- Department of Neurological Surgery, Nippon Medical School, Tokyo, Japan
Correspondence Address:
Fumihiro Matano, MD. PhD., Senior Assistant Professor, Department of Neurological Surgery, Nippon Medical School, Tokyo, Japan.
DOI:10.25259/SNI_626_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Fumihiro Matano, Shigeyuki Tahara, Yujiro Hattori, Yohei Nounaka, Koshiro Isayama, Akira Teramoto, Akio Morita. Wrapping method for better fat handling in endoscopic trans-sphenoidal surgery. 25-Oct-2024;15:390
How to cite this URL: Fumihiro Matano, Shigeyuki Tahara, Yujiro Hattori, Yohei Nounaka, Koshiro Isayama, Akira Teramoto, Akio Morita. Wrapping method for better fat handling in endoscopic trans-sphenoidal surgery. 25-Oct-2024;15:390. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13156
Abstract
Background: Fat is commonly used for preventing cerebrospinal fluid (CSF) leakage during endoscopic transsphenoidal surgery (ETSS). However, fat is soft, slippery, and sometimes not easy to handle. The present study aimed to examine the efficacy of our Surgicel® wrapping method, which allows for better fat handling, in preventing the occurrence of CSF leakage among patients undergoing ETSS.
Methods: We used fat tissues removed from the abdomen. The fat was cut with scissors into pieces that were approximately 5 mm in size. Surgicel® was also cut into 2.5 cm2. The fat tissues were encased with these Surgicel® squares and slightly moistened with a saline solution.
Results: Between January 2023 and August 2024, 34 patients aged 18–86 years (average 54.9 years) underwent ETSS. Among these patients, 20 had pituitary tumors, 6 had Rathke’s cysts, and 8 had other conditions. None of the patients had CSF leakage postoperatively. The use of Surgicel®-wrapped fat during ETSS is better than the use of fat alone.
Conclusion: The Surgicel® wrapping method allows for better fat handling during ETSS.
Keywords: Endoscopic trans-sphenoidal surgery, Fat handling, Surgicel wrap
INTRODUCTION
Endoscopic trans-sphenoidal surgery (ETSS) has been widely performed owing to the recent advancements in endoscopic cameras and technology.[
MATERIALS AND METHODS
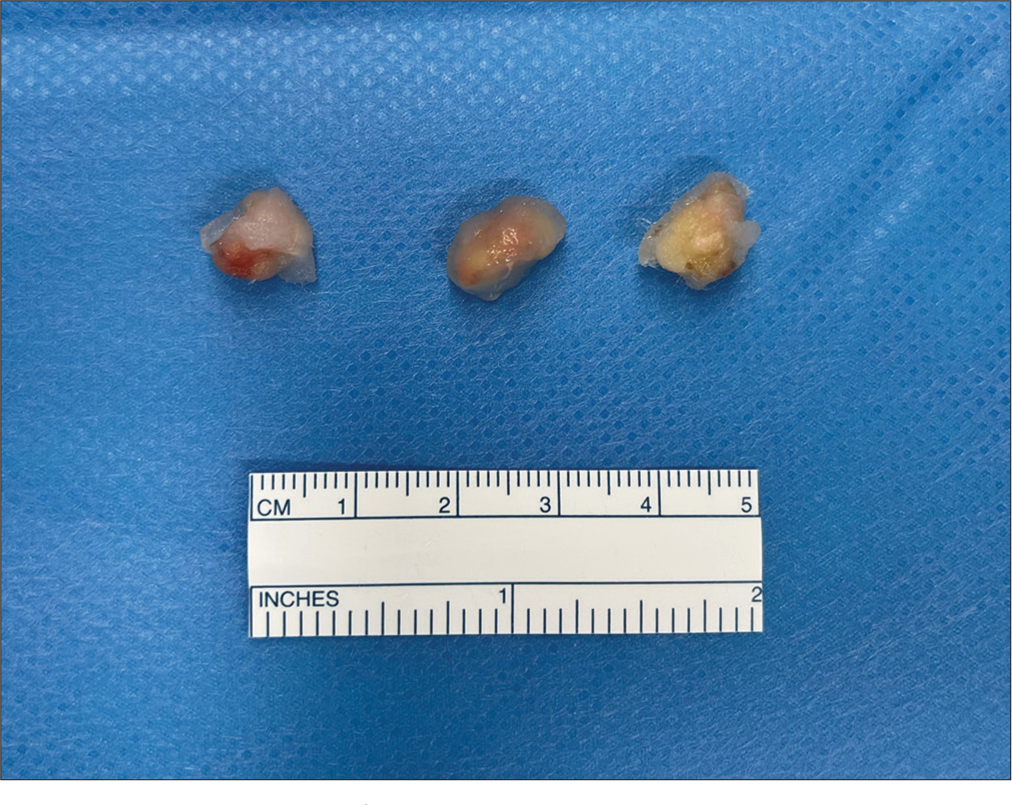
We used fat removed from the abdomen. The size of the fat removed depended on the size of the dural opening and the extent of CSF leakage. In our cases, we removed approximately 3 cm2 of fat. The fat tissues were cut with scissors to approximately 5 mm in size [
Surgicel® was then cut into 2.5 cm2 [
Video 1
RESULTS
From January 2023 to August 2024, the Surgicel® wrapping method was performed on 34 patients who underwent ETSS, including 18 male and 16 female patients. The patient’s age ranged from 18 to 86 years (average, 54.9 years). Among the 34 patients, 20 had pituitary neuroendocrine tumors, 6 had Rathke’s cysts, 1 had a craniopharyngioma, 1 had a chordoma, and 6 had other conditions. The average follow-up period was 7.9 months, and no patient had CSF leakage postoperatively.
DISCUSSION
We have presented a method of encapsulating fat with Surgicel® and demonstrated its usefulness.
Minimally invasive ETSS has been expanding its application in recent years, not only for pituitary neuroendocrine tumors but also for craniopharyngioma, meningioma, chordoma, and chondrosarcoma, owing to the development of its techniques and instruments,[
Classically, several methods are widely used for preventing CSF leakage, such as fat closure, femoral fascia closure, suturing the dura mater,[
Fat is slippery and does not easily fit into the implantation site, making it difficult to handle. To solve this problem, we have developed a method of encasing a fat mass in Surgicel®.
Surgicel® is fluffy cotton commonly used as a hemostatic agent and cost effective and widely used cost effective in neurosurgery. Wrapping the fat with Surgicel® creates friction on the surface of the fat mass, making it less slippery and much easier to handle. The fat is also shaped into a lump by being encased in Surgicel®, which provides a hemostatic effect. We sometimes fill the fat and then suture the dura mater, but even in this case, the fat fits better, and the suturing becomes easier. In addition, surgeons can adjust the number of fat pieces according to the volume of the extraction cavity since small tumor extraction cavities require fewer pieces, whereas larger cavities require more pieces.
Of course, CSF leakage can be caused by various factors, and it cannot be solved by this method alone. However, the ease of fat handling is considered a significant advantage.
CONCLUSION
The Surgicel® wrapping method is useful to ensure better fat handling during ETSS.
Limitation
The Surgicel® wrapping method led to improved handling of fat tissues during ETSS with a reduced risk of CSF leakage. However, we have not conducted a comparative study involving cases that underwent ETSS with and without Surgicel® wrapping, so there is still a lack of scientific evidence of the efficacy of our technique.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Video available online at
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Ahn S, Park JS, Kim DH, Kim SW, Jeun SS. Surgical experience in prevention of postoperative CSF leaks using abdominal fat grafts in endoscopic endonasal transsphenoidal surgery for pituitary adenomas. J Neurol Surg B Skull Base. 2021. 82: 522-7
2. D’Alessandris QG, Rigante M, Mattogno PP, La Rocca G, Romanello M, Auricchio AM. Impact of 4K ultra-high definition endoscope in pituitary surgery: Analysis of a comparative institutional case series. J Neurosurg Sci. 2022. 66: 425-33
3. Hara T, Akutsu H, Yamamoto T, Tanaka S, Takano S, Ishikawa E. Cranial base repair using suturing technique combined with a mucosal flap for cerebrospinal fluid leakage during endoscopic endonasal surgery. World Neurosurg. 2015. 84: 1887-93
4. Khan DZ, Ali AM, Koh CH, Dorward NL, Grieve J, Layard Horsfall H. Skull base repair following endonasal pituitary and skull base tumour resection: A systematic review. Pituitary. 2021. 24: 698-713
5. Kshettry VR, Lobo B, Lim J, Sade B, Oya S, Lee JH. Evaluation of non-watertight dural reconstruction with collagen matrix onlay graft in posterior fossa surgery. J Korean Neurosurg Soc. 2016. 59: 52-7
6. Matano F, Froelich S. Overview and pitfalls of the extended Trans: Nasal endoscopic approach. No Shinkei Geka. 2022. 50: 634-43
7. Murai Y, Shirokane K, Sato S, Higuchi T, Kubota A, Ozeki T. Preliminary clinical surgical experience with temporary simultaneous use of an endoscope during exoscopic neurosurgery: An observational study. J Clin Med. 2022. 11: 1753
8. Nassimizadeh A, Lancer H, Hodson J, Ahmed S. Three-dimensional endoscopic endonasal surgery: A systematic review. Laryngoscope. 2022. 132: 1895-903
9. Shahein M, Montaser AS, Barbero JM, Maza G, Todeschini AB, Otto BA. Collagen matrix with mucoperiosteum graft as an effective fatless flapless reconstruction after endoscopic pituitary adenoma resection. Oper Neurosurg (Hagerstown). 2020. 19: E573-80
10. Shahein M, Prevedello DM, Beaumont TL, Ismail K, Nouby R, Palettas M. The role of indocyanine green fluorescence in endoscopic endonasal skull base surgery and its imaging correlations. J Neurosurg. 2020. 135: 923-33
11. Shen M, Qiao N, Shou X, Chen Z, He W, Ma Z. Collagen sponge is as effective as autologous fat for grade 1 intraoperative cerebral spinal fluid leakage repair during transsphenoidal surgery. Clin Neurol Neurosurg. 2022. 214: 107131
12. Zhou Z, Zuo F, Chen X, Zhao Q, Luo M, Jiang X. Risk factors for postoperative cerebrospinal fluid leakage after transsphenoidal surgery for pituitary adenoma: A meta-analysis and systematic review. BMC Neurol. 2021. 21: 417