- Department of Neurosurgery, Faculty of Medicine, Yamagata University, Yamagata, Japan
Correspondence Address:
Yasuaki Kokubo
Department of Neurosurgery, Faculty of Medicine, Yamagata University, Yamagata, Japan
DOI:10.4103/sni.sni_73_18
Copyright: © 2018 Surgical Neurology International This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.How to cite this article: Yuki Yamada, Yasuaki Kokubo, Kanako Kawanami, Hiroshi Itagaki, Shinji Sato, Yukihiko Sonoda. A case report: C2 radiculopathy induced by neck flexion due to the cord compression of C2 segmental type vertebral artery relieved by microvascular decompression. 15-May-2018;9:101
How to cite this URL: Yuki Yamada, Yasuaki Kokubo, Kanako Kawanami, Hiroshi Itagaki, Shinji Sato, Yukihiko Sonoda. A case report: C2 radiculopathy induced by neck flexion due to the cord compression of C2 segmental type vertebral artery relieved by microvascular decompression. 15-May-2018;9:101. Available from: http://surgicalneurologyint.com/surgicalint-articles/a-case-report-c2-radiculopathy-induced-by-neck-flexion-due-to-the-cord-compression-of-c2-segmental-type-vertebral-artery-relieved-by-microvascular-decompression/
Abstract
Background:Decompression of an anomalous vertebral artery (VA) may effectively treat cervical myelopathy/radiculopathy due to resultant spinal cord or nerve compression. Here we report a case of C2 radiculopathy induced by neck flexion due to cord compression of the C2 segmental type VA relieved by microvascular decompression.
Case Description:A 30-year-old female presented with left occipitalgia, sensory abnormalities in the left upper and lower extremities, and neck pain induced by neck flexion. The magnetic resonance imaging (MRI) revealed an abnormal flow void, confirming that the VA was compressing the spinal cord at the C1 level. Three-dimensional computed tomography (3D-CT) showed an anomalous course of the left VA, which entered the spinal canal between the axis and atlas. Microvascular decompression was performed by transposing the artery (e.g., anchoring it to the dura using PTEF): this effectively relieved cord compression.
Conclusion:An anomalous VA rarely causes cervical radiculopathy induced by neck flexion. When it occurs, microvascular decompression effectively relieves pressure resulting in a resolution of symptoms.
Keywords: Anomalous vertebral artery, C2 segmental type vertebral artery, cervical radiculopathy, microvascular decompression
INTRODUCTION
C2 radiculopathy may be attributed to and cervical compression may be attributed to an anomalous vertebral artery (VA). These patients may present with symptoms consistent with other neurovascular compression syndromes; for example, hemifacial spasm, trigeminal neuralgia, and glossopharyngeal neuralgia. Previously, microvascular decompression of anomalous VA had effectively treated these disorders.[
CASE REPORT
A 30-year-old female exhibited neck pain induced by neck flexion. This was considered to be C2 radiculopathy. The neurological examination was normal. SEP and MEG of the upper extremities were normal. The cervical x-ray was unremarkable, but the motion-sensitized driven-equilibrium (MSDE)-turbo spin echo (TSE)[
Figure 1
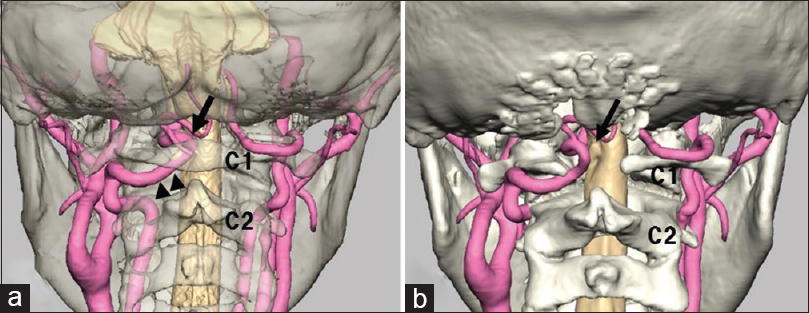
Fusion images by MRI and three-dimensional computed tomography (3D-CT) angiography. (a) Preoperation, (b) postoperation. (a) shows the anomalous course of the left VA, which entered the spinal canal between the axis and atlas (arrowhead). There was no fenestration of the VA and no laterality of the diameter of the VA. The intradural course of the left VA formed a vascular loop and compressed the spinal cord at the C1 level (arrow). (b) shows that the left VA was separated from the surface of the cord accompanied by C1 laminectomy (arrow)
Figure 2
Pre- and postoperative MRI findings. (a) Motion-sensitized driven-equilibrium-turbo spin echo (MSDE-TSE), (b) T2-WI: preoperative magnetic resonance imaging (MRI). (c) MSDE-TSE, (d) T2-weighted image (T2-WI): postoperative MRI. (a) shows that the cervical cord at the C1 level is compressed by the left vertebral artery (VA). (b) shows an abnormal flow void indicating that the left VA is compressing the spinal cord at the C1 level without a signal change in the spinal cord. (c) and (d) show that the left VA was separated from the surface of the cord. The compression of the cord was relieved after the operation
She underwent microvascular surgical decompression of the cord by performing a VA mobilization procedure. This required a suboccipital craniectomy and C1 laminectomy (e.g., midline skin incision). The left VA was accessed through a paramedian dural incision. The left VA was mobilized laterally and anchored to the dura mater by PTEF tape (2 mm; BARD) [
Figure 3
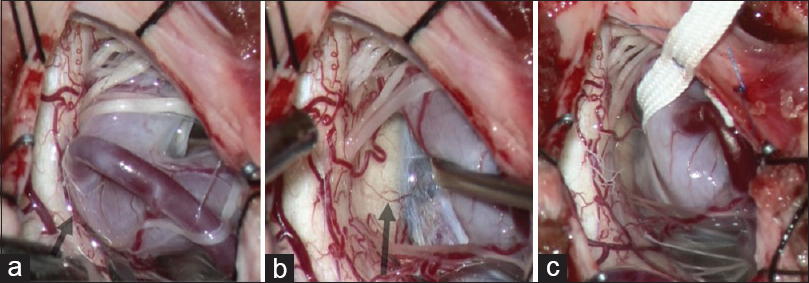
Intraoperative photographs. (a) The vascular loop of the left VA compressed the cervical cord at the C1 level and C2 dorsal nerve roots (arrow). (b) Impression by the left VA on the cord and stretched C2 nerve roots was observed (arrow). (c) The left VA was mobilized laterally and anchored to the dura mater by PTEF tape to relieve the cord compression
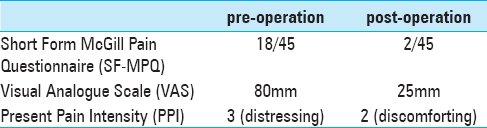
Postoperatively the patient was pain-free [
DISCUSSION
According to the previous reports describing the compression of the cervical cord or nerve roots by an elongated VA or VA anomaly inducing myelopathy or radiculopathy, such as trigeminal neuralgia and hemifacial spasm, the symptoms observed were radiculopathy, and/or myelopathy at the level of the cord compression. Most of the cases were treated by microvascular surgical decompression, with improvement of symptoms obtained in all cases.[
The characteristic features of our case are the young age (the youngest among the previous reports) and the symptom of neck pain induced by neck flexion. Only one other report[
Although the cause of neck pain induced by neck flexion is rarely radiculopathy/myelopathy due to compression of the cervical cord by the VA, surgical microvascular decompression can be effective when this is the case.
CONCLUSION
Anomalous VA is a rare cause of cervical radiculopathy induced by neck flexion. Microvascular decompression is an effective treatment for this disorder inducing symptom relief.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Isozumi T, Yamamoto A, Nishihara K, Nishiura I, KondoA , Handa H. Radiculomyelopathy caused by cord compression by an anomalous vertebral artery: A case report. Spinal Surg. 1999. 13: 181-6
2. Sellin JN, Al-Hafez B, Duckworth EA. Microvascular decompression of a C-2 segmental-type vertebral artery producing trigeminal hypesthesia. J Neurosurg. 2014. 121: 919-23
3. Takahashi T, Tominaga T, Hassan T, Yoshimoto T. Cervical cord compression with myelopathy caused by bilateral persistence of the first intersegmental arteries: Case report. Neurosurgery. 2003. 53: 234-7
4. Tokuda K, Miyasaka K, Abe H, Abe S, Takei H, Sugimoto S. Anomalous atlantoaxial portions of vertebral and posterior inferior cerebellar arteries. Neuroradiology. 1985. 27: 410-3
5. Vincentelli F, Caruso G, Rabehanta PB, Rey M. Surgical treatment of a rare congenital anomaly of the vertebral artery: Case report and review of the literature. Neurosurgery. 1991. 28: 416-20
6. Wang J, Yarnykh VL, Yuan C. Enhanced image quality in blackblood MRI using the improved motion-sensitized driven-equilibrium (iMSDE) sequence. J Magn Reson Imaging. 2010. 31: 1256-63
7. Watanabe K, Hasegawa K, Takano K. Anomalous vertebral artery-induced cervical cord compression causing severe nape pain. Case report. J Neurosurg. 2001. 95: 146-9