- Department of Medicine, Faculty of Health Sciences, Universidad Anáhuac,
- Neurological Center, Centro Médico ABC,
- Department of Neurological Surgery, Hospital Ángeles Pedregal,
- Department of Neurological Surgery, Instituto Nacional de Neurología y Neurocirugía “Manuel Velasco Suárez”,
- Department of Internal Medicine, Fundación Clínica Médica Sur.
Correspondence Address:
Luis Alberto Ortega-Porcayo, Department of Neurological Surgery, Hospital Ángeles Pedregal, Mexico City, Mexico.
DOI:10.25259/SNI_140_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Júlia Moscardini-Martelli1, Juan Antonio Ponce-Gomez2,3,4, Victor Alcocer-Barradas3,4, Samuel Romano-Feinholz2, Pilar Padilla-Quiroz5, Marcela Osuna Zazueta2,3, Luis Alberto Ortega-Porcayo1,2,3. Upward transtentorial herniation: A new role for endoscopic third ventriculostomy. 06-Jul-2021;12:334
How to cite this URL: Júlia Moscardini-Martelli1, Juan Antonio Ponce-Gomez2,3,4, Victor Alcocer-Barradas3,4, Samuel Romano-Feinholz2, Pilar Padilla-Quiroz5, Marcela Osuna Zazueta2,3, Luis Alberto Ortega-Porcayo1,2,3. Upward transtentorial herniation: A new role for endoscopic third ventriculostomy. 06-Jul-2021;12:334. Available from: https://surgicalneurologyint.com/surgicalint-articles/10944/
Abstract
Background: The placement of external ventricular drainage (EVD) to treat hydrocephalus secondary to a cerebellar stroke is controversial because it has been associated to upward transtentorial herniation (UTH). This case illustrates the effectiveness of endoscopic third ventriculostomy (ETV) after the ascending herniation has occurred.
Case Description: A 50-year-old man had a cerebellar stroke with hemorrhagic transformation, tonsillar herniation, and non-communicating obstructive hydrocephalus. Considering that the patient was anticoagulated and thrombocytopenic, an EVD was placed initially, followed by clinical deterioration and UTH. We performed a suboccipital craniectomy immediately after clinical worsening, but the patient did not show clinical or radiological improvement. On the 5th day, we did an ETV, which reverses the upward herniation and hydrocephalus. The patient improved progressively with good neurological recovery.
Conclusion: ETV is an effective and safe procedure for obstructive hydrocephalus. The successful resolution of the patient’s upward herniation after the ETV offers a potential option to treat UTH and advocates further research in this area.
Keywords: Cerebellar stroke, Endoscopic third ventriculostomy, Obstructive hydrocephalus, Upward transtentorial herniation
INTRODUCTION
The gold-standard treatment of a cerebellar stroke with acute neurological deterioration is a decompressive suboccipital craniectomy with dural expansion; it prevents brain herniation and is the preferred treatment even in the setting of associated hydrocephalus. External ventricular drainage (EVD) is recommended in obstructive hydrocephalus but should be followed or accompanied by decompressive craniectomy.[
UTH is clinically characterized by impaired consciousness and brainstem dysfunction.[
CASE REPORT
A 50-year-old male was admitted for a diagnostic evaluation of chest precordial pain, shortness of breath, nausea, diaphoresis, and abdominal pain. He had a past medical history of hypothyroidism treated with levothyroxine and atrial fibrillation treated with apixaban. Myocardial infarction was ruled out, and the EKG confirmed paroxysmal atrial fibrillation. On the 2nd day, the patient developed acute suboccipital headache, nausea, vomiting, dizziness, and dysmetria. Subsequently, he developed acute neurological deterioration. On examination, he was in coma, pupils were miotic, corneal, and nausea reflexes were present and symmetrical. Abnormal flexion was observed under pain stimuli. He had hyperreflexia and bilateral Babinski. Laboratory findings revealed thrombocytopenia and brain MRI showed a bilateral cerebellar ischemic stroke in PICA territory with hemorrhagic transformation, tonsillar herniation, and non-communicating obstructive hydrocephalus [
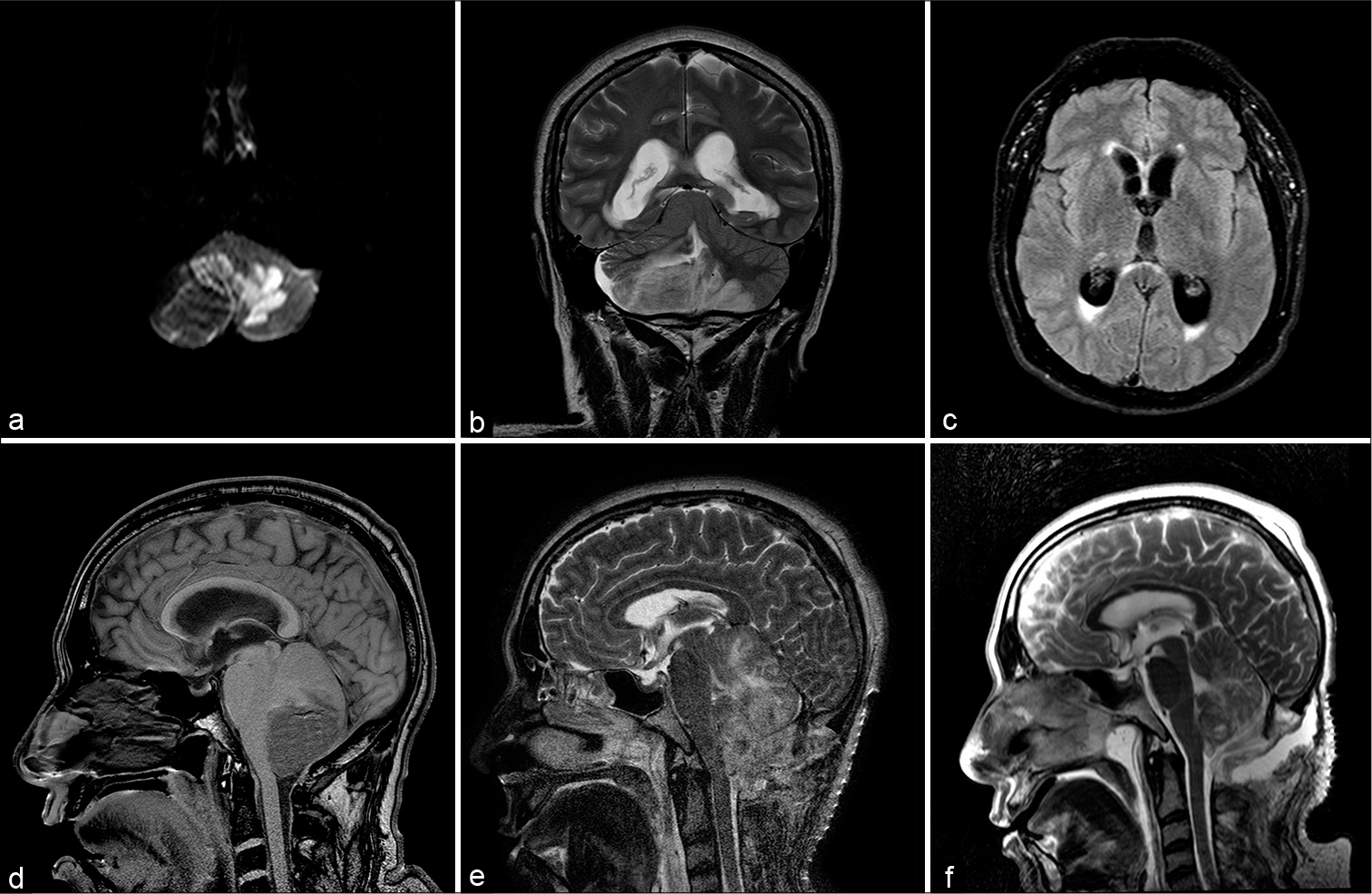
Figure 1:
PICA infarct with hemorrhagic transformation involving the posterior lobe of both cerebellar hemispheres seen on DWI (a), T2 (b) and the associated obstructive non-communicating hydrocephalus (c, d). After the EVD and the suboccipital craniectomy, the patient persisted with upward transtentorial herniation (e); notice the flattening of the quadrigeminal cistern, the “spinning top” appearance of the midbrain and the cerebral aqueduct occlusion. After the ETV, the upward transtentorial herniation was reversed (f) and the patient improved clinically.
We initially placed an EVD considering that the patient was anticoagulated and thrombocytopenic. The EVD was connected to ICP monitoring, which measured 35 mmHg. After draining 10 cc of CSF, the patient developed bradycardia, hypertension, and bilateral mydriasis, he was transferred back to the OR, and we performed a middle suboccipital craniectomy; the cerebellum was 5 mm deep from the dura and it did not swell immediately through the dural defect [
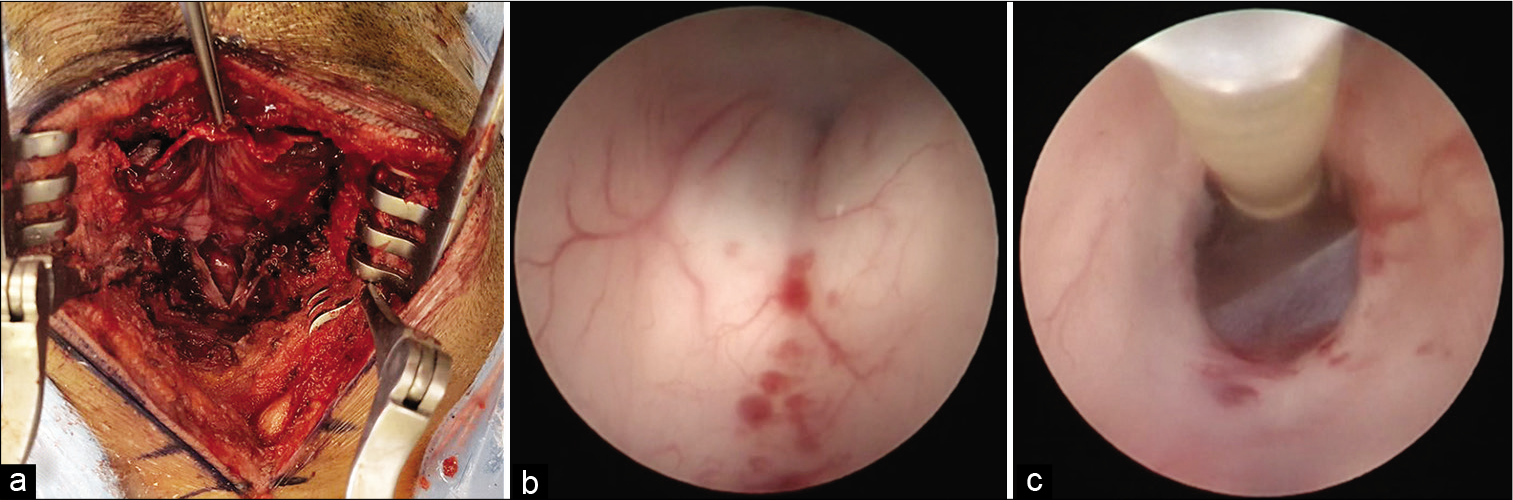
Figure 2:
Middle suboccipital craniectomy (a). Even though the MRI showed severe edema, the cerebellum was displaced dorsally away from the dural edge (a). During the endoscopic third ventriculostomy, we observed midbrain microhemorrhages and an active flow through the tuber cinereum fenestration (b and c).
DISCUSSION
There have been reported several UTH cases secondary to posterior fossa lesions. In 1920, Meyer gave the earliest descriptions of UTH,[
In our case, the patient was initially treated with an EVD to reduce ICP while the anticoagulant activity was reversed; however, the ventricular CSF drainage triggered an UTH because of a pressure gradient difference in the supratentorial and infratentorial compartments that resulted from a sudden pressure resistance decrease of the supratentorial space.[
The treatment of UTH has been proposed in the literature since 1947 when Ecker recommended a tentorial section and cerebellar aspiration to release the CSF and vein obstruction.[
The clinical diagnosis of UTH is characterized by intracranial hypertension syndrome, altered state of consciousness, loss of brainstem reflexes, and abnormal posturing.[
CONCLUSION
ETV is an effective and safe procedure for obstructive hydrocephalus. The successful resolution of the patient’s upward herniation after the ETV offers a potential option of treatment and advocates further research in this area.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
Thanks to Karla Ortega for proofreading this manuscript.
References
1. Adamson DC, Dimitrov DF, Bronec PR. Upward transtentorial herniation, hydrocephalus, and cerebellar edema in hypertensive encephalopathy. Neurologist. 2005. 11: 171-5
2. Amar AP. Controversies in the neurosurgical management of cerebellar hemorrhage and infarction. Neurosurg Focus. 2012. 32: E1
3. Arriada N, Sotelo J. Continuous-flow shunt for treatment of hydrocephalus due to lesions of the posterior fossa. J Neurosurg. 2004. 101: 762-6
4. Auer LM, Auer T, Sayama I. Indications for surgical treatment of cerebellar haemorrhage and infarction. Acta Neurochir (Wien). 1986. 79: 74-9
5. Braksick SA, Himes BT, Snyder K, van Gompel JJ, Fugate JE, Rabinstein AA. Ventriculostomy and risk of upward herniation in patients with obstructive hydrocephalus from posterior fossa mass lesions. Neurocrit Care. 2018. 28: 338-43
6. Cuneo RA, Caronna JJ, Pitts L, Townsend J, Winestock DP. Upward transtentorial herniation: Seven cases and a literature review. Arch Neurol. 1979. 36: 618-23
7. Dinsdale HB. Spontaneous hemorrhage in the posterior fossa. A study of primary cerebellar and pontine hemorrhages with observations on their pathogenesis. Arch Neurol. 1964. 10: 200-17
8. Ecker A. Upward transtentorial herniation of the brain stem and cerebellum due to tumor of the posterior fossa with special note on tumors of the acoustic nerve. J Neurosurg. 1948. 5: 51-61
9. El-Gaidi MA, El-Nasr AH, Eissa EM. Infratentorial complications following preresection CSF diversion in children with posterior fossa tumors. J Neurosurg Pediatr. 2015. 15: 4-11
10. Gurajala I, Brahmaprasad V, Rajesh A, Ramachandran G, Purohit AK. Reverse brain herniation following ventriculoperitoneal shunt. Indian J Anaesth. 2012. 56: 585-7
11. Heros RC. Cerebellar hemorrhage and infarction. Stroke. 1982. 13: 106-9
12. Knupling R, Fuchs EC, Stoltenburg G, Gerull G, Giesen M, Mrowinski D. Chronic and acute transtentorial herniation with tumours of the posterior cranial fossa. Neurochirurgia (Stuttg). 1979. 22: 9-17
13. Koenig MA. Cerebral edema and elevated intracranial pressure. Continuum (Minneap Minn). 2018. 24: 1588-602
14. Laine FJ, Shedden AI, Dunn MM, Ghatak NR. Acquired intracranial herniations: MR imaging findings. AJR Am J Roentgenol. 1995. 165: 967-73
15. LeBeau J.editors. L’oedème du Cerveau. Son Rôle Dans L’évolution de Tumeurs et des Abcès Intracrâniens. Thesis. Paris: J. Recht; 1938. p. 233
16. McKissock W, Richardson A, Walsh L. Spontaneous cerebellar hemorrhage: A study of 34 consecutive cases treated surgically. Brain. 1960. 83: 1-9
17. Meyer A. Herniation of the brain. Arch Neuropsych. 1920. 4: 387-400
18. Osborn AG, Heaston DK, Wing SD. Diagnosis of ascending transtentorial herniation by cranial computed tomography. AJR Am J Roentgenol. 1978. 130: 755-60
19. Rai R, Iwanaga J, Shokouhi G, Oskouian RJ, Tubbs RS. The tentorium cerebelli: A comprehensive review including its anatomy, embryology, and surgical techniques. Cureus. 2018. 10: e3079
20. Stevens RD, Shoykhet M, Cadena R. Emergency neurological life support: Intracranial hypertension and herniation. Neurocrit Care. 2015. 23: S76-82
21. Stone JL, Bailes JE, Hassan AN, Sindelar B, Patel V, Fino J. Brainstem monitoring in the neurocritical care unit: A rationale for real-time, automated neurophysiological monitoring. Neurocrit Care. 2017. 26: 143-56
22. Vindigni M, Tuniz F, Ius T, Cramaro A, Skrap M. Endoscopic third ventriculostomy in patients with secondary triventricular hydrocephalus from a haemorrhage or ischaemia in the posterior cranial fossa. Minim Invasive Neurosurg. 2010. 53: 106-11
23. Waidhauser E, Hamburger C, Marguth F. Neurosurgical management of cerebellar hemorrhage. Neurosurg Rev. 1990. 13: 211-7
24. Wijdicks EF, Sheth KN, Carter BS, Greer DM, Kasner SE, Kimberly WT. Recommendations for the management of cerebral and cerebellar infarction with swelling: A statement for healthcare professionals from the American heart association/ American stroke association. Stroke. 2014. 45: 1222-38
25. Yadav G, Sisodia R, Khuba S, Mishra L. Anesthetic management of a case of transtentorial upward herniation: An uncommon emergency situation. J Anaesthesiol Clin Pharmacol. 2012. 28: 413-5