- Department of Neurosurgery, Federal University of Espirito Santo, Vitória, Brazil
- Department of Medicine, School of Science of Santa Casa de Misericórdia de Vitória (EMESCAM), Vitória, Brazil
- Department of Medicine, Fatima Memorial College of Medicine and Dentistry (FMHCMD), Lahore, Pakistan
Correspondence Address:
Walter Fagundes, Department of Neurosurgery, Federal University of Espirito Santo, Vitoria, Brazil.
DOI:10.25259/SNI_702_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Walter Fagundes1, Isabella Rabelo Faria1, Rodrigo Martins Pereira1, Stefano Aliprandi Sacht1, Izabela Orlandi Môro2, Rabbia Jabbar3. Vestigial human tail and occult spinal dysraphism: A case report. 06-Dec-2024;15:452
How to cite this URL: Walter Fagundes1, Isabella Rabelo Faria1, Rodrigo Martins Pereira1, Stefano Aliprandi Sacht1, Izabela Orlandi Môro2, Rabbia Jabbar3. Vestigial human tail and occult spinal dysraphism: A case report. 06-Dec-2024;15:452. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13269
Abstract
Background: The presence of a human tail is a rare condition resulting from an embryonic remnant that fits the definition of a caudal appendage. It may be a vestigial (true) or a pseudotail. Both may be considered markers of underlying intraspinal abnormalities.
Case Description: The present case documents a 5-year-old girl with a caudal appendage in the lumbar region, with a previously normal neurological examination. Spinal magnetic resonance imaging (MRI) showed the presence of occult spinal dysraphism associated with a cutaneous appendage with lipomatous content. We performed microsurgical treatment to excise the lesion and explore the occult spinal dysraphism. A histopathological examination revealed mature adipose tissue with blood vessels and nerve fibers and no bone or cartilage tissue.
Conclusion: The presence of a tail-like appendage in the lumbosacral region must alert to the possibility of underlying occult spinal dysraphism. Preoperative assessment must include a complete neurological examination and a detailed MRI evaluation.
Keywords: Caudal appendage, Human tail, Spinal dysraphism, Vestigial
INTRODUCTION
The human tail has been classified as either a true (persistent vestigial) tail or a pseudotail.[
CASE REPORT
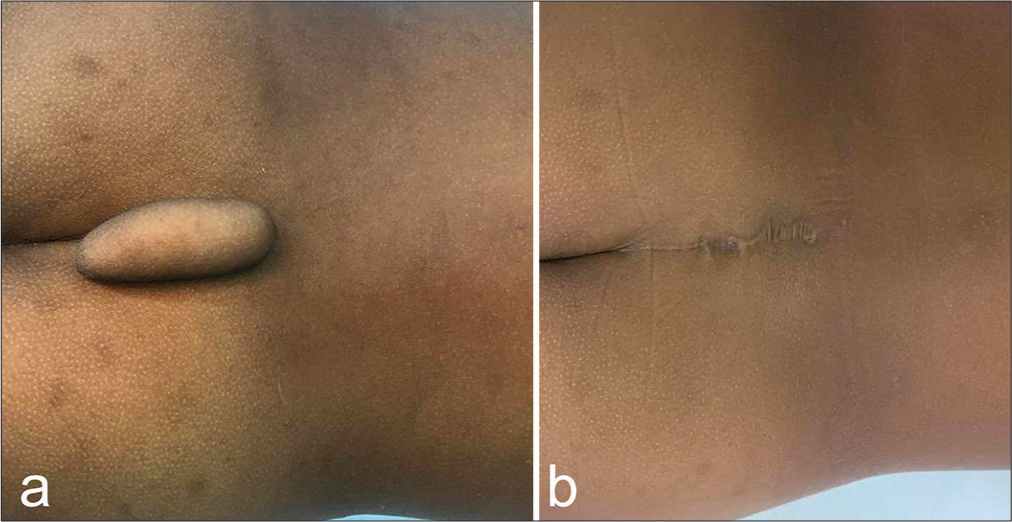
A 5-year-old girl was admitted with a tail-like structure that had been present since birth. In the midline of the lumbosacral region, a skin-covered, soft, non-tender, and nonfluctuating appendage, 6.5 cm in length and 2 cm in diameter, appeared similar to a human tail [
DISCUSSION
The incidence of true human tails is observed to be twice as high in male patients as in female patients. Consequently, reports of this condition in females are relatively rare, making our case involving a girl particularly noteworthy.
The human tail is a rare vestigial appendage observed in the midline or just off the midline of the lumbar or sacrococcygeal region.[
Three cases of spinal dysraphism with tail-like cutaneous structures have been described,[
The distinguishing features between true tails and pseudotails have been described, providing a basis for differentiation.[
Wilkinson and Boylan[
The human tail has been characterized as a benign congenital anomaly.[
It is important to evaluate the presence of a tethered cord on MRI, which, in the present case, was not observed in any of the MRI sequences. In addition, it is important to remember that the absence of a fibrous or dermal tract attached to the dura does not rule out an abnormality of the filum terminale.
The present case involves a female child with a vestigial human tail, occult spinal dysraphism, and a normal neurological examination. Therefore, in addition to a thorough clinical examination, an MRI should be performed in every case of a human tail to assess for the possibility of spinal dysraphism before the surgical treatment for excision.
CONCLUSION
This case underscores the importance of early identification and comprehensive evaluation of caudal appendages in children. A vestigial tail may signal underlying conditions such as occult spinal dysraphism, highlighting the need for a detailed neurological examination and MRI to identify associated anomalies. Surgical management should address both esthetic and neurological considerations. Thorough assessment and proactive intervention are essential to achieve favorable outcomes in patients with these rare congenital anomalies.
Disclosures
The authors report no conflicts of interest concerning the materials or methods used in this study or the findings specified in this paper.
Ethical approval
The Institutional Review Board approval is obtained by the Ethics Committee of the Health Science Center at the Federal University of Espírito Santo under the number 39194620.0.0000.5060.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Akhil P, Ashutosh N, Fais F, Shashank M, Sanjay P, Singhal BM. True vestigial tail with lumbosacral meningomyelocele: A rare case report. Br J Neurosurg. 2010. 24: 597-9
2. Belzberg AJ, Myles ST, Trevenen CL. The human tail and spinal dysraphism. J Pediatr Surg. 1991. 26: 1243-5
3. Chauhan SP, Gopal NN, Jain M, Gupta A. Human tail with spina bifida. Br J Neurosurg. 2009. 23: 634-5
4. Cai C, Shi O, Shen C. Surgical treatment of a patient with human tail and multiple abnormalities of the spinal cord and column. Adv Orthop. 2011. 1: 153797
5. Dao AH, Netsky MG. Human tails and pseudotails. Hum Pathol. 1984. 15: 449-53
6. Islam MN, Adhikari SB, Alam MM, Dilshad Munmun UH. Experience with human tail and its outcome. Afr J Paediatr Surg. 2021. 18: 43-6
7. Kabra NS, Srinivasan G, Udani RH. True tail in a neonate. Indian Pediatr. 1999. 36: 712-3
8. Ledley FD. Evolution and the human tail: A case report. N Engl J Med. 1982. 306: 1212-5
9. Liaqat N, Sandhu AI, Khan FA, Ehmed E, Dar SH. Child with a tail. APSP J Case Rep. 2013. 4: 42
10. Lu FL, Wang PJ, Teng RJ, Yau KI. The human tail. Pediatr Neurol. 1998. 19: 230-3
11. Mukhopadhyay B, Shukla RM, Mukhopadhyay M, Mandal KC, Haldar P, Benare A. Spectrum of human tails: A report of six cases. J Indian Assoc Pediatr Surg. 2012. 17: 23-5
12. Pillai MK, Nair ST. A True human tail in a neonate: Case report and literature review. Sultan Qaboos Univ Med J. 2017. 17: e109-11
13. Singh DK, Kumar B, Sinha VD, Bagaria HR. The human tail: Rare lesion with occult spinal dysraphism--a case report. J Pediatr Surg. 2008. 43: e41-3
14. Spiegelmann R, Schinder E, Mintz M, Blakstein A. The human tail: A benign stigma. Case report. J Neurosurg. 1985. 63: 461-2
15. Tubbs RS, Malefant J, Loukas M, Jerry Oakes W, Oskouian RJ, Fries FN. Enigmatic human tails: A review of their history, embryology, classification, and clinical manifestations. Clin Anat. 2016. 29: 430-8
16. Wilkinson CC, Boylan AJ. Proposed caudal appendage classification system; spinal cord tethering associated with sacrococcygeal eversion. Childs Nerv Syst. 2017. 33: 69-89