- Department of Neurosurgery, Hospital Universitario Fundacion Favaloro, Buenos Aires, Argentina.
- Department of Hand Surgery, Hospital Universitario Fundacion Favaloro, Buenos Aires, Argentina.
- Department of Neurosurgery, Hospital de Clínicas José de San Martín (UBA), Buenos Aires, Argentina.
Correspondence Address:
Juan Pablo Martinez, Department of Neurosurgery, Hospital Universitario Fundacion Favaloro, Buenos Aires, Argentina.
DOI:10.25259/SNI_91_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Juan Pablo Martinez1, Ana Lovaglio1, Gilda Di Masi1, Jorge Mandolesi1, Pablo Zancolli2, Mariano Socolovsky3. Thoracodorsal to long thoracic nerve transfer in a patient with traumatic injury: A case report. 17-May-2024;15:163
How to cite this URL: Juan Pablo Martinez1, Ana Lovaglio1, Gilda Di Masi1, Jorge Mandolesi1, Pablo Zancolli2, Mariano Socolovsky3. Thoracodorsal to long thoracic nerve transfer in a patient with traumatic injury: A case report. 17-May-2024;15:163. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=12899
Abstract
Background: Traumatic injury to the long thoracic nerve causes paralysis of the serratus muscle, clinically expressed as winged scapula and functional impairment of the shoulder girdle. Treatment varies according to the severity of the injury, with a focus on early intervention for best results; however, the therapeutic approach remains a challenge at present.
Case Description: We present the case of a 32-year-old male patient, athlete, right-handed, presented with bilateral paresis predominantly in the right arm, associated with paresthesia and changes in the coloring of the upper limbs. After being diagnosed with Thoracic Outlet Syndrome and undergoing surgery, vascular symptoms persisted with a significant loss of strength in the right shoulder. Winged scapula was observed and structural lesions were excluded on magnetic resonance imaging. Electromyographic studies confirmed the presumption of traumatic nerve involvement of the long thoracic nerve. Notwithstanding 6 months of physical therapy, there was no improvement, so a nerve transfer from the thoracodorsal nerve to the right long thoracic nerve was chosen. At 12 months, complete resolution of the winged scapula and functional recovery were observed. The patient also experienced a decrease in preoperative pain from 5/10 to 2/10 on the visual analog scale.
Conclusion: Nerve transfer from the thoracodorsal nerve to the long thoracic nerve is a safe and effective technique to treat winged scapula due to long thoracic nerve injury.
Keywords: Injury, Long thoracic, Nerve transfer, Peripheral nerve, Thoracodorsal, Injury
INTRODUCTION
The long thoracic nerve – also known as the serratus major nerve or Charles Bell’s nerve[
CASE REPORT
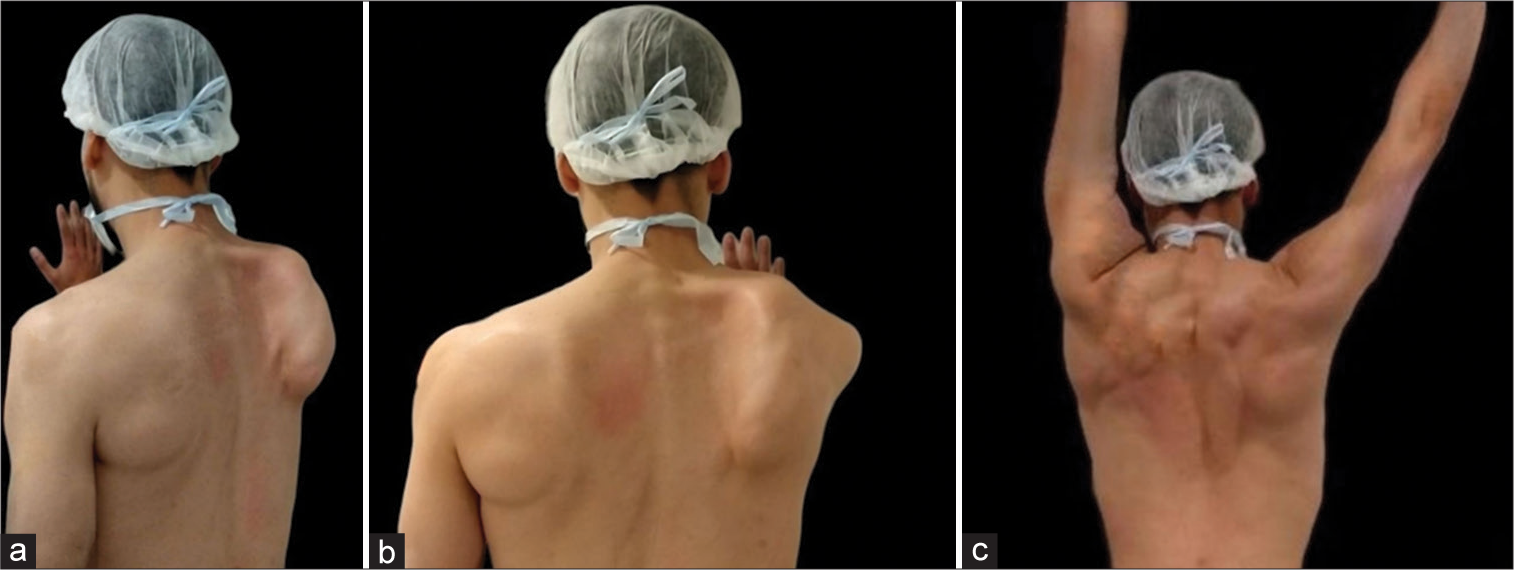
We present a 32-year-old male patient, a right-handed athlete, who presented with a bilateral (predominantly right upper limb) abduction paresis of 12 months duration, associated with progressive paresthesias and changes in the coloring of the upper limbs. As an important history before the consultation, he had been diagnosed with vascular Thoracic Outlet Syndrome in another institution for which he had undergone surgery. The right first rib had been resected in that procedure with an axillary approach on that side. After surgery, the patient developed persistence of previous vascular symptoms and loss of flexion strength in the right shoulder. On physical examination at our clinic, we observed a right-winged scapula together with an absence of commitment of the deltoid, triceps, supraspinatus, and infraspinatus muscles [
Video 1
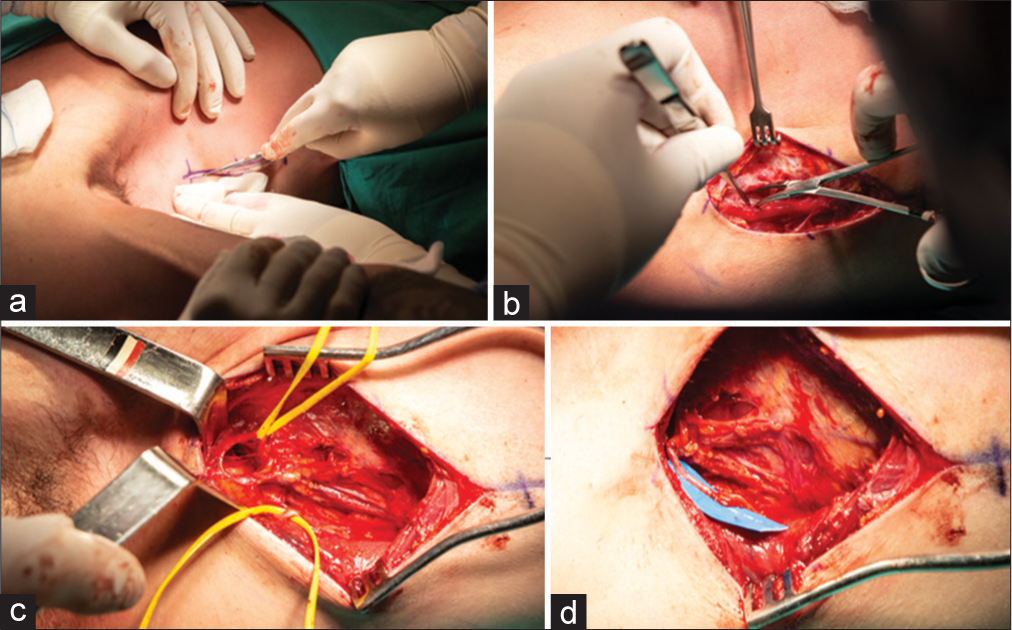
Figure 2:
(a) Intraoperative picture showing a skin incisión; (b) intraoperative picture showing a dissection of the latissimus dorsi; (c) intraoperative picture showing a separate thoracodorsal nerve in the inferior side and long thoracic nerve in the superior side; and (d) intraoperative picture showing the preparation of donor branches for neurorrhaphy.
A bandage was applied to immobilize the patient’s shoulder in adduction and internal rotation for 2 weeks, after which physical therapy sessions were started with activation movements for the latissimus dorsi and pectoralis major muscles, 5 times a week for 90 min during the first 3 months, and then continued for the same duration, 3 times a week. During the sessions, the exercises described by Ray et al. were carried out, with evident and progressive results from the 4th month of physiotherapy.[
The patient was monitored 6 months after surgery, with partial improvement of the winged scapula and good recovery of flexion and function of the right shoulder. At 12 months, there was complete resolution of the winged scapula, with full functional recovery and muscle strength of both the latissimus dorsi and pectoralis muscles. The patient reported that he was able to complete all his routine activities normally and also showed a decrease in preoperative pain with Visual Analog Scale, 5/10–2/10 [
Figure 3:
(a) Postoperative examination at 12 months showing total resolution of the winged scapula, functional recovery, and muscle strength; (b) Postoperative examination at 12 months showing total resolution of the winged scapula, functional recovery, and muscle strength; and (c) postoperative examination at 12 months showing total resolution of the winged scapula, functional recovery, and muscle strength.
DISCUSSION
Injury to the long thoracic nerve results in severe loss of shoulder function, particularly flexion, due to loss of scapular stabilization and rotation.[
It remains difficult to determine a definitive therapeutic option in this pathology, especially due to its varied presentations. Physiotherapy and clinical observation are the recommended initial treatment, with many documented cases describing favorable results with this conservative strategy.[
Surgical options are extensive, although recently, according to literature reports, both nerve transfer and modified pectoralis major muscle-tendon transfer have gained prominence.[
CONCLUSION
Nerve transfer from the thoracodorsal nerve to the long thoracic nerve is very useful, proving to be a safe and successful technique for the treatment of winged scapula due to long thoracic nerve injury. We recommend this procedure for patients with <1 year of postinjury evolution. It is important to implement a good physical therapy program before and after surgery to optimize the functional results of the shoulder.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Video link:
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Atasoy E, Majd M. Scapulothoracic stabilisation for winging of the scapula using strips of autogenous fascia lata. J Bone Joint Surg Br. 2000. 82: 813-7
2. Berry H, MacDonald EA, Mrazek AC. Accessory nerve palsy: A review of 23 cases. Can J Neurol Sci. 1991. 18: 337-41
3. Connor PM, Yamaguchi K, Manifold SG, Pollock RG, Flatow EL, Bigliani LU. Split pectoralis major transfer for serratus anterior palsy. Clin Orthop Relat Res. 1997. 341: 134-42
4. Del Sasso L, Mondini A, Brambilla S. A case of isolated paralysis of serratus anterior. Ital J Orthop Traumatol. 1988. 14: 533-7
5. Elhassan BT, Wagner ER. Outcome of transfer of the sternal head of the pectoralis major with its bone insertion to the scapula to manage scapular winging. J Shoulder Elbow Surg. 2015. 24: 733-40
6. Friedenberg SM, Zimprich T, Harper CM. The natural history of long thoracic and spinal accessory neuropathies. Muscle Nerve. 2002. 25: 535-9
7. Fu SY, Gordon T. Contributing factors to poor functional recovery after delayed nerve repair: Prolonged denervation. J Neurosci. 1995. 15: 3886-95
8. Gordon SL, Graham WP, Black JT, Miller SH. Acessory nerve function after surgical procedures in the posterior triangle. Arch Surg. 1977. 112: 264-8
9. Gregg JR, Labosky D, Harty M, Lotke P, Ecker M, DiStefano V. Serratus anterior paralysis in the young athlete. J Bone Joint Surg Am. 1979. 61: 825-32
10. Grzybowski A, Kaufman MH. Sir Charles Bell (1774-1842): Contributions to neuro-ophthalmology. Acta Ophthalmol Scand. 2007. 85: 897-901
11. Kauppila LI, Vastamäki M. Iatrogenic serratus anterior paralysis. Long-term outcome in 26 patients. Chest. 1996. 109: 31-4
12. Klebe TM, Døssing KV, Blenstrup T, Nielsen-Ferreira J, Rejsenhus L, Aalkjaer G. Scapulae alatae--englevinger. En opgørelse of 64 patienter behandlet med brace-bandage og fysioterapi på Viborg Sygehus [Scapulae alatae-angels’ wings. A study of 64 patients treated with braces and physical therapy at the Viberg’s hospital]. Ugeskr Laeger. 2003. 165: 1779-82
13. Mackinnon SE, Novak CB. Nerve transfers. New options for reconstruction following nerve injury. Hand Clin. 1999. 15: 643-66
14. Mah JY, Otsuka NY. Scapular winging in young athletes. J Pediatr Orthop. 1992. 12: 245-7
15. Makin GJ, Brown WF, Ebers GC. C7 radiculopathy: Importance of scapular winging in clinical diagnosis. J Neurol Neurosurg Psychiatry. 1986. 49: 640-4
16. Marin R. Scapula winger’s brace: A case series on the management of long thoracic nerve palsy. Arch Phys Med Rehabil. 1998. 79: 1226-30
17. Martin RM, Fish DE. Scapular winging: Anatomical review, diagnosis, and treatments. Curr Rev Musculoskelet Med. 2008. 1: 1-11
18. Noland SS, Krauss EM, Felder JM, Mackinnon SE. Surgical and clinical decision making in isolated long thoracic nerve palsy. Hand (N Y). 2018. 13: 689-94
19. Novak CB, Mackinnon SE. Surgical treatment of a long thoracic nerve palsy. Ann Thorac Surg. 2002. 73: 1643-5
20. Ogino T, Sugawara M, Minami A, Kato H, Ohnishi N. Accessory nerve injury: Conservative or surgical treatment?. J Hand Surg Br. 1991. 16: 531-6
21. Parsonage MJ, Turner JW. Neuralgic amyotrophy; the shoulder-girdle syndrome. Lancet. 1948. 1: 973-8
22. Perlmutter GS, Leffert RD. Results of transfer of the pectoralis major tendon to treat paralysis of the serratus anterior muscle. J Bone Joint Surg Am. 1999. 81: 377-84
23. Phillips LH. Familial long thoracic nerve palsy: A manifestation of brachial plexus neuropathy. Neurology. 1986. 36: 1251-3
24. Pugliese GN, Green RF, Antonacci A. Radiation-induced long thoracic nerve palsy. Cancer. 1987. 60: 1247-8
25. Ray WZ, Pet MA, Nicoson MC, Yee A, Kahn LC, Mackinnon SE. Two-level motor nerve transfer for the treatment of long thoracic nerve palsy. J Neurosurg. 2011. 115: 858-64
26. Saunders JR, Hirata RM, Jaques DA. Considering the spinal accessory nerve in head and neck surgery. Am J Surg. 1985. 150: 491-4
27. Seckel BR. Enhancement of peripheral nerve regeneration. Muscle Nerve. 1990. 13: 785-800
28. Segonds JM, Alnot JY, Asfazadourian H. Paralysie isolée du muscle serratus antérieur d’origine traumatique [Isolated traumatic serratus anterior muscle palsy]. Rev Chir Orthop Reparatrice Appar Mot. 2002. 88: 751-9
29. Sharp WJ, Nowak LR, Zamani T, Kresowik TF, Hoballah JJ, Ballinger BA. Long-term follow-up and patient satisfaction after surgery for thoracic outlet syndrome. Ann Vasc Surg. 2001. 15: 32-6
30. Sunderland S. The anatomy and physiology of nerve injury. Muscle Nerve. 1990. 13: 771-84
31. Vastamäki M, Kauppila LI. Etiologic factors in isolated paralysis of the serratus anterior muscle: A report of 197 cases. J Shoulder Elbow Surg. 1993. 2: 240-3
32. Warner JJ, Navarro RA. Serratus anterior dysfunction. Recognition and treatment. Clin Orthop Relat Res. 1998. 349: 139-48
33. Watson CJ, Schenkman M. Physical therapy management of isolated serratus anterior muscle paralysis. Phys Ther. 1995. 75: 194-202
34. Weisberger EC, Kincaid J, Riteris J. Cable grafting of the spinal accessory nerve after radical neck dissection. Arch Otolaryngol Head Neck Surg. 1998. 124: 377-80
35. Wiater JM, Flatow EL. Long thoracic nerve injury. Clin Orthop Relat Res. 1999. 368: 17-27