysts and spinal cord herniation. The “scalpel sign” is a pathognomonic radiologic finding describing the CSF space outline and spinal cord indentation on sagittal imaging that is seen with arachnoid webs.[
Pathophysiology
Arachnoid web is an extramedullary transverse band of arachnoid tissue that extends to the dorsal surface of the spinal cord resulting in mass effect and dorsal indentation of the spinal cord.[
Treatment and outcomes
The most common surgical treatment is with laminectomy with intradural excision of the arachnoid web including variations of this with hemilaminectomy and minimally invasive techniques.[
CONCLUSION
Thoracic arachnoid webs remain a rare entity that can have severe neurological impairments with rapid improvement of symptoms postoperatively. For patients that are symptomatic from an associated syrinx, a midline myelotomy to facilitate drainage can be considered to be done concomitantly with the arachnoid web resection.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Ali H, Hamilton P, Zygmunt S, Yakoub K. Spinal arachnoid web-a review article. J Spine Surg. 2018. 4: 446-50
2. Aljuboori Z, Boakye M. Rare dorsal thoracic arachnoid web mimics spinal cord herniation on imaging. Surg Neurol Int. 2020. 11: 66
3. Aljuboori Z, Boakye M. Surgical release of a dorsal thoracic arachnoid web. World Neurosurg. 2020. 143: 289
4. Brasil P, Pereira L, Távora D, Camara A, Filho CM, Coimbra P. Imaging findings in dorsal thoracic arachnoid web and the differential diagnosis of “scalpel sign”. Neurographics. 2020. 10: 96-102
5. Chang H, Nagai A, Oya S, Matsui T. Dorsal spinal arachnoid web diagnosed with the quantitative measurement of cerebrospinal fluid flow on magnetic resonance imaging. J Neurosurg Spine. 2014. 20: 227-33
6. Heiss J, Snyder K, Peterson M, Patronas NJ, Butman JA, Smith RK. Pathophysiology of primary spinal syringomyelia. J Neurosurg Spine. 2012. 17: 367-80
7. Hirai T, Taniyama T, Yoshii T, Mizuno K, Okamoto M, Inose H. Clinical outcomes of surgical treatment for arachnoid web: A case series. Spine Surg Relat Res. 2019. 3: 43-8
8. Hubbard M, Hunt M, Jones K, Polly D. Thoracic spinal cord impingement by an arachnoid web at the level of a hemivertebra: Case report. J Neurosurg Spine. 2017. 27: 638-42
9. Inoue J, Miyakoshi N, Hongo M, Kobayashi T, Abe T, Kikuchi K. Diagnosis and surgical treatment of thoracic dorsal arachnoid web: A report of two cases. Case Rep Orthop. 2020. 2020: 8816598
10. Nisson P, Hussain I, Härtl R, Kim S, Baaj A. Arachnoid web of the spine: A systematic literature review. J Neurosurg Spine. 2019. 31: 175-84
11. Paramore C. Dorsal arachnoid web with spinal cord compression: Variant of an arachnoid cyst?. J Neurosurg. 2000. 93: 287-90
12. Qureshi A, Bains N, Balasetti V, Salame K, Gomez CR, Siddiq F. Percutaneous fenestration of a spinal arachnoid web using an intrathecal catheter: Effect on cerebrospinal fluid flow and clinical status. World Neurosurg. 2020. 142: 17-23
13. Reardon M, Raghavan P, Carpenter-Bailey K, Mukherjee S, Smith JS, Matsumoto JA. Dorsal thoracic arachnoid web and the “Scalpel Sign”: A distinct clinical-radiologic entity. Am J Neuroradiol. 2013. 34: 1104-10
14. Vergara P, Barone D. Minimally invasive excision of thoracic arachnoid web. World Neurosurg. 2018. 109: e81-7
15. Zhang D, Papavassiliou E. Spinal intradural arachnoid webs causing spinal cord compression with inconclusive preoperative imaging: A report of 3 cases and a review of the literature. World Neurosurg. 2017. 99: 251-8