- Department of Orthopaedics, Khoula Hospital, Muscat, Oman.
DOI:10.25259/SNI_306_2019
Copyright: © 2019 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Sam Supreeth, Khalifa Al Ghafri. Ventral holocord spinal epidural abscess managed surgically in a critical setting. 13-Dec-2019;10:248
How to cite this URL: Sam Supreeth, Khalifa Al Ghafri. Ventral holocord spinal epidural abscess managed surgically in a critical setting. 13-Dec-2019;10:248. Available from: https://surgicalneurologyint.com/surgicalint-articles/9798/
Abstract
Background: Extensive epidural abscess is an uncommon entity which is increasing in the aging population. Its prevalence is also greater among those with diabetes mellitus and in those who are immunocompromised. Here, a 59-year-old female presented with a spinal epidural abscess (SEA) warranting operative intervention.
Case Description: A 59-year-old female with a history of diabetes and hypertension, presented with the acute onset of a high-grade fever, generalized back pain, and an evolving quadriparesis. Preliminary laboratory studies revealed elevated inflammatory markers. The magnetic resonance scan showed a ventral epidural abscess extending from C1-2 to the L5 level. She underwent urgent surgical decompression using a Nelaton catheter placed through an L4-L5 hemilaminectomy and threaded cephalad (40 cm); this resulted in a complete recovery.
Conclusion: This case study underscores a unique way of managing an anterior holospinal SEA extending from the C1-2 through the L5 spinal levels.
Keywords: Cervicolumbar, Critical, Hemilaminectomy, Holocord, Nelaton, Spinal epidural abscess, Ventral
INTRODUCTION
Spinal epidural abscess (SEA) occurs in approximately 0.2–2 case/10,000 admissions.[
Treatment of SEA is a two-staged process that includes (1) antibiotics for treating the systemic manifestations versus (2) surgery with additional appropriate antibiotic therapy. Here, we report the case of a ventrally located SEA extending from the C1-2 through L5 level treated successfully utilizing a minimally invasive catheter technique (Nelaton catheter: 40 cm long) introduced through a hemilaminectomy at the L4-L5 level.
CASE DESCRIPTION
A 59-year-old female with diabetes and hypertension presented with low back pain, electric shock- like sensations, and a progressive quadriparesis of 10 days duration. For the past 2 days, she had a high-grade fever with chills. Her neurological examination revealed diffuse hyperreflexia 3–4+ accompanied by bilateral Hoffman’s sign, clonus, and Babinski responses.
Laboratory studies
Preliminary laboratory tests revealed markedly elevated C-reactive protein (CRP: 447 mg/l), a high erythrocytes sedimentation rate (ESR: 119 mm/h), an increased white blood cell count (WBC: 25 × 103/µl), and abnormal serum urea level (11.69 mmol/l).
Radiological studies
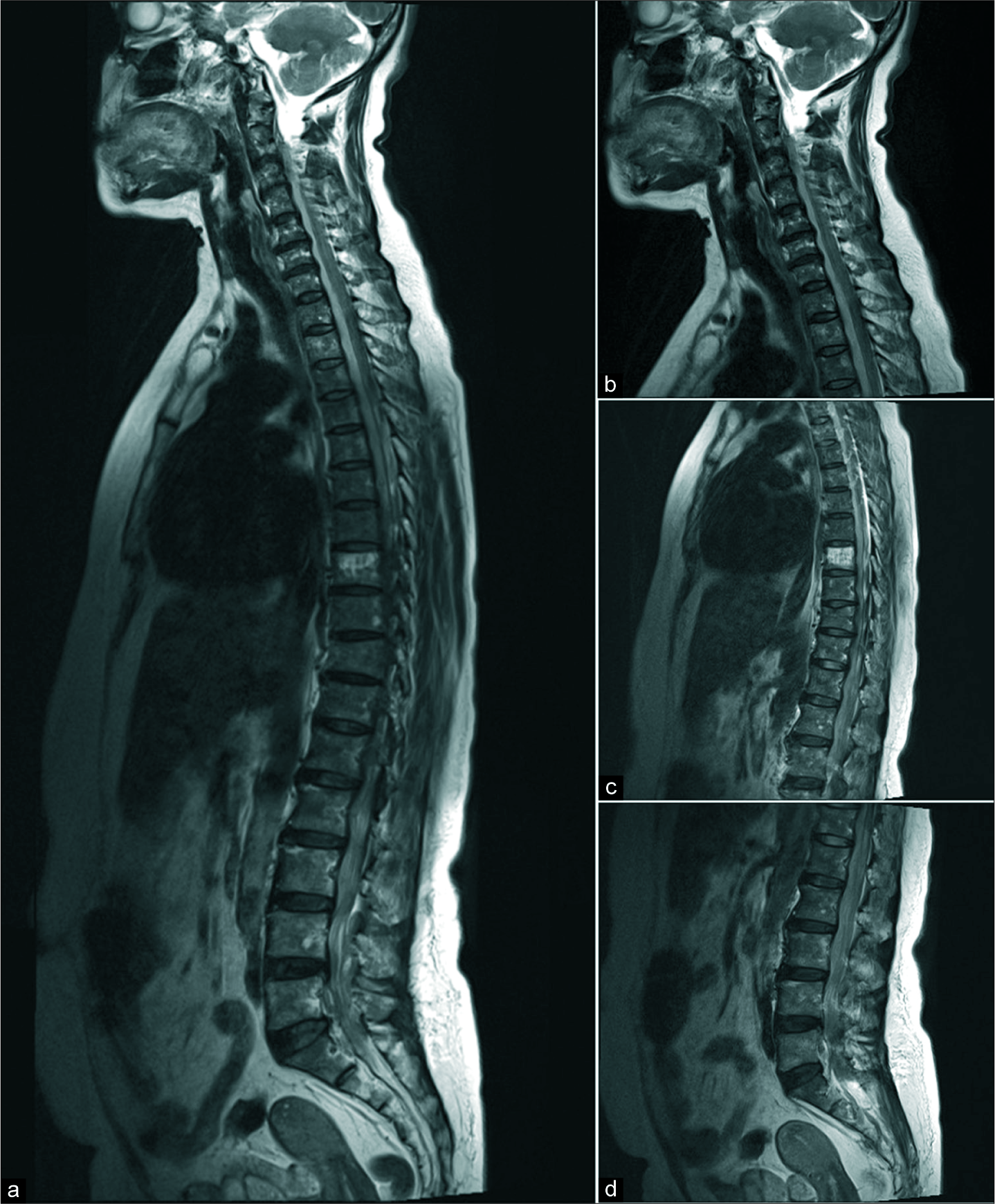
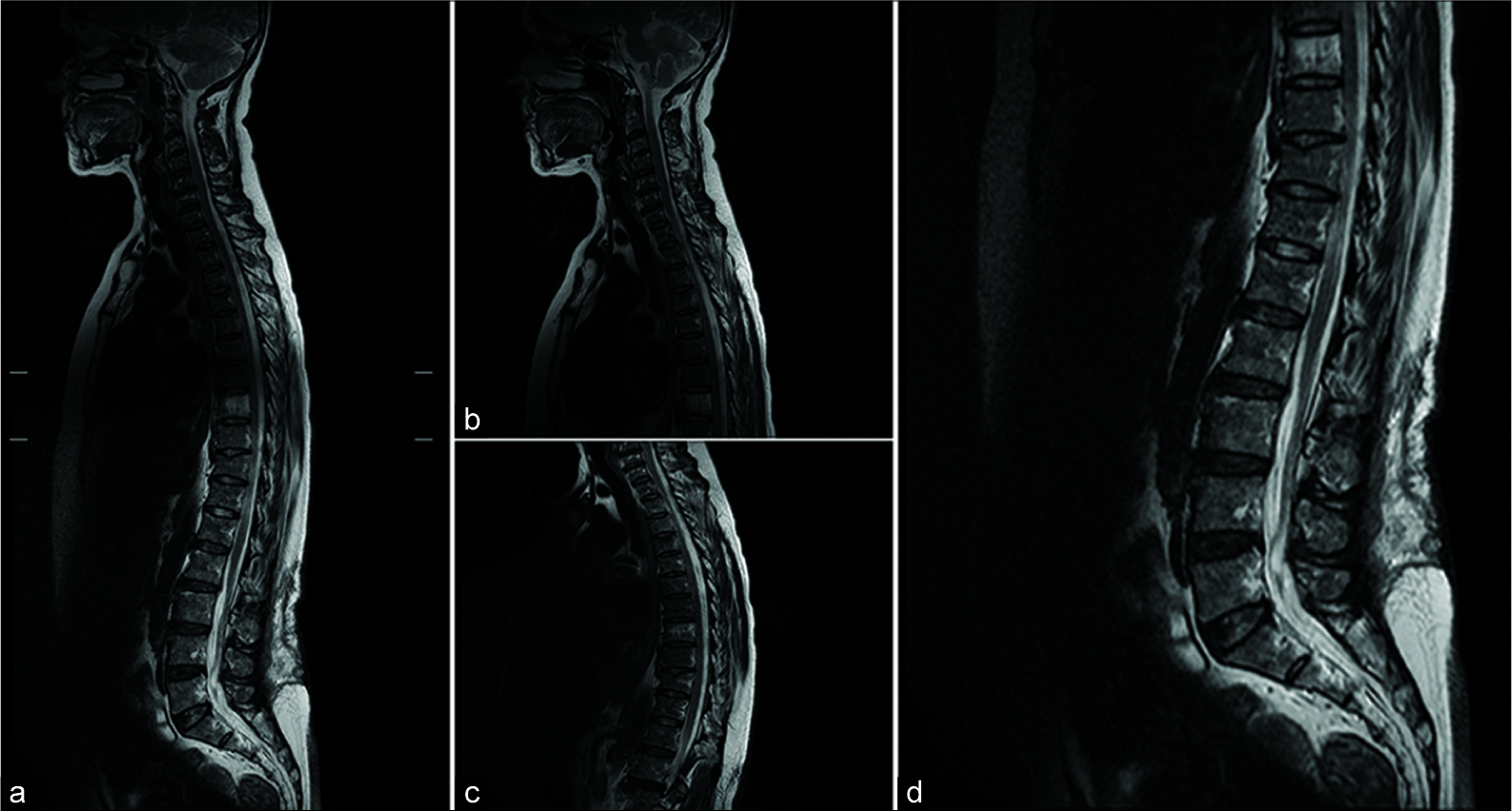
Magnetic resonance imaging (MRI) [
Treatment of SEA
At surgery, the right paraspinal abscess at the L4-5 level was filled with frank pus and was appropriately drained. Next, the patient underwent L4-5 right side hemilaminectomy allowing for drainage of pus from the ventral spinal canal; tilting the operating table (reverse Trendelenburg) further facilitated such drainage from more cephalad levels. Next, a Nelaton catheter (size 14 gauge and 40 cm long) was gently and gradually guided cephalad along the ventral epidural space. This allowed for further washout of pus and accompanying infectious debris. Once instilled irrigation drained clear fluid, the catheter was then withdrawn, and the wound was closed. Over the next 4 postoperative months, the patient improved dramatically as did the inflammatory markers.
Antibiotic regimen
Intraoperative cultures of the ventral pus and blood culture yielded Streptococcus pneumoniae. It was appropriately treated with ceftriaxone (2 g once a day) and vancomycin (1 g twice a day) for 6 weeks intravenously, followed by oral cefuroxime (500 mg twice a day) for an additional 6 weeks on discharge. An incidental finding was an infection involving the right knee requiring arthroscopic washout at both 1 week and 3 weeks after the spine surgery.
Postoperative course
The 1-month postoperative MRI [
DISCUSSION
Location of SEA
SEA most typically appear in the lumbar level (48%) followed by thoracic (31%) and then cervical (21%) levels.[
Five similar holocord SEAs
Five similar cases of holocord SEA have previously been reported. One study included three pockets of SEA located at C7-T5 ventrally, and T5-11, and L1-5 dorsally.[
Operative techniques for holocord SEA
Different techniques for treating holocord SEA are described ranging from; open decompression/late closure, multilevel decompression, limited decompression (one-level laminectomy or hemilaminectomy with Fogarty embolectomy catheter use), percutaneous CT-guided needle aspiration, and limited laminectomies (e.g., using a silicon catheter epidurally).[
CONCLUSION
In this case, we utilized a Nelaton catheter (size 14; 40 cm long) introduced through a right-sided L4-L5 hemilaminectomy to successfully drain a holocord ventral SEA extending from the C1-C2 through the L5.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms.
Financial support and sponsorship
Nil.
Conflicts of interest
Acknowledgement to Rahesh Nair for his support.
References
1. Baker AS, Ojemann RG, Swartz MN, Richardson EP. Spinal epidural abscess. N Engl J Med. 1975. 293: 463-8
2. Bluman EM, Palumbo MA, Lucas PR. Spinal epidural abscess in adults. J Am Acad Orthop Surg. 2004. 12: 155-63
3. Heusner AP. Nontuberculous spinal epidural infections. N Engl J Med. 1948. 239: 845-54
4. Lu CH, Chang WN, Lui CC, Lee PY, Chang HW. Adult spinal epidural abscess: Clinical features and prognostic factors. Clin Neurol Neurosurg. 2002. 104: 306-10
5. Lyu RK, Chen CJ, Tang LM, Chen ST. Spinal epidural abscess successfully treated with percutaneous, computed tomography-guided, needle aspiration and parenteral antibiotic therapy: Case report and review of the literature. Neurosurgery. 2002. 51: 509-12
6. Miftode E, Luca V, Mihalache D, Leca D, Stefanidis E, Anuţa C. Spinal epidural abscess. Rev Med Chir Soc Med Nat Iasi. 2001. 105: 778-84
7. Panagiotopoulos V, Konstantinou D, Solomou E, Panagiotopoulos E, Marangos M, Maraziotis T. Extended cervicolumbar spinal epidural abscess associated with paraparesis successfully decompressed using a minimally invasive technique. Spine (Phila Pa 1976). 2004. 29: E300-3
8. Pradilla G, Ardila GP, Hsu W, Rigamonti D. Epidural abscesses of the CNS. Lancet Neurol. 2009. 8: 292-300
9. Reihsaus E, Waldbaur H, Seeling W. Spinal epidural abscess: A meta-analysis of 915 patients. Neurosurg Rev. 2000. 23: 175-204
10. Riaz S, Mahmood JK. Extensive spinal epidural abscess. J Ayub Med Coll Abbottabad. 2007. 19: 64-7
11. Schultz KD, Comey CH, Haid RW. Technical note. Pyogenic spinal epidural abscess: A minimally invasive technique for multisegmental decompression. J Spinal Disord. 2001. 14: 546-9
12. Song KJ, Choi BW, Kim GH, Choi BR. Unusual spinal epidural abscess without predisposing factors treated using a minimally invasive technique. J Korean Orthop Assoc. 2009. 44: 680-5
13. Tahir MZ, Hassan RU, Enam SA. Management of an extensive spinal epidural abscess from C-1 to the sacrum. Case report. J Neurosurg Spine. 2010. 13: 780-3
14. Verner EF, Musher DM. Spinal epidural abscess. Med Clin North Am. 1985. 69: 375-84