- Department of Neurosurgery, University Hospital Center Osijek, Osijek, Croatia
- Faculty of Medicine, Josip Juraj Strossmayer University of Osijek, Osijek, Croatia
- Department of Neurology, University Hospital Center Osijek, Osijek, Croatia
- Department of Pathology and Forensic Medicine, University Hospital Center Osijek, Osijek, Croatia
- Department of Oncology, University Hospital Center Osijek, Osijek, Croatia
- Department of Diagnostic and Interventional Radiology, University Hospital Center Osijek, Osijek, Croatia
- Department of Anesthesiology and Critical Care, University Hospital Center Osijek, Osijek, Croatia
- Department of Neurology, Požega County Hospital, Požega, Požeško-Slavonska, Croatia.
Correspondence Address:
Nenad Koruga, Department of Neurosurgery, University Hospital Center Osijek, Faculty of Medicine, Josip Juraj Strossmayer University of Osijek, Osijek, Croatia.
DOI:10.25259/SNI_66_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Nenad Koruga1,2, Alen Rončević1, Anamarija Soldo Koruga2,3, Jasmina Rajc2,4, Josipa Flam2,5, Tatjana Rotim2,6, Tajana Turk2,6, Sonja Škiljić2,7, Marijan Cesarik8, Tomislav Paun8. A rare presentation of leiomyosarcoma metastasis to the cervical spine: A case report and a brief review. 12-Apr-2024;15:128
How to cite this URL: Nenad Koruga1,2, Alen Rončević1, Anamarija Soldo Koruga2,3, Jasmina Rajc2,4, Josipa Flam2,5, Tatjana Rotim2,6, Tajana Turk2,6, Sonja Škiljić2,7, Marijan Cesarik8, Tomislav Paun8. A rare presentation of leiomyosarcoma metastasis to the cervical spine: A case report and a brief review. 12-Apr-2024;15:128. Available from: https://surgicalneurologyint.com/surgicalint-articles/12854/
Abstract
Background: Leiomyosarcoma (LMS) is a rare malignancy that originates from smooth muscle. The most common sites of metastases include the lungs, liver, kidney, and skin. Notably, metastases of LMS to the central nervous system/or spine are extremely rare. When a cervical spinal LMS lesion was encountered, the patient successfully underwent gross total tumor resection with negative margins.
Case Description: A 63-year-old female had undergone an anterior cervical C5–C7 diskectomy and fusion 18 years ago and resection of a retroperitoneal LMS 3 years ago. She newly presented with right-sided numbness and pain of 2 months duration that correlated with a focal right-sided C5-level hemiparesis (i.e., 4/5 motor strength). When the cervical magnetic resonance demonstrated a right-sided C5 intralaminar mass with extension into the C5–C6 foramen, she underwent posterior tumor resection; pathologically, this proved to be an LMS metastasis. Respectively, 1- and six months postoperatively, follow-up magnetic resonance imaging scans showed no tumor recurrence; she tolerated adjuvant oncological treatment accompanied by physical therapy. However, in one postoperative year, the lesion recurred, and she is presently under consideration for additional surgical management.
Conclusion: Gross total surgical resection is the first line of treatment for patients with metastatic LMS. Here, a patient with a C5 laminar/C5–C6 foraminal bony LMS metastasis underwent posterior tumor resection accompanied by adjuvant oncological treatment but exhibited disease recurrence within one postoperative year.
Keywords: Leiomyosarcoma, Metastasis, Radiculopathy, Spine
INTRODUCTION
Leiomyosarcoma (LMS) is a rare malignant tumor that arises from smooth muscle cells. It most commonly involves the uterus, followed by the gastrointestinal tract and retroperitoneum; its incidence is 0.7 cases per 100,000 patients/year.[
CASE REPORT
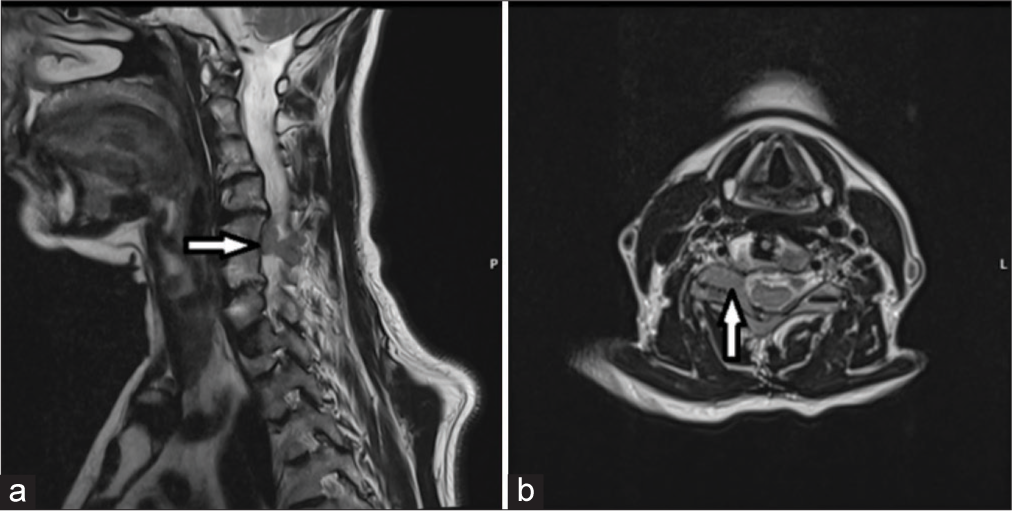
A 63-year-old female presented with a right mild hemiparesis (i.e., 4/5 motor deficit) and relative right-sided C5 sensory level of 1 month’s duration. In 2005, she had a C5–C7 anterior cervical diskectomy and fusion, while in 2021, she had a retroperitoneal LMS completely removed. She underwent posterior surgical resection of the right-sided C5 laminar/C5– C6 bony foraminal lesion documented by magnetic resonance imaging (MRI) that proved to be a LMS metastasis [
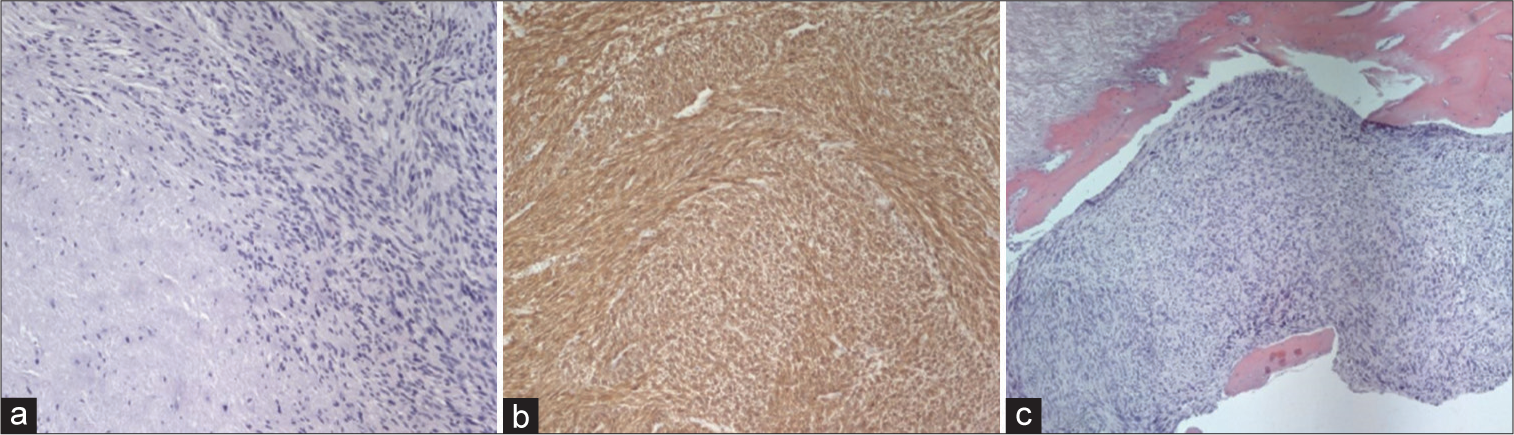
Figure 2:
(a) ×10 magnification – Hematoxylin and eosin staining: Spindle-shaped cells with moderate nuclear pleomorphism, with area of necrosis, (b) ×10 magnification – Immunohistochemical staining, diffuse smooth muscle actin, positivity in tumor cells, and (c) ×5 magnification – hematoxylin and eosin staining, tumor infiltration, and destruction of the bone.
Postoperative course
Postoperative cervical MRI scans revealed no tumor recurrence 1 and 6 months postoperatively [
DISCUSSION
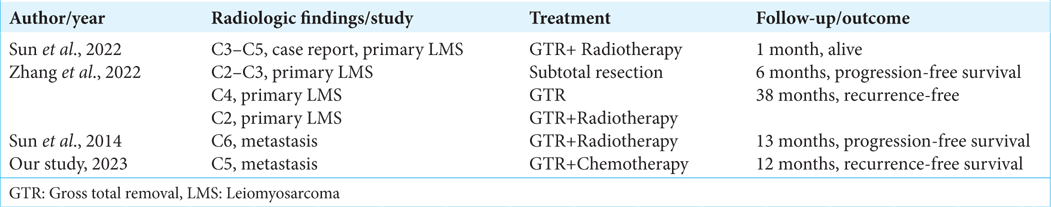
LMS rarely metastasizes to the spine
LMSs are highly malignant tumors that rarely metastasize to the spine. Sun et al., in 2013, reported a metastatic LMS lesion to the cervical spine with destruction of the C6 vertebra; the patient underwent an anterior decompression and fusion.[
Survival rates for spinal LMS
LMS are aggressive, highly malignant lesions that frequently recur and metastasize.[
Bony metastases for LMS lesions
LMS rarely causes osseous spinal vertebral metastases.[
CONCLUSION
The prognosis for patients with metastatic LMS is poor due to the high rate of metastases. Here, a 63-year-old female with a 2021 diagnosis of a retroperitoneal LMS was newly presented with a C5 laminar/C5–C6 foraminal bony lesion that, despite gross total posterior excision, recurred one year later.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Ducimetière F, Lurkin A, Ranchère-Vince D, Decouvelaere AV, Peoc’H M, Istier L. Incidence of sarcoma histotypes and molecular subtypes in a prospective epidemiological study with central pathology review and molecular testing. PLoS One. 2011. 6: e20294
2. Elhammady MS, Manzano GR, Lebwohl N, Levi AD. Leiomyosarcoma metastases to the 207spine. Case series and review of the literature. J Neurosurg Spine. 2007. 6: 178-83
3. Imura Y, Takenaka S, Outani H, Nakai T, Yasuda N, Nakai S. Impact of surgery and chemotherapy on metastatic extrauterine leiomyosarcoma. Curr Oncol. 2022. 29: 2301-11
4. LiBrizzi CL, Vankara A, Meyer CF, Levin AS, Morris CD. Bone metastases in patients with leiomyosarcoma: A retrospective analysis of survival and surgical management. Sarcoma. 2022. 2022: 6806932
5. Maimone G, Nicassio N, Malik I, Cambria M. Metastatic leiomyosarcoma of the spine 216 updates in management and surgical strategy. Open J Mod Neurosurg. 2013. 3: 98-103
6. Shapiro S. Myelopathy secondary to leiomyosarcoma of the spine. Case report. Spine. 1992. 17: 249-51
7. Sun H, Zhuang M, Cheng D, Zhu C, Liu Z, Qiu X. Primary leiomyosarcoma of cervical spine invading the vertebra without obvious osteoclasia: Case report and literature review. J Spinal Cord Med. 2022. 45: 643-7
8. Sun Z, Wang H, Yang H, Jiang W. Leiomyosarcoma metastatic to the cervical spine causing a C6 compression fracture: A case report. Oncol Lett. 2014. 8: 263-5
9. Zhang J, Chen Y, Xing X, Wang Q, Liu K, Zhang E. Primary leiomyosarcoma of the spine: an analysis of imaging manifestations and clinicopathological findings. Insights Imaging. 2022. 13: 195
10. Ziewacz JE, Lau D, La Marca F, Park P. Outcomes after surgery for spinal metastatic leiomyosarcoma. J Neurosurg Spine. 2012. 17: 432-7