- Department of Neurosurgery, Kurume University School of Medicine, Kurume City, Japan.
Correspondence Address:
Yusuke Otsu, Department of Neurosurgery, Kurume University School of Medicine, Kurume City, Japan.
DOI:10.25259/SNI_450_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Yusuke Otsu, Satoru Komaki, Nobuyuki Takeshige, Kiyohiko Sakata, Motohiro Morioka. Visual-evoked potential predicts the efficacy of the optical canal decompression for traumatic optic nerve neuropathy showing blindness: A case report. 14-Jul-2023;14:245
How to cite this URL: Yusuke Otsu, Satoru Komaki, Nobuyuki Takeshige, Kiyohiko Sakata, Motohiro Morioka. Visual-evoked potential predicts the efficacy of the optical canal decompression for traumatic optic nerve neuropathy showing blindness: A case report. 14-Jul-2023;14:245. Available from: https://surgicalneurologyint.com/surgicalint-articles/12428/
Abstract
Background: The indication for surgical optic canal decompression (OCD) for traumatic optic neuropathy (TON) remains controversial because there is no reliable predictor of a good outcome. We report the case of a blind patient with TON whose remaining visual-evoked potential (VEP) suggested recovery potential of the injured optic nerve after OCD.
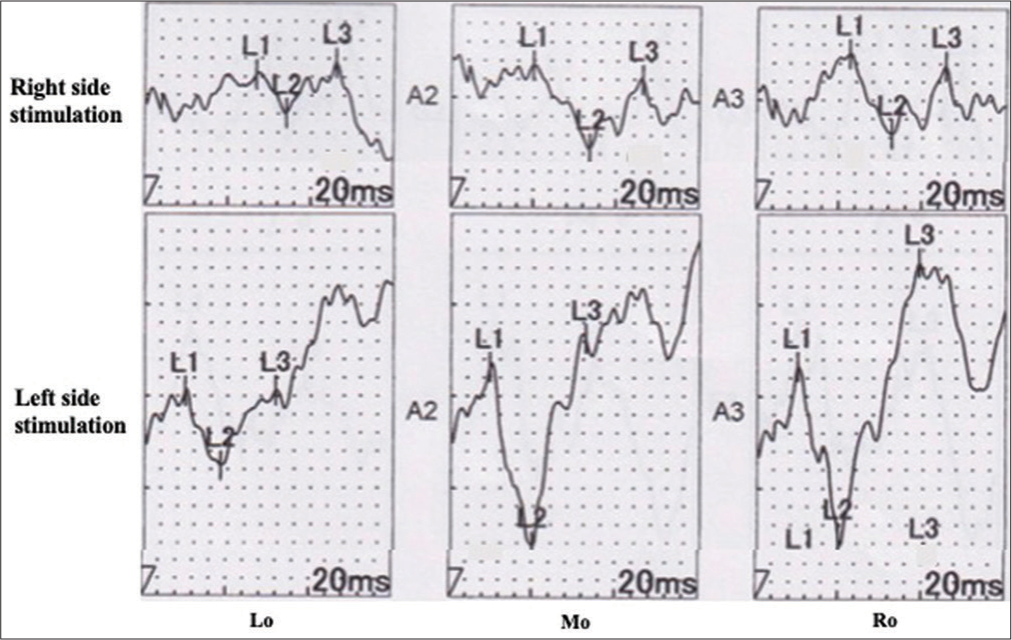
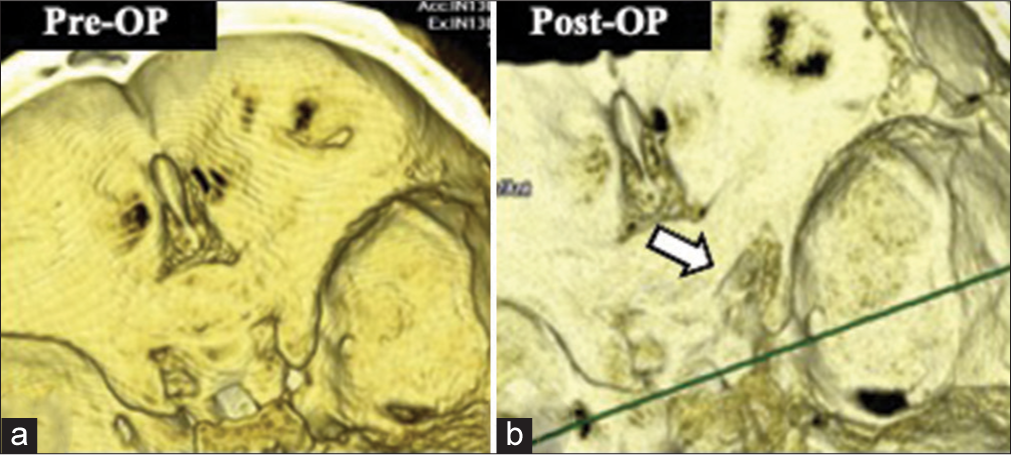
Case Description: A 48-year-old man had fallen from a height of 7 m, striking his head. He immediately complained of right-eye blindness. He had no light perception and the direct light reflex disappeared from the right pupil, although there was no fracture or traumatic lesion on computed tomography and magnetic resonance imaging. Because the amplitude of the VEP with the right eye stimulation remained unchanged, we performed the right OCD. During surgical OCD, the amplitude and latency of VEP began to improve. Finally, the visual field improved in almost all directions, and eyesight improved to 0.2.
Conclusion: The retained VEP activity in TON may suggest the recovery potential of the injured optic nerve, even in cases of blindness. It is possible that VEP is an indicator of aggressive treatment for TON such as OCD.
Keywords: Optic canal decompression, Traumatic optic neuropathy, Visual-evoked potential
INTRODUCTION
Traumatic optic neuropathy (TON) is one of the serious complications of craniomaxillofacial trauma, with an incidence of 0.5–2.0% in head trauma, and its visual outcome is poor.[
We report a unilateral TON case complaining of blindness showing approximately 50% visual-evoked potential (VEP) activity, where VEP had begun to recover immediately after decompression during OCD operation. This is the first report to suggest that VEP may be a reliable indicator of OCD operation for TON.
CLINICAL REPORT
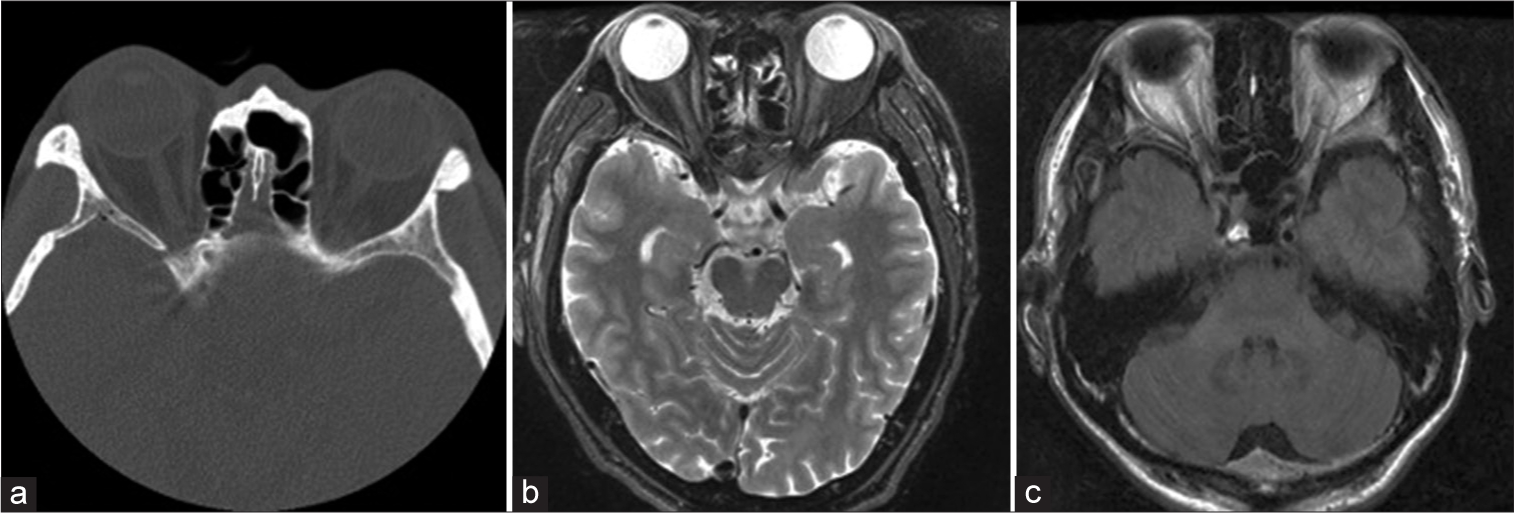
A 48-year-old man fell from a height of 7 m while working, striking his head, and losing sight completely in his right eye immediately afterward. His consciousness score was 14 points on the Glasgow Coma Scale (E6 V4 M4); his right pupil was 7 mm, and his left pupil was 3 mm. He had no light perception and the direct light reflex disappeared in the right pupil. There were no fractures or traumatic lesions on the head thin-slice computed tomography and magnetic resonance imaging [
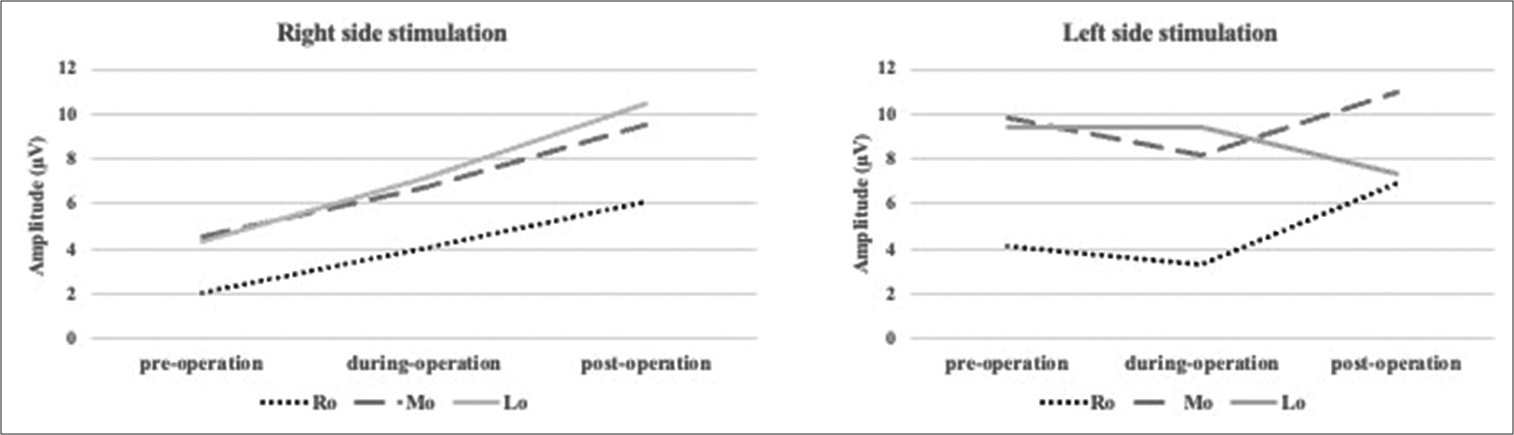
Figure 4:
Changes of visual-evoked potential during operation and follow-up time. After craniotomy and drilling out of the optic canal, the amplitude increased at all electrodes in the right-sided stimulation. The final measurement improved from 2.1 μV to 6.1 μV at L0 (Left occipital electrode), from 4.5 μV to 9.5 μV at M0 (Middle occipital electrode), and from 4.3 μV to 10.4 μV at R0 (Right occipital electrode).
DISCUSSION
TON, which occurs in up to 2% of patients after head trauma, is classified into direct and indirect injuries.[
CONCLUSION
The retained VEP activity in TON may suggest the recovery potential of the injured optic nerve, even in cases of blindness. It is possible that VEP is an indicator of aggressive treatment for TON such as OCD.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
Acknowledgments
The authors thank Keiko Nakahara for technical assistance.
References
1. Agarwal A, Mahapatra AK. Visual outcome in optic nerve injury patients without initial light perception. Indian J Ophthalmol. 1999. 47: 233-6
2. Chen B, Zhang H, Zhai Q, Li H, Wang C, Wang Y. Traumatic optic neuropathy: A review of current studies. Neurosurg Rev. 2022. 45: 1895-913
3. Chen HH, Lee MC, Tsai CH, Pan CH, Lin YT, Chen CT. Surgical decompression or corticosteroid treatment of indirect traumatic optic neuropathy: A randomized controlled trial. Ann Plast Surg. 2020. 84: S80-3
4. Entezari M, Rajavi Z, Sedighi N, Daftarian N, Sanagoo M. High-dose intravenous methylprednisolone in recent traumatic optic neuropathy; a randomized double-masked placebo-controled clinical trial. Graefes Arch Clin Exp Ophthalmol. 2007. 245: 1267-71
5. Fujitani T, Inoue K, Takahishi T, Ikushima K, Asai T. Indirect traumatic optic neuropathy--visual outcome of operative and nonoperative cases. Jpn J Opthalmol. 1986. 30: 125-34
6. Hayashi H, Kawaguchi M. Intraoperative monitoring of flash visual evoked potential under general anesthesia. Korean J Anesthesiol. 2017. 70: 127-35
7. Holmes MD, Sires BS. Flash visual evoked potentials predict visual outcome in traumatic optic neuropathy. Ophthalmic Plast Reconstr Surg. 2004. 20: 342-6
8. Karimi S, Arabi A, Ansari I, Shahraki T, Safi S. A systematic literature review on traumatic optic neuropathy. J Ophthalmol. 2021. 2021: 5553885
9. Miller NR. Traumatic optic neuropathy. J Neurol Surg B Skull Base. 2021. 82: 107-15
10. Odom JV, Bach M, Brigell M, Holder GE, McCulloch DL, Mizota A. ISCEV standard for clinical visual evoked potentials: (2016 update). Doc Ophthalmol. 2016. 133: 1-9
11. Singman EL, Daphalapurkar N, White H, Nguyen TD, Panghat L, Chang J. Indirect traumatic optic neuropathy. Mil Med Res. 2016. 3: 2
12. Siyanaki MR, Azab MA, Lucke-Wold B. Traumatic optic neuropathy: Update on management. Encyclopedia (Basel 2021). 2023. 3: 88-101
13. Steinsapir KD, Goldberg RA. Traumatic optic neuropathy. Surv Ophthalmol. 1994. 38: 487-518
14. Wei W, Zhao SF, Li Y, Zhang JL, Wu JP, Liu HC. The outcome of surgical and non-surgical treatments for traumatic optic neuropathy: A comparative study of 685 cases. Ann Transl Med. 2022. 10: 542
15. Wladis EJ, Aakalu VK, Sobel RK, McCulley TJ, Foster JA, Tao JP. Interventions for indirect traumatic optic neuropathy: A report by the American academy of ophthalmology. Ophthalmology. 2021. 128: 928-37
16. Yu-Wai-Man P, Griffiths PG. Surgery for traumatic optic neuropathy. Cochrane Database Syst Rev. 2013. 6: CD005024