- Department of Orthopedic Surgery, Akita Kousei Medical Center, Hondo, Japan
- Department of Orthopedic Surgery, Akita University Graduate School of Medicine, Hondo, Japan
- Department of Orthopedic Surgery, Yuri Kumiai General Hospital, Yurihonjo, Akita, Japan.
Correspondence Address:
Dr. Yoshinori Ishikawa, Department of Orthopedic Surgery, Akita Kousei Medical Center, Akita, Japan.
DOI:10.25259/SNI_830_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Yoshinori Ishikawa1, Naohisa Miyakoshi2, Takashi Kobayashi1, Toshihiko Kikuchi3. Treatment of progressive paralysis associated with cervical myelopathy and suspected amyotrophic lateral sclerosis: A case report. 02-Nov-2021;12:550
How to cite this URL: Yoshinori Ishikawa1, Naohisa Miyakoshi2, Takashi Kobayashi1, Toshihiko Kikuchi3. Treatment of progressive paralysis associated with cervical myelopathy and suspected amyotrophic lateral sclerosis: A case report. 02-Nov-2021;12:550. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=11206
Abstract
Background: Amyotrophic lateral sclerosis (ALS) is an intractable progressive disease, with an incidence of 2.2– 2.3 per 100,000 individuals, which is not extremely low. ALS symptoms are accompanied by spinal myeloradicular motor deficit; its differential diagnosis is must because progressive paralysis needs emergency surgery.
Case Description: A 64-year-old man with suspected ALS showing progressive paralysis with cervical myelopathy was diagnosed as normal after performing a nerve conduction study preoperatively. Postoperative diffuse fasciculation after posterior decompression allowed the diagnosis of ALS through needle electromyography (EMG). Thereafter, the patient’s condition slowly deteriorated and he died after 16 months.
Conclusion: Surgery might aggravate ALS symptoms; however, surgery for progressive paralysis in patients with suspected ALS is required for distinguishing patients with non-ALS paralysis. Approximately 70% of cases have spinal-onset ALS lacking typical cranial nerve symptoms; thus, to prevent unnecessary surgery, surgeons should at least know the characteristic features of ALS and should be aware that early diagnosis requires needle EMG for definitive diagnosis of ALS.
Keywords: Amyotrophic lateral sclerosis, Cervical myelopathy, Needle electromyography, Progressive paralysis, Treatment
INTRODUCTION
Amyotrophic lateral sclerosis (ALS) is an intractable progressive disease, with an incidence of 2.2–2.3 per 100,000 individuals,[
A patient with spinal cord compression and suspected ALS lacking typical sensory deficit, who consulted a neurologist preoperatively, presented with progressive arm drop and difficulty in standing. Postoperative diffuse fasciculation was noted on a video, which lead to the definitive diagnosis of ALS with needle electromyography (EMG). Here, the postoperative course of a missed-definitive diagnosis of ALS paralysis is presented and ways to prevent unnecessary surgical treatment for such ALS patients were retrospectively reflected.
CASE REPORT
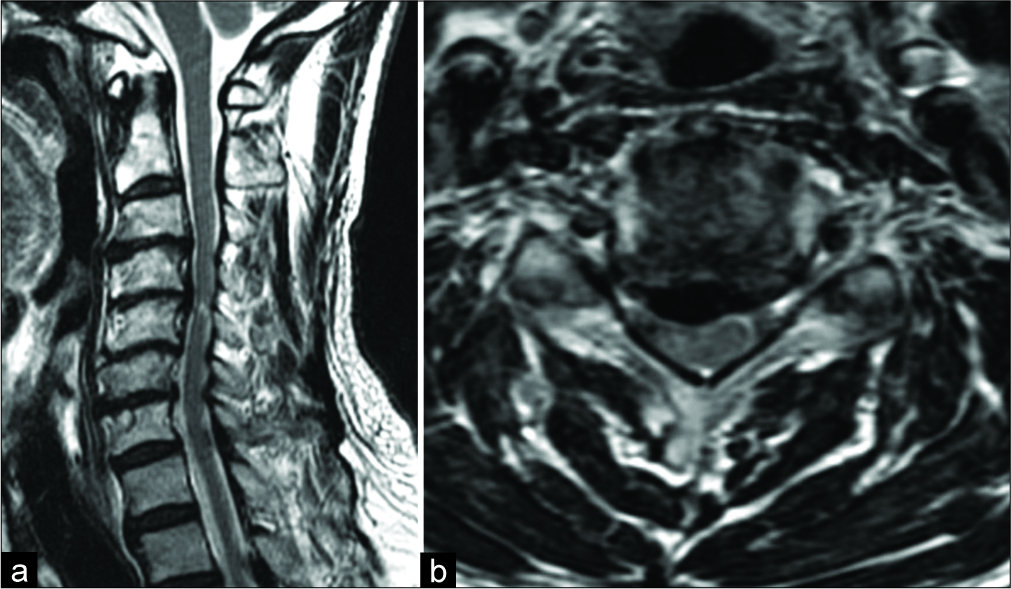
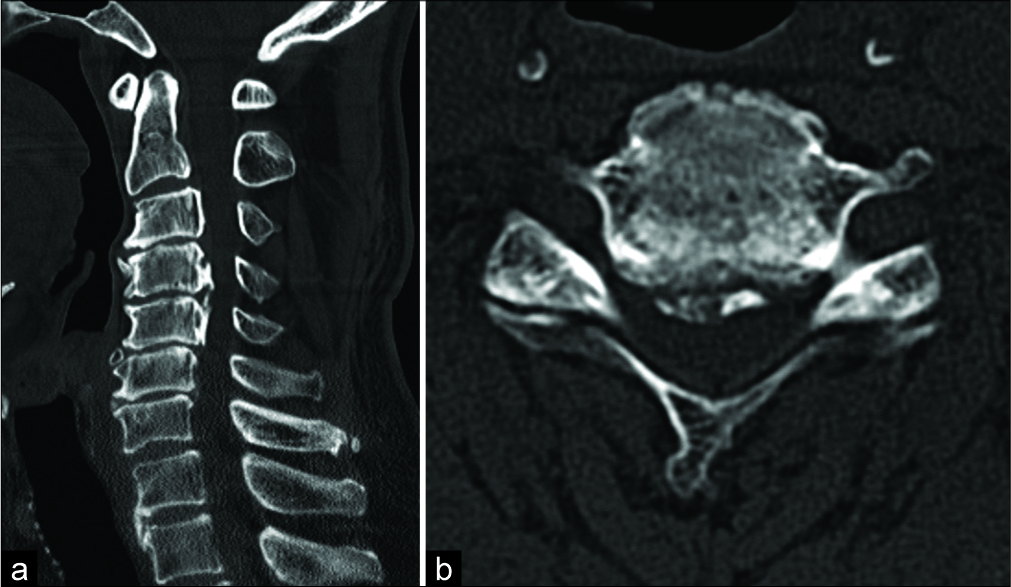
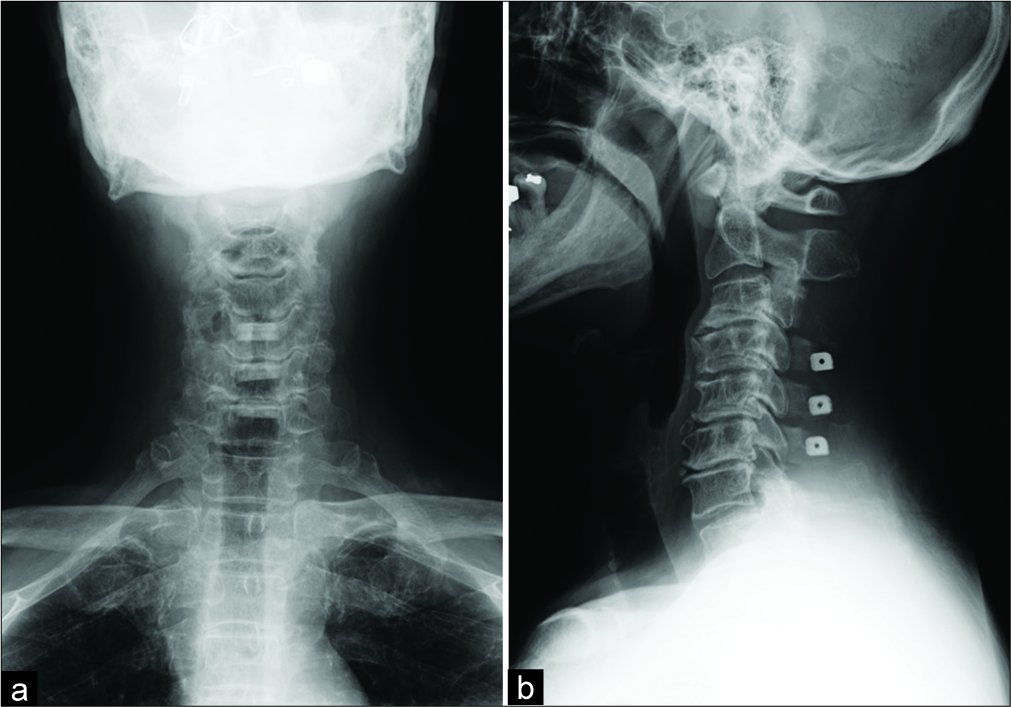
A 64-year-old man, with no significant history except lumbar surgery with foot drop and sciatica, noted difficulty in right shoulder elevation, walking, and using chopsticks for a month. Physical examination revealed hyperreflexia and motor weakness in the upper limbs (shoulder elevation 3/5, elbow flexion 4/5, and finger extension 2-/3) and slow stream of urination without sensory disturbance. Bilateral Hoffman sign and Babinski sign were positive. Despite previous lumbar surgery, foot drop progressed bilaterally without numbness or sensory disturbance, implying the presence of motor neuron disease (MND). Imaging studies revealed canal narrowing at multiple locations with ossification of the posterior longitudinal ligament and spinal cord compression with T2 signal change at C4–C5 [
Video 1
DISCUSSION
The percentage of motor cells decrease to 30% at 1 year, and the mean duration for artificial ventilation is 3 years after ALS onset.[
Avoiding surgery is better; however, treatment of progressive severe paralysis for suspected case without definitive diagnosis is unknown. Our emergent surgical indication for cervical spinal cord decompression is acute progressive paralysis accompanied by inability to stand or move extremities against gravity. In case with symptoms that do not clearly fit the criteria for cervical myelopathy, we consult a neurologist preoperatively. Spinal-onset ALS is noted in 67.4% of individuals without typical cranial or bulbar symptoms;[
Only 10% of patients have familial ALS with hereditary cause; thus, genetic diagnosis is not always required. Indeed, several genes lead to better understanding of ALS, but remission is impossible. ALS symptoms continue to deteriorate and never improve; however, simultaneous myeloradiculopathy might show improvement with decompression surgery. Such information should be examined in eligible patients preoperatively. Some drugs have been reported to delay progression; therefore, only early definitive ALS diagnosis can lead to a better quality of life in patients with ALS.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Video available on:
References
1. Arasaki K, Tamaki M. A loss of functional spinal alpha motor neurons in amyotrophic lateral sclerosis. Neurology. 1998. 51: 603-5
2. de Carvalho M, Dengler R, Eisen A, England JD, Kaji R, Kimura J. Electrodiagnostic criteria for diagnosis of ALS. Clin Neurophysiol. 2008. 119: 497-503
3. Doi Y, Atsuta N, Sobue G, Morita M, Nakano I. Prevalence and incidence of amyotrophic lateral sclerosis in Japan. J Epidemiol. 2014. 24: 494-9
4. Kanbayashi T, Mikata T, Hatanaka Y, Sonoo M. Amyotrophic lateral sclerosis with a sudden-onset history. Clin Neurophysiol Pract. 2017. 2: 103-4
5. Kihira T, Kanno S, Miwa H, Okamoto K, Kondo T. The role of exogenous risk factors in amyotrophic lateral sclerosis in Wakayama, Japan. Amyotroph Lateral Scler. 2007. 8: 150-6
6. Pinto S, Swash M, de Carvalho M. Does surgery accelerate progression of amyotrophic lateral sclerosis?. J Neurol Neurosurg Psychiatry. 2014. 85: 643-6
7. Watanabe H, Atsuta N, Hirakawa A, Nakamura R, Nakatochi M, Ishigaki S. A rapid functional decline type of amyotrophic lateral sclerosis is linked to low expression of TTN. J Neurol Neurosurg Psychiatry. 2016. 87: 851-8
8. Yoshor D, Klugh A, Appel SH, Haverkamp LJ. Incidence and characteristics of spinal decompression surgery after the onset of symptoms of amyotrophic lateral sclerosis. Neurosurgery. 2005. 57: 984-9