- Department of Neurosurgery, Riverside University Health System, Riverside, California, United States.
- Department of Neurosurgery, University of Colorado School of Medicine, Aurora, Colorado, United States.
- Department of Neurosurgery, Kaiser Sunset Medical Center, Los Angeles, California, United States.
Correspondence Address:
Michael W. Kortz, Department of Neurosurgery, University of Colorado School of Medicine, Aurora, Colorado, United States.
DOI:10.25259/SNI_824_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Jacob Bernstein1, Samir Kashyap1, Michael W. Kortz2, Bishoy Zakhary1, Ariel Takayanagi1, Harjyot Toor1, Paras Savla1, Margaret R. Wacker1, Ajay Ananda3, Dan Miulli1. Utilization of epilepsy surgery in the United States: A study of the National Inpatient Sample investigating the roles of race, socioeconomic status, and insurance. 02-Nov-2021;12:546
How to cite this URL: Jacob Bernstein1, Samir Kashyap1, Michael W. Kortz2, Bishoy Zakhary1, Ariel Takayanagi1, Harjyot Toor1, Paras Savla1, Margaret R. Wacker1, Ajay Ananda3, Dan Miulli1. Utilization of epilepsy surgery in the United States: A study of the National Inpatient Sample investigating the roles of race, socioeconomic status, and insurance. 02-Nov-2021;12:546. Available from: https://surgicalneurologyint.com/surgicalint-articles/11210/
Abstract
Background: Epilepsy is estimated to affect 70 million people worldwide and is medically refractory in 30% of cases.
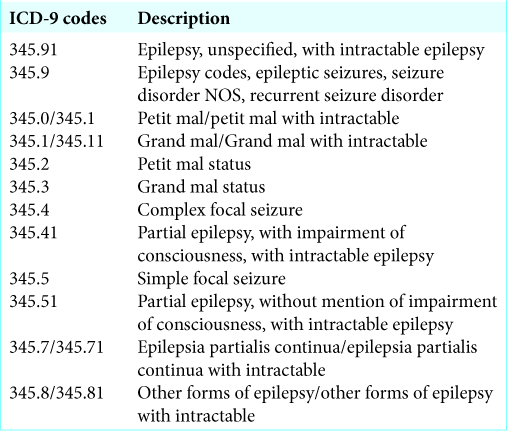
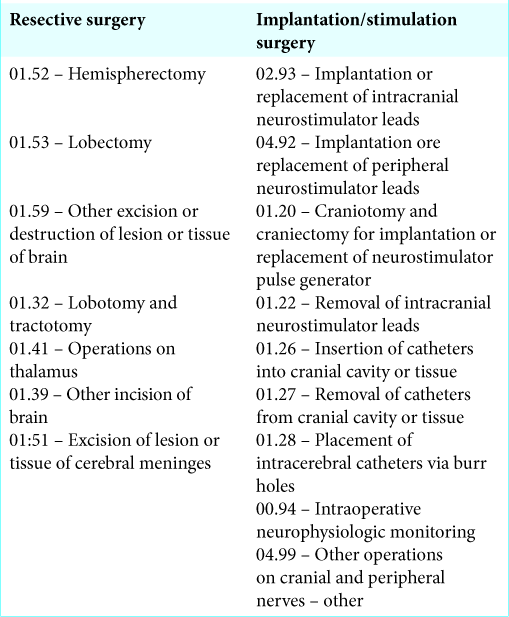
Methods: This is a retrospective cross-sectional study using a US database from 2012 to 2014 to identify patients aged ≥18 years admitted to the hospital with epilepsy as the primary diagnosis. The sampled population was weighted using Healthcare Cost and Utilization Project guidelines. Procedural ICD-9 codes were utilized to stratify the sampled population into two cohorts: resective surgery and implantation or stimulation procedure.
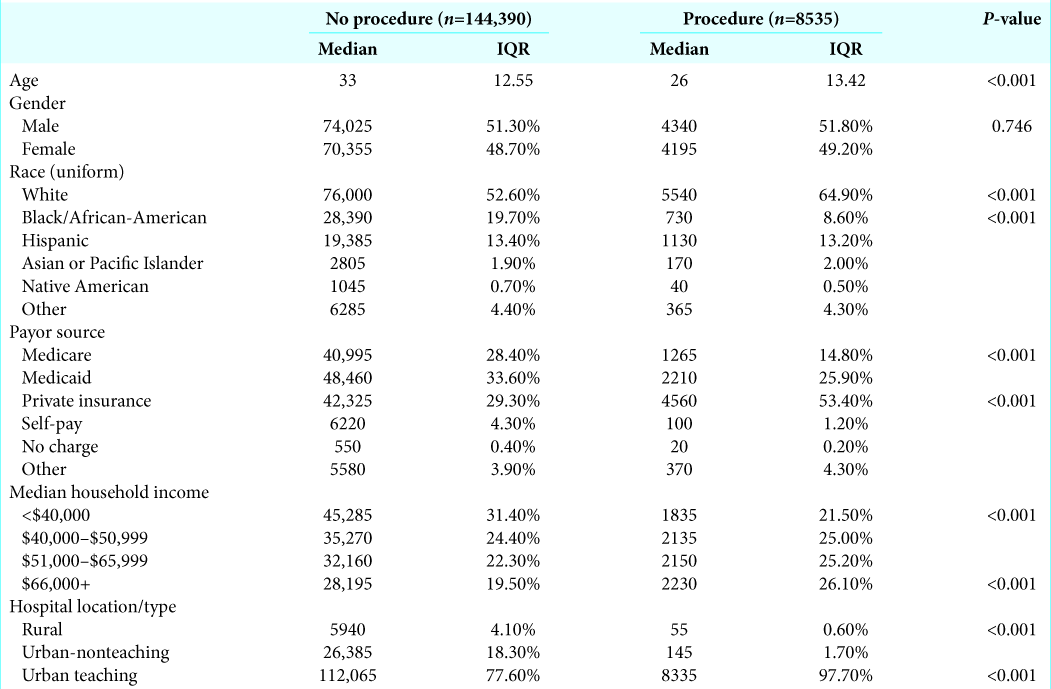
Results: Query of the database yielded 152,925 inpatients, of which 8535 patients underwent surgical intervention. The nonprocedural group consisted of 76,000 White patients (52.6%) and 28,390 Black patients (19.7%) while the procedural group comprised 5550 White patients (64%) and 730 Black patients (8.6%) (P P
Conclusion: We demonstrate an area of need and significant improvement at institutions that have the resources and capability to perform epilepsy surgery. The data show that institutions may not be performing enough epilepsy surgery as a result of racial and socioeconomic bias. Admissions for epilepsy continue to increase without a similar trend for epilepsy surgery despite its documented effectiveness. Race, socioeconomic status, and insurance all represent significant barriers in access to epilepsy surgery. The barriers can be remedied by improving referral patterns and implementing cost-effective measures to improve inpatient epilepsy services in rural and nonteaching hospitals.
Keywords: Deep brain stimulation, Epilepsy surgery, Functional neurosurgery, National database, Neuromodulation
INTRODUCTION
Epilepsy is estimated to affect 70 million people worldwide.[
Epilepsy surgery in children and adults continues to be underutilized in the US.[
Our study aims to characterize hospitalization and surgery rates from 2012 to 2014 in the United States using the national inpatient database and to further elucidate factors associated with utilization of epilepsy surgery as well as its associated complications.
MATERIALS AND METHODS
Study design and eligibility criteria
Institutional Review Board approval was obtained from Riverside University Health System for access to the National Inpatient Sample (NIS), Healthcare Cost and Utilization Project (HCUP), Agency for Healthcare Research and Quality.[
RESULTS
Query of the database yielded 152,925 inpatients with an epilepsy-DRG from 2012 to 2014. Of these patients, 8535 patients underwent surgical intervention. The median age of those in the procedural group was 26 years compared to 33 years in the nonprocedural group (P < 0.001). The number of epilepsy-DRG admissions increased by 9.2% as the number of epilepsy surgeries decreased by 1.4% during the 3-year study period. There was a significant racial difference in the demographics of nonprocedural versus procedural groups. The nonprocedural group consisted of 76,000 White patients (5.6%) and 28,390 Black patients (19.7%) while the procedural group comprised 5550 White patients (64%) and 730 Black patients (8.6%) (P <0.001). There were no statistically significant differences between any other racial demographic between the two groups [
There were no significant differences in comorbidities or complications between the resective surgery group and the implantation or stimulation surgery group. There were higher costs (median costs $164,286 vs. $108,782, P < 0.001) and greater hospital length of stay with the implantation or stimulation surgery group (9 vs. 4 days, <0.001). Resective surgeries saw a 7.4% increase from 2012 to 2014 (1490–1600) while implantation or stimulation surgeries saw a 10.9% decrease from 2012 to 2014 (1370–1220).
DISCUSSION
Medically refractory epilepsy is a condition unfamiliar to many patients and clinicians. In fact, one survey found nearly 49% of one group of neurologists were unfamiliar with the definition of medically refractory epilepsy.[
Racial factors in utilization of epilepsy surgery
Our findings are in line with previous publications discussing racial disparities in access to epilepsy surgery. In a single institution retrospective cohort, Burneo et al. found that African-Americans were 60% less likely to undergo epilepsy surgery than non-Hispanic Whites.[
Socioeconomic factors in utilization of epilepsy surgery
In our review, median income represented the second most significant barrier to receiving epilepsy surgery. Those in the lowest income quartile were the only subset of patients to have a lower percentage of patients to undergo a surgical procedure (31.4% vs. 21.5%). Recent studies demonstrate similar findings. In a retrospective review of 284 children receiving epilepsy surgery, those in the lowest income quintile had the longest time to receive epilepsy surgery and had significantly lower odds of improvement in seizure frequency.[
Geographic barriers to epilepsy surgery
Patients residing in rural locations also underwent significantly fewer epilepsy procedures. This is likely because epilepsy providers are primarily located in urban centers and visiting these centers are not feasible for many patients.[
Potential solutions
The above factors each play a unique role that affects access to epilepsy surgery. It is essential that primary care providers and neurologists be educated on the efficacy of epilepsy surgery and early referral to epilepsy centers is encouraged.[
Schlitz et al. highlights the possibility of minimally-invasive epilepsy surgery for patients with disadvantaged patients but is not convinced that access will be broadened beyond large academic centers in the near future. They argue that behavioral and social strategies will be more effective to address the surgical access gap for medically refractory epilepsy.[
In addition, epilepsy programs must make efforts to alleviate the financial burden on patient families. The multiple encounters required for preoperative planning can be a deterrent for families whose financial security may be threatened by taking time off work. Jackson et al. suggested having an epilepsy program coordinator schedule all of the patient’s preoperative studies and appointments together to prevent delays to surgery and to ease the family’s burden.[
Remote EEG software provides a technological solution that can eliminate many existing barriers for patients with this condition. Multiple studies in Guinea found that a smartphone-based technology – Smartphone Brain Scanner – and tablet-based software provided the ability for low-income areas to receive specialist input using remote technologies and crowdsourcing.[
Limitations
Retrospective reviews inherently have their own limitations on how long and what variables were collected in addition to selection bias. Having to search a database based on various diagnostic and procedure codes may leave out a significant number of patients due to incorrect coding. The sample data come from the years 2012 to 2014 which may not accurately reflect current trends in epilepsy surgery, however, the NIS only has data through 2018 and the largest database study previously performed on epilepsy surgery reported data through 2008.[
CONCLUSION
Our review of the NIS data from 2012 to 2014 and epilepsy literature demonstrate an area of need and significant improvement at institutions that have the resources and capability to perform epilepsy surgery. Potential epilepsy surgery patients can be up to 30% in a hospital catchment area. The data show that institutions are not performing enough epilepsy surgery because of racial and socioeconomic bias. Admissions for epilepsy continue to increase without an increase in epilepsy surgery despite its documented effectiveness. Race, socioeconomic status, and insurance all represent significant barriers in access to epilepsy surgery. The barriers can be remedied by improving referral patterns and implementing cost-effective measures to improve inpatient epilepsy services in rural and nonteaching hospitals.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Alluri RK, Leland H, Heckmann N. Surgical research using national databases. Ann Transl Med. 2016. 4: 393
2. Benbadis SR, Heriaud L, Tatum WO, Vale FL. Epilepsy surgery, delays and referral patterns-are all your epilepsy patients controlled?. Seizure. 2003. 12: 167-70
3. Burneo JG, Black L, Knowlton RC, Faught E, Morawetz R, Kuzniecky RI. Racial disparities in the use of surgical treatment for intractable temporal lobe epilepsy. Neurology. 2005. 64: 50-4
4. Catchpool M, Dalziel K, Mahardya RT, Harvey AS. Cost-effectiveness of epileptic surgery compared with medical treatment in children with drug-resistant epilepsy. Epilepsy Behav. 2019. 97: 253-9
5. Chan AK, McGovern RA, Brown LT, Sheehy JP, Zacharia BE, Mikell CB. Disparities in access to deep brain stimulation surgery for Parkinson disease: Interaction between African American race and Medicaid use. JAMA Neurol. 2014. 71: 291-9
6. Engel J. A greater role for surgical treatment of epilepsy: Why and when?. Epilepsy Curr. 2003. 3: 37-40
7. Englot DJ, Ouyang D, Garcia PA, Barbaro NM, Chang EF. Epilepsy surgery trends in the United States, 1990-2008. Neurology. 2012. 78: 1200-6
8. Erba G, Moja L, Beghi E, Messina P, Pupillo E. Barriers toward epilepsy surgery. A survey among practicing neurologists. Epilepsia. 2012. 53: 35-43
9. Hakimi AS, Spanaki MV, Schuh LA, Smith BJ, Schultz L. A survey of neurologists’ views on epilepsy surgery and medically refractory epilepsy. Epilepsy Behav. 2008. 13: 96-101
10. Haneef Z, Stern J, Dewar S, Engel J. Referral pattern for epilepsy surgery after evidence-based recommendations: A retrospective study. Neurology. 2010. 75: 699-704
11. Jackson HN, Gadgil N, Pan IW, Clarke DF, Wagner KM, Cronkite CA. Sociodemographic factors in pediatric epilepsy surgery. Pediatr Neurol. 2020. 107: 71-6
12. Jetté N, Sander JW, Keezer MR. Surgical treatment for epilepsy: The potential gap between evidence and practice. Lancet Neurol. 2016. 15: 982-94
13. McClelland S, Guo H, Okuyemi KS. Racial disparities in the surgical management of intractable temporal lobe epilepsy in the United States: A population-based analysis. Arch Neurol. 2010. 67: 577-83
14. Nathan CL, Gutierrez C. FACETS of health disparities in epilepsy surgery and gaps that need to be addressed. Neurol Clin Pract. 2018. 8: 340-5
15. Owens S, Sirven JI, Shafer PO, Fishman J, Wild I, Findley M. Innovative approaches reaching underserved and rural communities to improve epilepsy care: A review of the methodology of the connectors project. Epilepsy Behav. 2019. 90: 273-83
16. Pestana Knight EM, Schiltz NK, Bakaki PM, Koroukian SM, Lhatoo SD, Kaiboriboon K. Increasing utilization of pediatric epilepsy surgery in the United States between 1997 and 2009. Epilepsia. 2015. 56: 375-81
17. Peterson K, LaRoche S, Cummings T, Woodard V, Moise AM, Clary H. Addressing the epilepsy surgery gap: Impact of community/tertiary epilepsy center collaboration. Epilepsy Behav Rep. 2020. 14: 100398
18. Pisu M, Richman J, Piper K, Martin R, Funkhouser E, Dai C. Quality of antiepileptic treatment among older medicare beneficiaries with epilepsy: A retrospective claims data analysis. Med Care. 2017. 55: 677-83
19. Roberts JI, Hrazdil C, Wiebe S, Sauro K, Vautour M, Wiebe N. Neurologists’ knowledge of and attitudes toward epilepsy surgery: A national survey. Neurology. 2015. 84: 159-66
20. Rubinger L, Chan C, Andrade D, Go C, Smith ML, Snead OC. Socioeconomic status influences time to surgery and surgical outcome in pediatric epilepsy surgery. Epilepsy Behav. 2016. 55: 133-8
21. Samanta D, Ostendorf AP, Willis E, Singh R, Gedela S, Arya R. Underutilization of epilepsy surgery: Part I: A scoping review of barriers. Epilepsy Behav. 2021. 117: 107837
22. Samanta D, Singh R, Gedela S, Scott Perry M, Arya R. Underutilization of epilepsy surgery: Part II: Strategies to overcome barriers. Epilepsy Behav. 2021. 117: 107853
23. Sánchez Fernández I, Stephen C, Loddenkemper T. Disparities in epilepsy surgery in the United States of America. J Neurol. 2017. 264: 1735-45
24. Schiltz NK, Fernandez-Baca Vaca G. Epidemiologist’s view: Addressing the epilepsy surgery treatment gap with minimally-invasive techniques. Epilepsy Res. 2018. 142: 179-81
25. Schiltz NK, Koroukian SM, Lhatoo SD, Kaiboriboon K. Temporal trends in pre-surgical evaluations and epilepsy surgery in the U.S. from 1998 to 2009. Epilepsy Res. 2013. 103: 270-8
26. Schiltz NK, Koroukian SM, Singer ME, Love TE, Kaiboriboon K. Disparities in access to specialized epilepsy care. Epilepsy Res. 2013. 107: 172-80
27. Shone LP, Dick AW, Brach C, Kimminau KS, LaClair BJ, Shenkman EA. The role of race and ethnicity in the state children’s health insurance program (SCHIP) in four states: Are there baseline disparities, and what do they mean for SCHIP?. Pediatrics. 2003. 112: e521
28. Sokolov E, Abdoul Bachir DH, Sakadi F, Williams J, Vogel AC, Schaekermann M. Tablet-based electroencephalography diagnostics for patients with epilepsy in the West African republic of guinea. Eur J Neurol. 2020. 27: 1570-7
29. Sperling MR. Temporal lobectomy for refractory epilepsy. JAMA. 1996. 276: 470
30. Wheeler SM, Bryant AS. Racial and ethnic disparities in health and health care. Obstet Gynecol Clin North Am. 2017. 44: 1-11
31. Wiebe S. Epilepsy: Does access to care influence the use of epilepsy surgery?. Nat Rev Neurol. 2016. 12: 133-4
32. Williams JA, Cisse FA, Schaekermann M, Sakadi F, Tassiou NR, Hotan GC. Smartphone EEG and remote online interpretation for children with epilepsy in the Republic of Guinea: Quality, characteristics, and practice implications. Seizure. 2019. 71: 93-9