- Departments of Orthopedics, NYU Winthrop Hospital, Mineola, NY, USA.
- Departments of Neurosurgery, NYU Winthrop Hospital, Mineola, NY, USA.
- Departments of Clinical Professor of Neurological Surgery, School of Medicine, State University of New York at Stony Brook, NY, USA.
Correspondence Address:
Nancy E. Epstein
Departments of Neurosurgery, NYU Winthrop Hospital, Mineola, NY, USA.
Departments of Clinical Professor of Neurological Surgery, School of Medicine, State University of New York at Stony Brook, NY, USA.
DOI:10.25259/SNI_243_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Marc Agulnick, Benjamin R. Cohen, Nancy E. Epstein. Unique Bone Suture Anchor Repair of Complex Lumbar Cerebrospinal Fluid Fistulas. Surg Neurol Int 13-Jun-2020;11:153
How to cite this URL: Marc Agulnick, Benjamin R. Cohen, Nancy E. Epstein. Unique Bone Suture Anchor Repair of Complex Lumbar Cerebrospinal Fluid Fistulas. Surg Neurol Int 13-Jun-2020;11:153. Available from: https://surgicalneurologyint.com/surgicalint-articles/10082/
Abstract
Background: Spine surgeons encounter occasional complex cerebrospinal fluid fistulas/dural tears (CSF/DT) during lumbar spinal surgery. In some cases, these leaks are found during the index procedure, but others may appear postoperatively, or in the course of successive procedures. Here we asked, whether these complex CSF fistulas/DT could be more readily repaired utilizing a “bone suture anchor” technique, particularly where there is no residual dural margin/remnant.
Methods: With the combined expertise of the orthopedist and neurosurgeon, mini/micro bone suture anchors, largely developed for hand surgery, facilitated repair of complex DT occurring during lumbar spine surgery. This technique was utilized to suture in place fascia, periosteal, or muscle grafts, and was followed by the application of microfibrillar collagen, and a fibrin sealant.
Results: This mini/micro suture anchor technique has now been utilized to repair multiple significant intraoperative and/or postoperative recurrent DT, largely avoiding the need to place lumbar drains and/or lumbo- peritoneal shunts.
Conclusions: Here, we reviewed how to directly suture dural grafts utilizing a mini/micro bone suture anchor technique to repair complex intraoperative primary/recurrent DT occurring during lumbar spine surgery. The major advantages of this technique, in addition to obtaining definitive occlusion of the DT, largely avoids the need to place lumbar drains and/or lumbo-peritoneal shunts with their attendant risks and complications.
Keywords: Massive, Dural Leak, Lumbar, Suture Anchors, Patch Grafts, Complex Repair
INTRODUCTION
Dealing with major primary and/or recurrent cerebrospinal fluid fistulas/dural tears (CSF/DT) occurring during complex lumbar surgery may be problematic. For primary cases or revision surgery (i.e. with significant postoperative scarring), there may be insufficient to no lateral dura present to “sew to”, precluding attaining a “water-tight” dural closure. In these situations, where it is optimal to fully close the dura, by applying fascia, sheep pericardium, muscle patch/other dural grafts (“graft material”), the surgeon should be able to close the dura utilizing mini/micro bone suture anchors, typically employed in hand surgery [
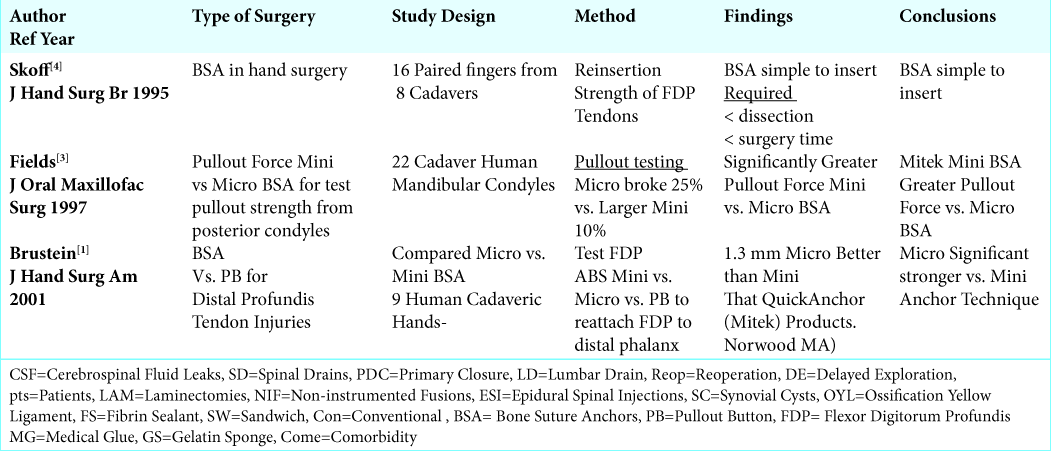
Figure 1:
Biotek Titanium Mini-Vim-Suture-Anchor (Arthroscopic Implants). This mini-Vim-Suture-Anchor-with-Needle is produced by Biotek and the anchor portion is made of Titanium. It is 2.8 mm to 3.5 mm in diameter, and 2.8 mm wide. They come preloaded with USP #2 BioFiber suture. In most cases it can be inserted without the need for a drill, although one is available.
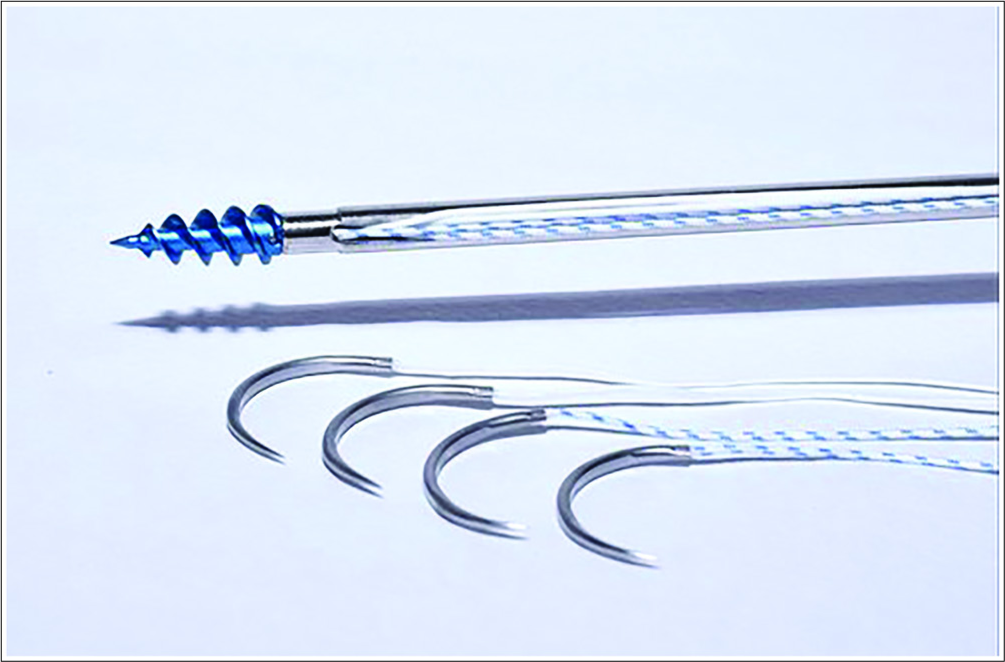
Figure 2:
Depuy Mitek Mini Gill II Titanium Anchor Suture Anchor (QuickAnchor: DepuySynthes, Part of Johnson&Johnson Family Companies). The nitinol arcs are used to reattach soft-tissues to bone. The GII Anchor is small with a high pull-out strength. The drill hole is 2.4 x 8.8mm. It utilizes multiple suture types including ORTHOCORD®, PANACRYL® & ETHIBOND®. It’s indications for use include Ulnar or lateral collateral ligament reconstruction in the hand.
Bone Suture Anchor Techniques in Orthopedics
Composition of Mimi/Micro Bone Suture
Bone Suture Anchors are utilized in orthopedics typically for affixing tendons and ligaments to bone [
Sutures Utilized with the Bone Suture Anchors
The sutures themselves, which may or may not come preloaded, consist of braided polyester sutures or ultrahigh molecular weight polyethylene [
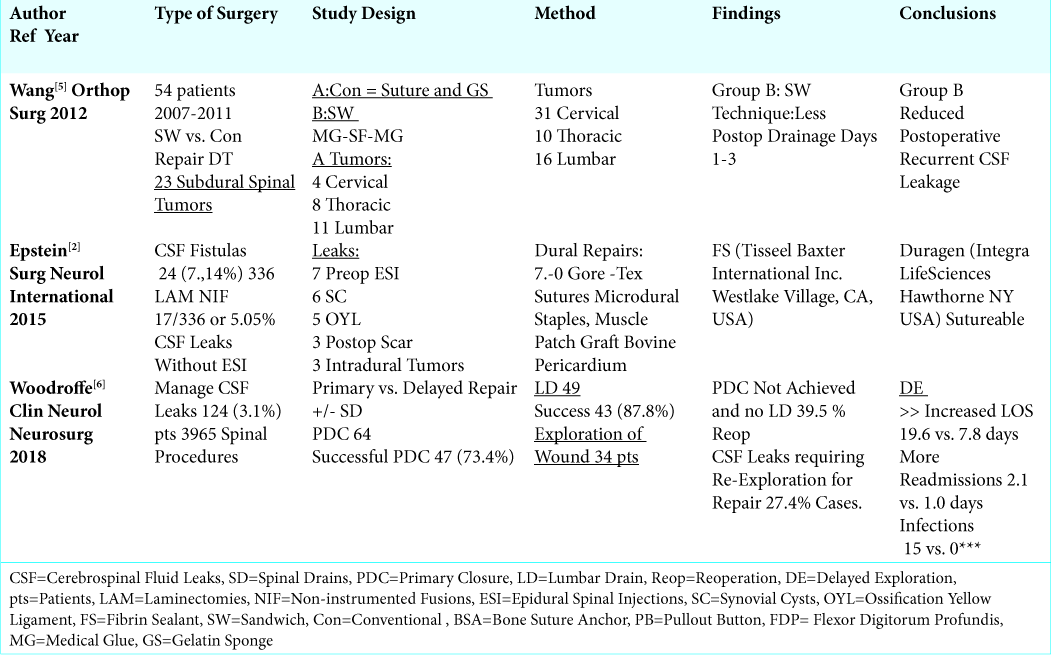
Bone Suture Anchor Repairs in Hand Surgery
In hand surgery, mini and/or micro bone suture anchor (BSA) techniques have been utilized for decades. [
Suture Anchor Repairs in Maxillofacial Surgery
In 1997, in the Journal of Maxillofacial Surgery, Fields et al. evaluated the pullout force of mini vs. micro bone suture anchors re: pullout strength from 22 cadaveric posterior mandibular condyles [
Incidence of Dural Tears (DT) and Treatment Modalities in Lumbar Surgery
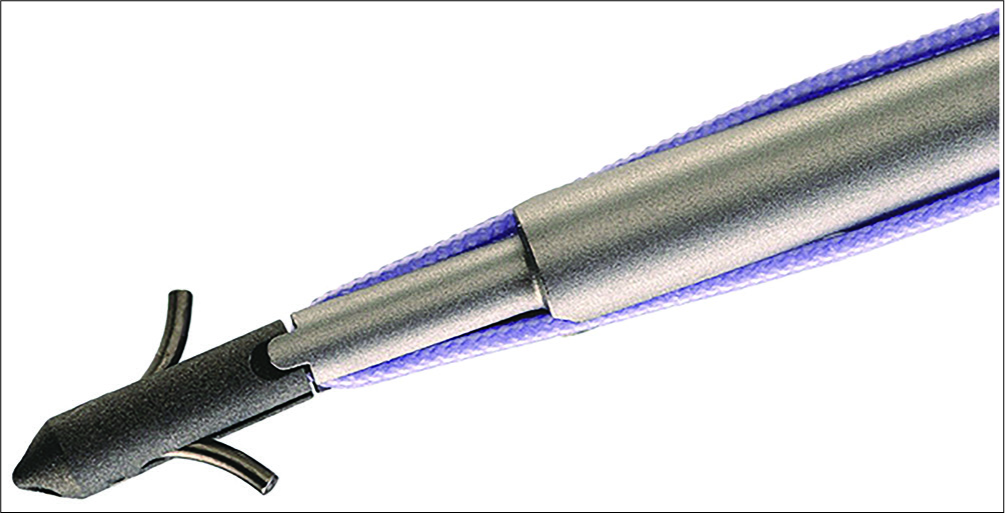
Different lumbar studies report varying frequencies of intraoperative dural fistulas and repair techniques [
Proposed Micro Bone Suture Anchor Repair of Complex Lumbar Dural Defects
Patients undergoing primary, secondary, or multiple reoperations to repair major lumbar dural defects may require mini/micro bone suture anchors to achieve adequate dural repair [
CONCLUSION
It may be difficult to treat complex primary and/or recurrent cerebrospinal fluid fistulas/dural tears (CSF/DT) that have occurred during lumbar surgery [
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Brustein M, Pellegrini J, Choueka J, Heminger H, Mass D. Bone suture anchors versus the pullout button for repair of distal Profundis tendon injuries: a comparison of strength in human cadaveric hands. J Hand Surg Am. 2001. 26: 489-96
2. Epstein NE. Incidence and management of cerebrospinal fluid fistulas in 336 multilevel laminectomies with non-instrumented fusions. Surgical Neurol International. 2015. 6: S463-8
3. Fields RT, Cardenas LE, Wolford LM. The pullout force for Mitek mini and micro suture anchor systems in human mandibular condyles. J Oral Maxillofac Surg. 1997. 55: 483-7
4. Skoff HD, Hecker AT, Hayes WC, Sebell-Sklar R, Straughn N. Bone suture anchors in hand surgery. J Hand Surg Br. 1995. 20: 245-8
5. Wang HR, Cao SS, Jiang YQ, Li JN, Li XL, Fu YG. A comparison between “sandwich” and conventional methods of repairing spinal dura rupture. Orthop Surg. 2012. 4: 233-40
6. Woodroffe RW, Nourski KV, Helland LC, Walsh B, Noeller J, Kerezoudis P. Management of iatrogenic spinal cerebrospinal fluid leaks: A cohort of 124 patients. Clin Neurol Neurosurg. 2018. 170: 61-66