- Neurosurgery Unit, Department of Surgery, Modibbo Adama University Teaching Hospital, Yola, Nigeria
- Department of Ophthalmology, Modibbo Adama University Teaching Hospital, Yola, Nigeria
- Department of Surgery, Modibbo Adama University Teaching Hospital, Yola, Nigeria
Correspondence Address:
Emmanuel Garba Sunday, Neurosurgery Unit, Department of Surgery, Modibbo Adama University Teaching Hospital, Yola, Nigeria.
DOI:10.25259/SNI_618_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Emmanuel Garba Sunday1, Temitope Mariam Gbadegesin2, Daniel Wycliffe3, Bala Nasir Muhammad3. Transorbital subfrontal arrowhead injury: Experience in a low-resource setting. 25-Oct-2024;15:379
How to cite this URL: Emmanuel Garba Sunday1, Temitope Mariam Gbadegesin2, Daniel Wycliffe3, Bala Nasir Muhammad3. Transorbital subfrontal arrowhead injury: Experience in a low-resource setting. 25-Oct-2024;15:379. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13167
Abstract
Background:With the insurgency and farmer-herder crisis in northeast Nigeria, arrow injuries with various fatalities have been on the increase. Practicing in a low-resource setting with no functional computed tomography (CT) scan necessitates utmost dependence on plain X-rays for decision-making in patient care.
Case Description:We present our experience with a patient who presented in our facility with a right transorbital subfrontal arrow injury. The patient had retrograde extraction of the arrow based on plain X-ray findings with no sequelae.
Conclusion:We highlighted the role of X-ray in the management of arrow injuries, although bone window CT without or with angiography is the gold standard of imaging modalities in the management of patients with arrow injuries to the head.
Keywords: Arrow injury, Low-resource setting, Subfrontal, Transorbital, X-rays
INTRODUCTION
Arrow injuries, once thought to have gone into extinction with the prehistoric era, are now being seen in modern times both in the developed and developing world, with its rise on the increase in the developing world and especially in northern Nigeria as a result of the insurgence (Boko Haram) and increasingly the farmer-herder crisis.[
Although the injury involves the upper extremities commonly, the head and neck are also affected with increased frequency. The magnitude of the injury is dependent on the distance and tangent of the arrow; hence, an arrow shot at close range (<50 m) and right tangent can pierce through a very strong supraorbital ridge.[
Plain X-rays had been used in the precomputed tomography (CT) era to manage patients with arrow injuries.[
The management of arrow injury to the head entails proper resuscitation, wound debridement, extraction of the arrow under direct vision, hematoma evacuation, watertight dural closure, and empirical antibiotics.[
CASE REPORT
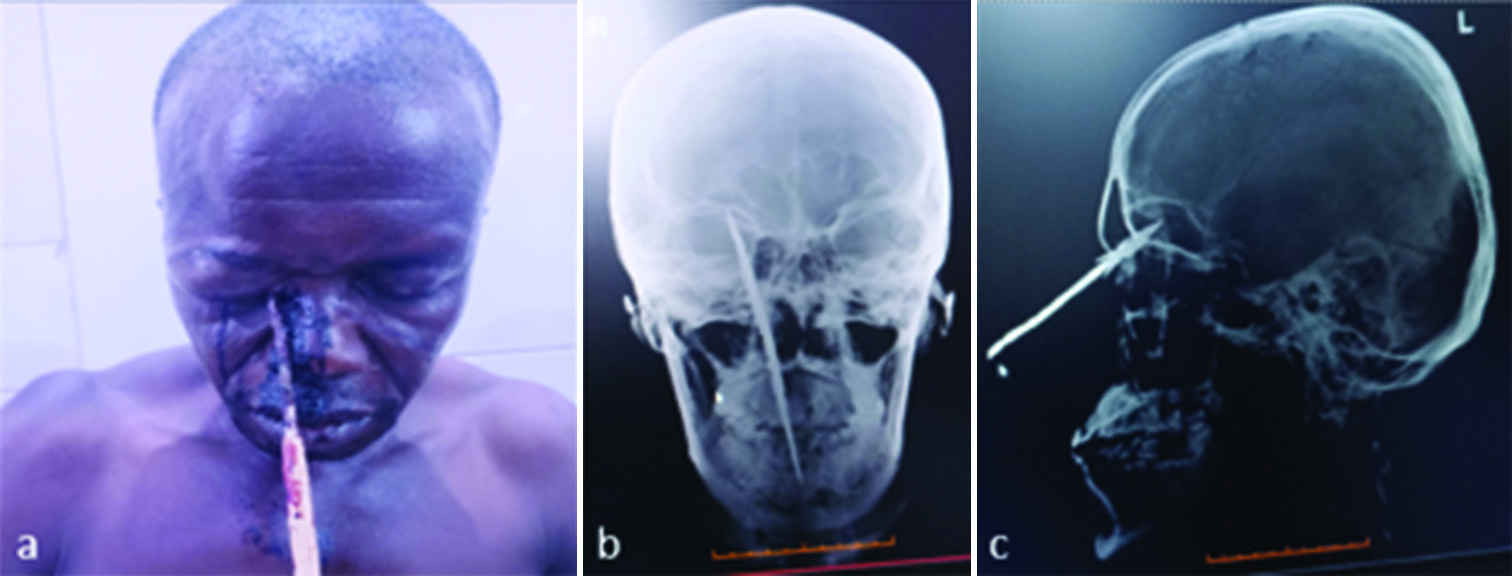
This is a 50-year-old right-handed male farmer who presented at the emergency department of our facility on account of arrowhead impalement in the right medial canthus and bleeding from the same spot following a farmer-herder altercation. However, there was no vomiting, visual impairment, personality change, seizure, loss of consciousness, or differential limb weakness. At the presentation, he was seen by the ophthalmology team, which involved the neurosurgery team on account of the skull X-ray findings of transorbital-sub-frontal arrowhead impalement with sub-frontal aerocele, sparing the globe. The arrowhead was just lateral to the right frontal sinus [
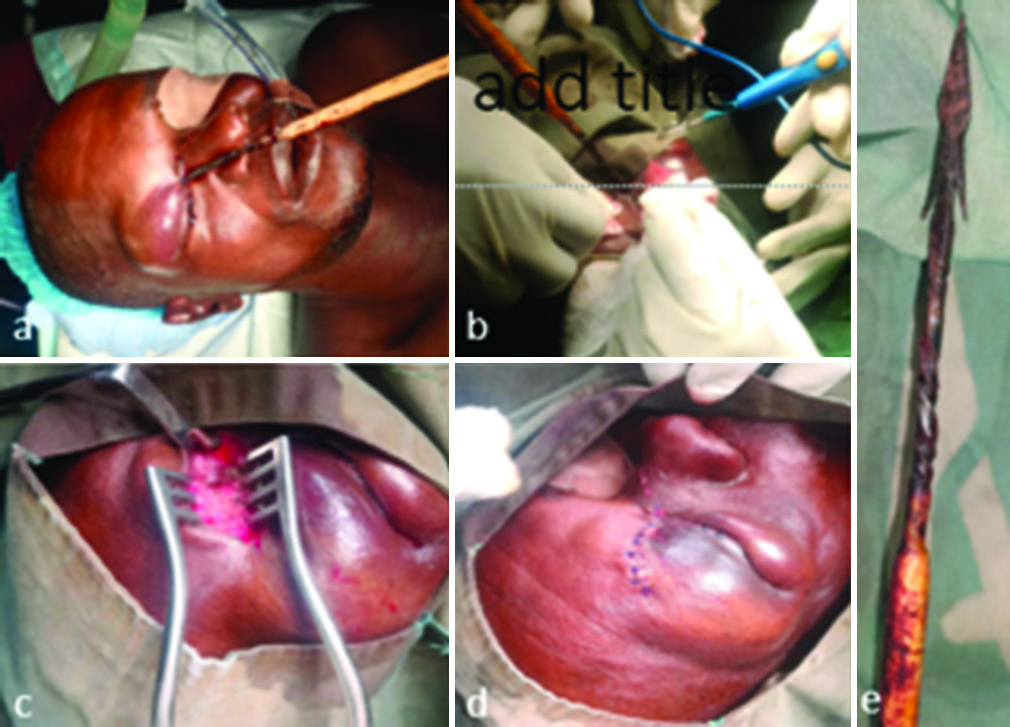
Intra-operatively, 20 cm arrow, 1 cm lateral to the right medial canthus in the upper eyelid, parallel to the midline, 80° to the skull base, with its 2.5 cm head and barbs buried in the substance of the muscle in the superomedial aspect of the right orbit and approximately 1 cm of the arrow tip attached to the orbital roof. Through a medial curvilinear superior eyelid incision extending to the entrance of the metallic shaft, the arrowhead was dissected out up to the dehisced orbital roof and was retrogradely extracted, and since there was no evidence of CSF egress on Valsalva maneuver, the wound was copiously irrigated with antibiotic-containing normal saline and closed in layers with the muscles apposed with 3/0 vicryl to reduce dead space and prevent CSF leak, the subcutaneous layer with 3/0 vicryl and the skin with 4/0 prolene (interrupted vertical mattress to allow for egress in the event of infective collection) as seen in
DISCUSSION
With the increase in high-velocity missiles such as shotguns and rifles due to banditry insurgency in northern Nigeria, the region has witnessed an increase in missile injuries. However, due to the same reasons, the resurgence of low (stab wounds) velocity and intermediate[
Bill, in his work, noted that arrow wounds are both punctured and incised.[
The index patient was a victim of the farmer-herdsmen crisis, which made up 20% of arrow injuries to the head and neck recorded by Adamu et al.,[
Due to the sponginess of the facial bones, arrows could lodge at various depths[
Arrow injuries are not commonly associated with mortality since, in most cases, the arrowheads tamponade vital vessels, and so it was admonished by Bill that the arrows may be extracted only in centers with facilities to manage such injuries. The patient arrived at our facility with a 20 cm snugly-fitting arrow (with its 2.5 cm head and barbs) buried in the right medial canthus and crusted blood around the entry point. The patient immediately had plain X-rays, which revealed the position of the arrow tip in the right median anterior skull base with subfrontal aerocele. Bone window with or without angiography (depending on the location of the arrowhead on X-ray) is a vital image modality in the management of cranial arrow injury. However, in the event where a CT scan is not functional,[
One option of surgery in this patient is a bifrontal craniotomy, breaking the arrow close to the entrance wound, anterograde extraction of the arrowhead, and cranialization and exenteration of the suspected involved frontal sinus. However, the morbidity and mortality involved in this option and considering our findings on plain skull X-ray made us opt for the safest option with the quickest recovery. Hence, we decided to extract the arrowhead whole retrogradely through the “superior medial transorbital extraconal subfrontal extradural approach.” There are many benefits of a transorbital approach, be it endoscopic or microscopic.[
CONCLUSION
Although CT bone window and angiography are the gold-standard imaging tools in arrow injury to the head, X-ray still has a role sometimes as a standalone imaging tool in low-resource settings. Retrograde extraction of arrowheads can still be done if the arrowhead has not gone deeply intracranial after careful dissection of the surrounding soft tissue from the arrow barbs.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Abdullahi H, Adamu A, Hasheem MG. Penetrating arrow injuries of the head-and-neck region: Case series and review of literature. Niger Med J. 2020. 61: 276-80
2. Adamu A, Garandawa HI, Nuhu AM, Farate A, Kodiya AM, Abdulrazaq A. A review of arrow shot injuries to the head and neck in Northeastern Nigeria. Borno Med J. 2021. 18: 1-7
3. Aref M, Kunigelis KE, Yang A, Subramanian PS, Ramakrishnan VR, Youssef AS. The effect of preoperative direct ligation of ethmoidal arteries on the perioperative outcomes of large anterior skull base meningiomas surgery: A clinical study. World Neurosurg. 2018. 120: e776-82
4. Bill JH, Arshhust J, editors. Sabre and Bayonnete wounds, arrow wounds. The International Encyclopedia of Surgery: A systematic treatise on the theory and practice of surgery. United States: William Wood; 1882. 2: 101-7
5. De Jongh K, Dohmen D, Salgado R, Ozsarlak O, Van Goethem JW, Beaucourt L. “William Tell” injury: MDCT of an arrow through the head. AJR Am J Roentgenol. 2004. 182: 1551-3
6. De Notaris M, Sacco M, Corrivetti F, Grasso M, Corvino S, Piazza A. The transorbital approach, a game-changer in neurosurgery: A guide to safe and reliable surgery based on anatomical principles. J Clin Med. 2023. 12: 6484
7. De Simone M, Zoia C, Choucha A, Kong DS, De Maria L. The transorbital approach: A comprehensive review of targets, surgical techniques, and multiportal variants. J Clin Med. 2024. 13: 2712
8. Di Ieva A, Lee J, Cusimano M, editors. Handbook of skull base surgery. Uttar Pradesh: Thieme Publishers; 2016. p. 43-6
9. Feller C, Martinez Del Campo E, Eraky AM, Montoure A, Maloley L, Harrison G. Transorbital approach for resection of intracranial skull base lesions: Outcomes and complications. Interdiscip Neurosurg. 2023. 32: 101747
10. Floreani SR, Nair SB, Switajewski MC, Wormald PJ. Endoscopic anterior ethmoidal artery ligation: A cadaver study. Laryngoscope. 2006. 116: 1263-7
11. Gifford TO, Orlandi RR. Epistaxis. Otolaryngol Clin North Am. 2008. 41: 525-36 viii
12. Hammon WM. Analysis of 2187 consecutive penetrating wounds of the brain from Vietnam. J Neurosurg. 1971. 34: 127-31
13. Harsh V, Alda H, Singh S, Kumar J, Sahay CB, Kumar A. Arrowhead injury of central nervous system: Three rare cases from rural India. Indian J Neurotrauma. 2021. 18: 138-41
14. Ibrahim AI, Murhega RB, Samuila S. A hunting arrow traumatism to the head: A case report from Niger. Clin Case Rep. 2023. 11: e7750
15. Madziga AG. Arrow injuries in North East Nigeria. West Afr J Med. 2003. 22: 106-9
16. Mono J, Hollenberg RD, Harvey JT. Occult transorbital intracranial penetrating injuries. Ann Emerg Med. 1986. 15: 589-91
17. O’Neill OR, Gilliland G, Delashaw JB, Purtzer TJ. Transorbital penetrating head injury with a hunting arrow: Case report. Surg Neurol. 1994. 42: 494-7
18. Ogunleye AO, Adeleye AO, Ayodele KJ, Usman MO, Shokunbi MT. Arrow injury to the skull base. West Afr J Med. 2004. 23: 94-6
19. Paramhans D, Shukla S, Batra A, Mathur RK. Successful removal of an impacted metallic arrowhead penetrating up to the brainstem. J Emerg Trauma Shock. 2010. 3: 303
20. Shereen R, Oskouian RJ, Loukas M, Tubbs RS. Treatment of arrow wounds: A review. Cureus. 2018. 10: e2473
21. Szczepanek E, Toppich J, Ostrowski P, Bonczar M, Nasser A, Dziedzic M. The complete anatomy of the anterior ethmoidal artery: A Meta-analysis with implications for sinus and skull base surgery. J Clin Med. 2024. 13: 1695
22. Usman B, Mohammed B, Shuwa FA, Garandawa HI. Penetrating intracranial arrow extraction: Our experience. Borno Med J. 2020. 17: 1-7
23. White DV, Sincoff EH, Abdulrauf SI. Anterior ethmoidal artery: Microsurgical anatomy and technical considerations. Neurosurgery. 2005. 56: 406-10 discussion 406-10
24. Yamamoto H, Nomura K, Hidaka H, Katori Y, Yoshida N. Anatomy of the posterior and middle ethmoidal arteries via computed tomography. SAGE Open Med. 2018. 6: 2050312118772473







Clinton Frederick Miller II MD FAANS
Posted November 11, 2024, 11:08 am
The authors are to be congratulated on their management. They might be interested in our review article: Miller, CF, Brodkey, GR, Colombi, BS: The Danger of Intracranial Wood: Surgical Neurology 1977 Feb; 7 (2): 95-103
E G Sunday
Posted November 12, 2024, 8:53 pm
Thank you for your kind words. The article was insightful. We will follow up the patient for a long period to track his progress and watch out for the complications stated in your article abstract. More so, I would like you let me have the full article. Thank you
Clinton Frederick Miller II MDc
Posted November 13, 2024, 5:15 pm
Send me your mailing address in Nigeria and I shall be happy to send you an original offprint of the article: The Danger of Intracranial Wood!!
E G Sunday
Posted November 14, 2024, 7:09 pm
emistocrate@yahoo.com
emistotle@gmail.com