- Department of Neurological Surgery, University of South Dakota, Sanford School of Medicine, SD, USA
- Neurological Surgery, Rapid City Regional Hospital, Rapid City, SD, USA
Correspondence Address:
Kelly E. Wong
Neurological Surgery, Rapid City Regional Hospital, Rapid City, SD, USA
DOI:10.4103/sni.sni_434_16
Copyright: © 2017 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Kelly E. Wong, Peter S. Chang, Mark S. Monasky, Rodney M. Samuelson. Traumatic spondyloptosis of the cervical spine: A case report and discussion of worldwide treatment trends. 26-May-2017;8:89
How to cite this URL: Kelly E. Wong, Peter S. Chang, Mark S. Monasky, Rodney M. Samuelson. Traumatic spondyloptosis of the cervical spine: A case report and discussion of worldwide treatment trends. 26-May-2017;8:89. Available from: http://surgicalneurologyint.com/surgicalint-articles/traumatic-spondyloptosis-of-the-cervical-spine-a-case-report-and-discussion-of-worldwide-treatment-trends/
Abstract
Background:Cervical spondyloptosis is defined as the dislocation of the spinal column most often caused by trauma. Due to compression or transection of the spinal cord, severe neurological deficits are common. Here, we review the literature and report a case of traumatic C5–6 spondyloptosis that was successfully treated using an anterior-only surgical approach.
Methods:The patient presented with quadriplegia and absent sensation distal to the C5 dermatome following a rollover motor vehicle accident. The preoperative American Spinal Injury Association Impairment Scale was A. Computed tomography of the cervical spine revealed C5–6 spondyloptosis, lamina fractures on the right side at the C3–4 level, and widened facet joint on the right side at C6–7.
Results:The patient underwent cervical traction and anterior cervical discectomy and fusion at the C5–6, C6–7 levels; no 360° fusion was warranted. Six months postoperatively, the patient remained quadriplegic below the C5 level.
Conclusion:Presently, no consensus is present regarding the best treatment for spondyloptosis. Worldwide, the 360° approach is the most commonly used (45%), followed by anterior-only surgery (31%) and posterior-only surgery (25%). The surgical choice depends upon patient-specific features but markedly varies among geographical regions.
Keywords: Cervical, trauma, spondylolisthesis, spondyloptosis
INTRODUCTION
Cervical spondyloptosis, an exceedingly rare entity, may be caused by congenital or neoplastic entities.[
CASE HISTORY
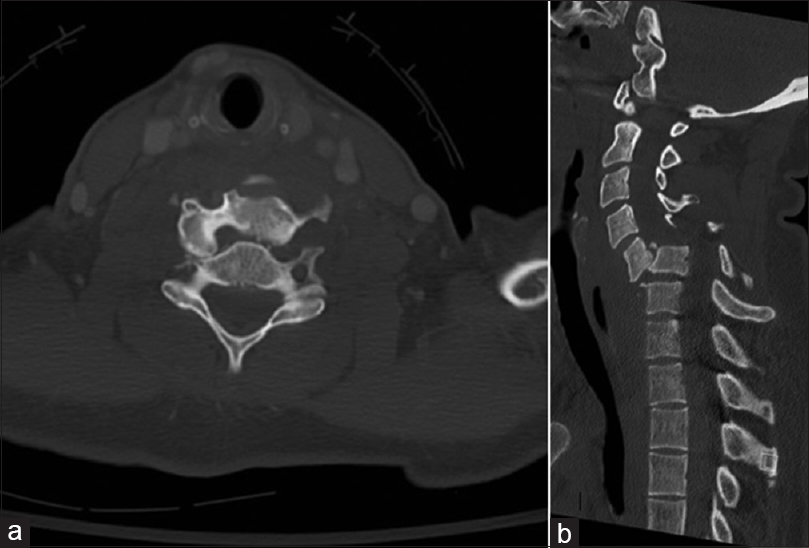
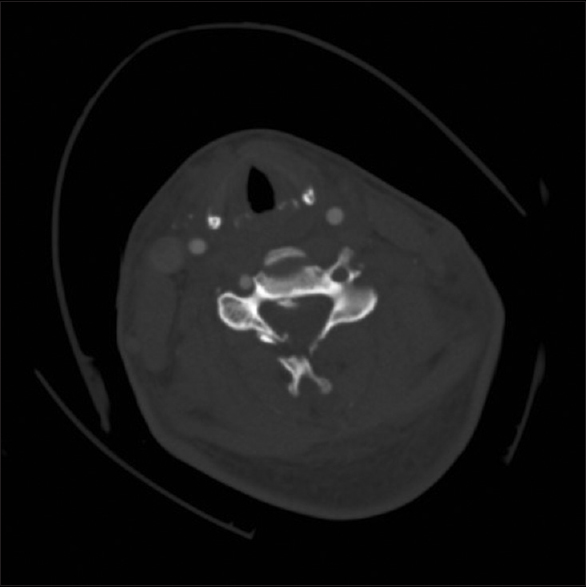
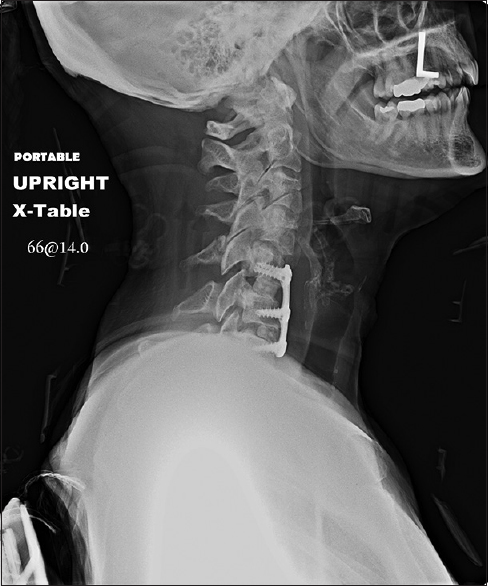
A 49-year-old woman presented with neck pain, quadriplegia, and a complete motor and sensory deficit at the C5 level attributed to a rollover motor vehicle accident. Her preoperative American Spinal Injury Association Impairment Scale (ASIA) was A. Computed tomography (CT) of the cervical spine demonstrated C5–6 spondyloptosis, superior and inferior lamina fractures on the right at the C3–4 level, and widened facet joint on the right at C6–7 [
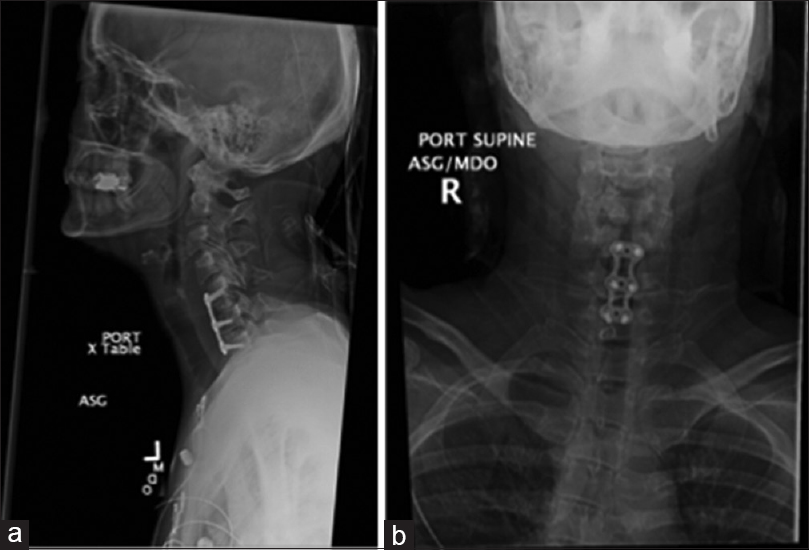
Preoperative partial anatomic reduction was achieved using Gardner–Wells traction and incrementally increased to 30 lbs (13.6 kg) under direct fluoroscopy. The patient was treated with anterior C5–6 and C6–7 discectomy with fusion (Puros S2 allograft bone grafts; Zimmer Spine, Minneapolis, MN, USA) and a 40-mm Invizia (Zimmer Spine; plates C5–C7); no posterior stabilization was used [
Postoperative angiography
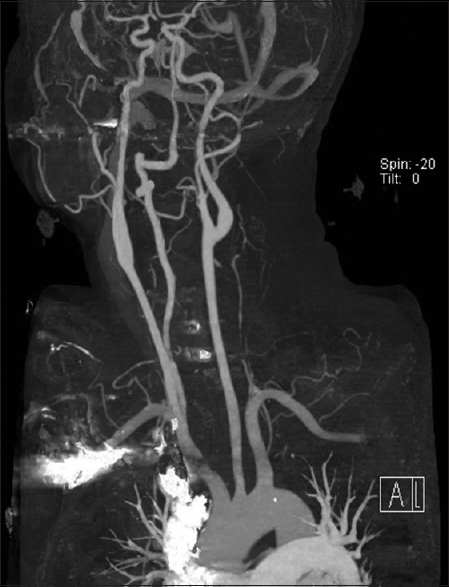
Postoperative CT angiography showed dissection and occlusion of the left vertebral artery originating at the C4–5 level with distal reconstitution via muscular collaterals [Figures
Postoperative status
Postoperatively, the patient showed ASIA A at a C5 motor and sensory level. The patient was discharged to a rehabilitation hospital on postoperative day 5; her condition remained unchanged 6 months later [
MATERIALS AND METHODS
We reviewed the literature on spondyloptosis, including grade 5 spondylolithesis, and found 32 cases in total. Our case is the 33rd such case. Variables assessed included the author, year, age, sex, injury level, injury mechanism, ASIA level (preoperative and postoperative), follow-up duration, surgical management choice, and country of origin. All single-staged 360° (anterior–posterior or posterior–anterior) or 540° (anterior–posterior–anterior or posterior–anterior–posterior) procedures were included under category 360°.
Statistical analysis
SPSS (Version 17, IBM, Chicago, IL, USA) was used for statistical analysis, and categorical variables were noted in number of patients (%). This relied on Pearson's Chi-squared test to compare the surgical approaches with regard to sex, geographical region (USA, Asia, and Europe), injury level, preoperative ASIA grade, immediate postoperative ASIA grade, and postoperative ASIA grade at the end of the follow-up period. P < 0.05 was considered statistically significant.
RESULTS
Clinical data
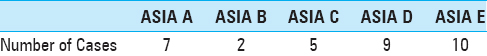
Thirty-three total cases of traumatic spondyloptosis were identified in the literature. The average patient age was 46.8 years; 24 were men and 9 were women [
Mechanism and severity of injury
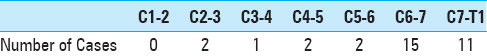
Motor vehicle accidents were predominant, followed by being struck by falling objects, assault, and iatrogenic causes. Of the 24 cases that were followed, the mean follow-up was 13.63 months (2–60 months). The predominant levels were C6–7 (45.5%) and C7–T1 (33.3%) [
Surgery
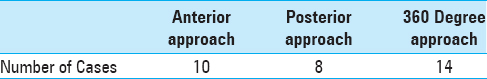
Thirty-two patients had received surgical treatment; only one patient, who was neurologically intact, refused surgery. Surgery was performed anteriorly alone in 31.3% of cases and posteriorly only in 25.0% of cases; 43.8% of cases underwent 360° repair. Only two cases (6.3%) were treated in a staged manner [
Complications
Four cases experienced worsening: Two demonstrated a deterioration of the neurological status (6.3%), one developed basal artery thrombosis leading to death (3.1%),[
Distribution of cases
Half of the cases were present in Asia, 43.8% in the United States, and 6.3% in Europe. The anterior-only approach was used significantly more frequently in Asia, whereas the posterior-only approach was significantly more common in the United States (P = 0.004). The 360° repair was used significantly more frequently in Asia, whereas the posterior-only approach was significantly more common in the United States (P = 0.003).
DISCUSSION
Cervical spondyloptosis typically results from severe hyperextension injury with bilateral pedicle fractures, and bilateral locked facets, with or without fracture of the laminae.[
Surgical fusions
The definitive management of spondyloptosis is through surgical fixation.[
Varying treatment choices
The treatment choice for patients with spondyloptosis widely varies. Surgical options include anterior cervical discectomy and fusion only, posterior lateral mass fusion with or without laminectomy, and 360° fusion.[
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Acikbas C, Gurkanlar D. Post-traumatic C7-T1 Spondyloptosis in a patient without neurological deficit: A case report. Turk Neurosurg. 2010. 20: 257-60
2. Dahdaleh NS, Dlouhy BJ, Greenlee JD, Smoker WR, Hitchon PW. An algorithm for the management of posttraumatic cervical spondyloptosis. J Clin Neurosci. 2013. 20: 951-7
3. Goffin J, Grob D. Spondyloptosis of the cervical spine in neurofibromatosis. A case report. Spine. 1999. 24: 587-90
4. Jayakumar P, Choi D, Casey A. Late presentation of a type III axis fracture with spondyloptosis. Ann R Coll Surg Engl. 2008. 90: W1-3
5. Keskin F, Kalkan E, Erdi F. The surgical management of traumatic c6-c7 spondyloptosis. J Korean Neurosurg Soc. 2013. 53: 49-51
6. Lee CW, Hwang SC, Im SB, Kim BT, Shin WH. Traumatic Thoracic Spondyloptosis: A Case Report. J Korean Neurosurg Soc. 2004. 35: 622-4
7. Mamindla RK, Kumar A, Bhattacharjee S, Sahu BP. A novel case of “ambulatory” cervical spondyloptosis: Case report with literature review. Eur Spine J. 2014. 23: 161-6
8. Menku A, Kurtsoy A, Tucer B, Oktem IS, Akdemir H. The surgical management of traumatic C6-C7 spondyloptosis in a patient without neurological deficits. Minim Invasive Neurosurg. 2004. 47: 242-4
9. Munakomi S, Bhattarai B, Cherian I. Traumatic Cervical Spondyloptosis in a Neurologically Stable Patient: A Therapeutic Challenge. Case Rep Crit Care. 2015. 2015: 540919-
10. Padwal A, Shukla D, Bhat DI, Somanna S, Devi BI. Post-traumatic cervical spondyloptosis: A rare entity with multiple management options. J Clin Neurosci. 2016. 28: 61-6
11. Ramieri A, Domenicucci M, Cellocco P, Lenzi J, Dugoni DE, Costanzo G. Traumatic spondylolisthesis and spondyloptosis of the subaxial cervical spine without neurological deficits: Closed re-alignment, surgical options and literature review. Eur Spine J. 2014. 23: 658-63
12. Srivastava SK, Agrawal KM, Sharma AK, Agrawal MD, Bhosale SK, Renganathan SR. C3-C4 spondyloptosis without neurological deficit-a case report. Spine J. 2010. 10: e16-20
13. Tumialan LM, Dadashev V, Laborde DV, Gupta SK. Management of traumatic cervical spondyloptosis in a neurologically intact patient: Case report. Spine. 2009. 34: E703-8
14. Tumialan LM, Theodore N. Basilar artery thrombosis after reduction of cervical spondyloptosis: A cautionary report. J Neurosurg Spine. 2012. 16: 492-6
15. Wild A, Jager M, Werner A, Eulert J, Krauspe R. Treatment of congenital spondyloptosis in an 18-month-old patient with a 10-year follow-up. Spine. 2001. 26: E502-5