- Department of Neurosurgery, Graduate School of Medical Sciences, Kanazawa University, Kanazawa, Ishikawa, Japan
Correspondence Address:
Mitsutoshi Nakada
Department of Neurosurgery, Graduate School of Medical Sciences, Kanazawa University, Kanazawa, Ishikawa, Japan
DOI:10.4103/2152-7806.194501
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Tomoya Kamide, Masanao Mohri, Kouichi Misaki, Naoyuki Uchiyama, Mitsutoshi Nakada. Intracranial aneurysm formation after radiotherapy for medulloblastoma. 21-Nov-2016;7:
How to cite this URL: Tomoya Kamide, Masanao Mohri, Kouichi Misaki, Naoyuki Uchiyama, Mitsutoshi Nakada. Intracranial aneurysm formation after radiotherapy for medulloblastoma. 21-Nov-2016;7:. Available from: http://surgicalneurologyint.com/surgicalint_articles/intracranial-aneurysm-formation-after-radiotherapy-for-medulloblastoma/
Abstract
Background:The development of an intracranial aneurysm after radiotherapy is rare but secondary effect of cranial irradiation in a primary disease treatment.
Case Description:The patient was a 17-year-old male adolescent who was diagnosed as having a posterior fossa medulloblastoma when he was 8 years old. He had undergone tumor resection with radiotherapy and chemotherapy. A distal posterior inferior cerebellar artery aneurysm was identified by magnetic resonance imaging 8 years after radiotherapy and grew rapidly throughout the next 1 year. The patient underwent microsurgical clipping and was discharged without deficit.
Conclusion:This experience demonstrates that physicians caring for patients who have undergone intracranial radiotherapy should carefully consider the possibility of an aneurysmal formation when conducting follow-up imaging.
Keywords: Chemotherapy, intracerebral aneurysm, medulloblastoma, radiation induced
INTRODUCTION
Radiotherapy is increasingly being performed for many intracerebral lesions. The benefits have been proven, however, negative consequences have also been reported.[
CASE REPORT
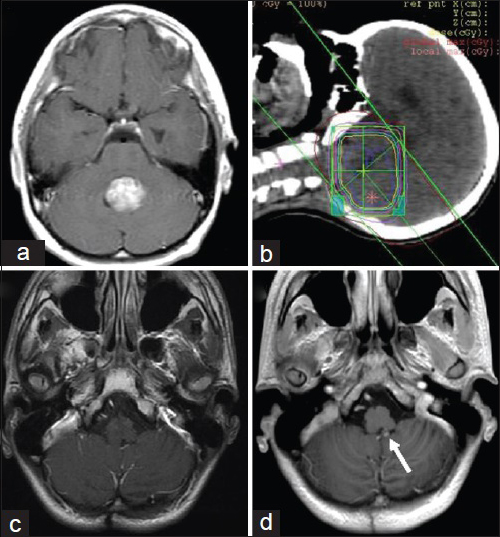
A 17-year-old man was found to have a posterior fossa medulloblastoma when he was 8 years old [
Figure 1
Primary tumor and follow-up magnetic resonance imaging. (a) Gross-total removal of the medulloblastoma. (b) Radiotherapy at 32.4 Gy for the posterior fossa and 23.4 Gy for the whole brain and spine; consequently, 55.8 Gy was irradiated around the tumor cavity. (c) Image obtained 7 years later showing no evident aneurysmal formation. (d) The 5-mm hyperintense nodule (arrow) on the continuous wall of the resected cavity discovered 9 years later
At 17 years of age, Gd-enhanced T1-weighted MR image revealed a 5-mm hyperintense nodule on the continuous wall of the resected cavity [
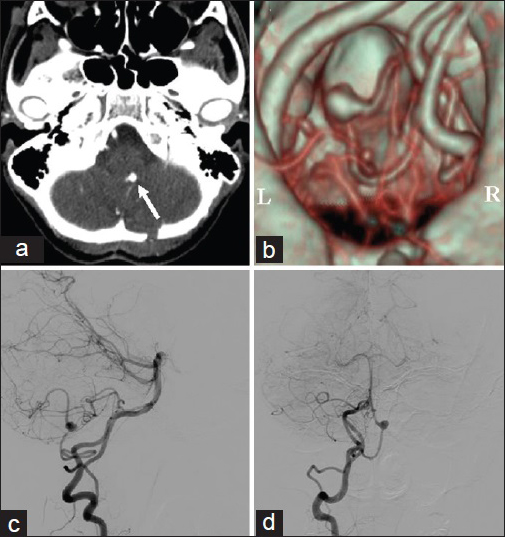
Figure 2
Radiological findings of aneurysm. (a, b) A three-dimensional computed tomographic angiogram showing that the nodule was a right posterior inferior cerebellar artery aneurysm (arrow). R, right and L, left. (c) Lateral and (d) anteroposterior digital subtraction angiographic views confirming the fenestrated vertebral artery and the aneurysm between the infratonsillar and supratonsillar loops
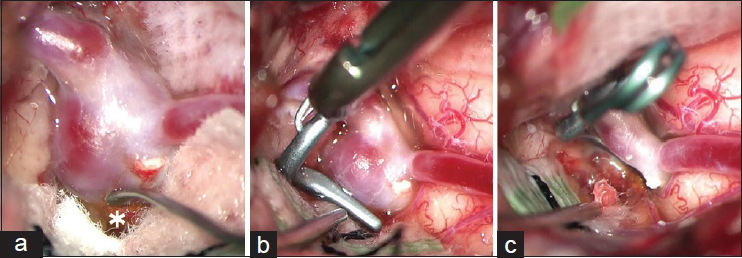
The patient underwent suboccipital craniotomy. The wall of the parent artery and aneurysm was normal, and the neck of saccular aneurysm was clipped using a fenestrated L-shaped clip to maintain the parent-artery flow [
DISCUSSION
Ionizing radiation has been linked to certain cerebrovascular pathologies, including radiation-induced vasculopathy, atherosclerotic vascular changes, vascular stenosis and occlusion, intracerebral hemorrhage, cavernous malformation, and aneurysmal formation.[
The pathophysiological mechanism of radiation-induced aneurysms is likely to resemble that of radiation-induced vasculopathy, in which initial endothelial injury caused by radiation results in aneurysmal change.[
Regarding radiation-induced vasculopathy, the Child Cancer Survivor Study reported that tumor relapse, cranial radiotherapy, and concurrent alkylating chemotherapy with radiotherapy are risk factors of stroke.[
Radiation-induced aneurysms are considered more fragile. The reported frequency of rupture was significantly greater than that in nonradiation-induced aneurysms; 55% presented with some form of hemorrhage and only 13% presented with incidental hemorrhage.[
In our case, 3D-CTA could reveal an PICA aneurysm clearly. However, we additionally performed DSA to consider how to treat the aneurysm. Owing to the irregular morphology of the radiation-induced aneurysms, detailed evaluation were essential to decide the treatment among neck clipping, coil embolization, proximal occlusion, and aneurysmal trapping with or without bypass. This may suggest that 3D-CTA is sufficient to detect radiation-induced aneurysms, however, DSA is recommended to manage these unusual aneurysms.
Intracranial aneurysms in irradiated fields are rare but are an important secondary effect of cranial radiotherapy for a primary tumor. Careful attention should be paid on serial follow-up of possible vascular involvement in long-term surviving patients who have undergone radiotherapy.
CONCLUSION
We reported a case of radiation-induced distal PICA aneurysm after radiotherapy for medulloblastoma. Our case suggests aneurysmal formation following radiotherapy is a rare but potentially late delayed complication. Thus, careful follow-up of imaging including vascular analysis is necessary for long-term survivors with cranial irradiation.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Benson PJ, Sung JH. Cerebral aneurysms following radiotherapy for medulloblastoma. J Neurosug. 1989. 70: 545-50
2. Bowers DC, Liu Y, Leisenring W, McNeil E, Stovall M, Gurney JG. Late-occurring stroke among long-term survivors of childhood leukemia and brain tumors: A report from the childhood cancer survivor study. J Clin Oncol. 2006. 24: 5277-82
3. Campen CJ, Kranick SM, Kasner SE, Kessler SK, Zimmerman RA, Lustig R. Cranial irradiation increases risk factor of stroke in pediatric brain tumor survivors. Stroke. 2012. 43: 3035-40
4. Maruyama K, Mishima K, Saito N, Fujimaki T, Sasaki T, Kirino T. Radiation-induced aneurysm and moyamoya vessels presenting with subarachnoid hemorrhage. Acta Neurochir. 2000. 142: 139-43
5. Matsumoto H, Minami H, Yamaura I, Yoshida Y. Radiation-induced cerebral aneurysm treated with endovascular coil embolization. Interv Neuroradiol. 2014. 20: 448-53
6. Murphy ES, Merchant TE, Yu JS, Chao ST, Suh JH. Review of cranial radiotherapy-induced vasculopathy. J Neurooncol. 2015. 122: 421-9
7. Nanney AD, Najib EE, Ahmadieh TY, Daou MR, Bit Ivan EN, Maymont MH. Intracranial aneurysms in previously irradiated fields: Literature review and case report. World Neurosurg. 2014. 81: 511-9
8. O’Connor MM, Mayberg MR. Effects of radiation on cerebral vasculature; A review. Neurosurgery. 2000. 46: 138-51
9. Sciubba DM, Gallia GL, Recinos P, Garonzik IM, Clatterbuck RE. Intracranial aneurysm following radiation therapy during childhood for a brain tumor. J Neurosurg. 2006. 105: 134-9
10. Scodary DJ, Tew JM, Thomas GM, Tomsick Th, Liwnicz BH. Radiation-induced cerebral aneurysms. Acta Neurochir. 1990. 102: 141-4
11. Yamaguchi S, Kato T, Takeda M, Ikeda H, Kitamura K. Ruptured distal anterior inferior cerebellar artery aneurysm following stereotactic irradiation for vestibular schwannoma: Case report. Neurol Med Chir. 2009. 49: 202-5