- Department of Neurology, School of Medicine, Selçuk University, Konya, Turkey
- Department of Neurosurgery, School of Medicine, Selçuk University, Konya, Turkey
Correspondence Address:
Hulagu Kaptan
Department of Neurosurgery, School of Medicine, Selçuk University, Konya, Turkey
DOI:10.4103/2152-7806.176130
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ekmekci H, Kaptan H. Camptocormia and deep brain stimulation: The interesting overlapping etiologies and the therapeutic role of subthalamic nucleus-deep brain stimulation in Parkinson disease with camptocormia. Surg Neurol Int 10-Feb-2016;7:
How to cite this URL: Ekmekci H, Kaptan H. Camptocormia and deep brain stimulation: The interesting overlapping etiologies and the therapeutic role of subthalamic nucleus-deep brain stimulation in Parkinson disease with camptocormia. Surg Neurol Int 10-Feb-2016;7:. Available from: http://surgicalneurologyint.com/surgicalint_articles/camptocormia-and-deep-brain-stimulation-the-interesting-overlapping-etiologies-and-the-therapeutic-role-of-subthalamic-nucleus%e2%80%91deep-brain-stimulation-in-parkinson-disease-with-camptocormia/
Abstract
Background:Camptocormia is known as “bent spine syndrome” and defined as a forward hyperflexion. The most common etiologic factor is related with the movement disorders, mainly in Parkinson's disease (PD).
Case Description:We present the case of a 51-year-old woman who has been followed with PD for the last 10 years, and also under the therapy for PD. An unappreciated correlation low back pain with camptocormia developed. She underwent deep brain stimulation (DBS) in the subthalamic nucleus bilaterally and improved her bending posture.
Conclusion:The relationship between the DBS and camptocormia is discussed in this unique condition.
Keywords: Camptocormia, deep brain stimulation, Parkinson's disease
INTRODUCTION
Camptocormia is rarely reported in literature and is also known as “bent spine syndrome.” It was first described by Brodie in 1818. This date is 1 year later than the date that James Parkinson described the disease to be remembered by his name at the present time. Camptocormia is becoming an increasingly recognized finding of Parkinson patients and dystonic disorders. The main feature of this diagnosis is the marked forward flexion increase during insistent walking and the concomitant lower back pain commonly seen in most of the cases. Either the bending or the lumbar pain is improved in recumbent and supine position. Diagnosis is established exclusively upon clinical findings. In the past, psychogenic etiology was assumed to be the main reason; nowadays, the organic causes of camptocormia have been postulated. The other etiological causes of camptocormia are dystonia, spinal deformities, cerebrovascular diseases, and neuromuscular diseases. Psychiatric causes are less than previously thought. As mentioned earlier, the diagnosis of camptocormia is built upon clinical investigations, imaging of the brain and spinal cord, electromyography (EMG), or muscle biopsy when needed. Clinical treatment is limited and most unsuccessfully, it includes the supportive conservative measures to withdrawal of causative drugs, surgical corrections of spinal deformities, electroconvulsive therapy, and deep brain stimulation (DBS).[
DBS is a unique surgical procedure developed to treat several disabling neurological diseases mainly Parkinson's disease (PD), tremor, dystonia, and some psychiatric disorders. DBS is used only for patients who improve to some degree after PD medications, but whose symptoms cannot be adequately controlled with these medications in times. DBS uses a surgically implanted, battery-operated medical device called an implantable pulse generator (IPG) - deliver electrical stimulation to specific areas in the brain. Before the procedure, a DBS team uses magnetic resonance imaging (MRI) or computed tomography (CT) scanning to identify and locate the exact target within the brain for surgical intervention. Some DBS teams and also we use microelectrode recording – which involves recording electrodes that monitor the activity of nerve cells in the target area – to more specifically identify the precise subcortical nucleus that will be stimulated. In general, these areas are the thalamus (T), subthalamic nucleus (STN), and globus pallidus (GP). The DBS system consists of three components: The lead, the extension, and the IPG. The lead (also called an electrode) – a thin, insulated wire – is inserted through a burr hole and implanted in the brain. The tip of the electrode is positioned within the specific nucleus. The extension is an insulated wire that is passed under the skin of the head, neck, and shoulder, connecting the lead to the IPG. The IPG is the third component and is usually implanted under the skin near the clavicle. Once the system is in place, electrical impulses are sent from the IPG up along the extension wire and the lead and into a specific target. These impulses block abnormal electrical signals and alleviate PD motor symptoms. In time, DBS is programed in accordance with patient's symptoms and responses.
Herein, a case hosting two different etiologies for a rare condition named camptocormia in PDs will be discussed. The interesting and worth discussing is the different origin of the mutual effect of spine, i.e., lumbar radiculopathy; the other is brain, i.e. PD. Another aspect of importance is the role of DBS in this double-diseased patient.
CASE REPORT
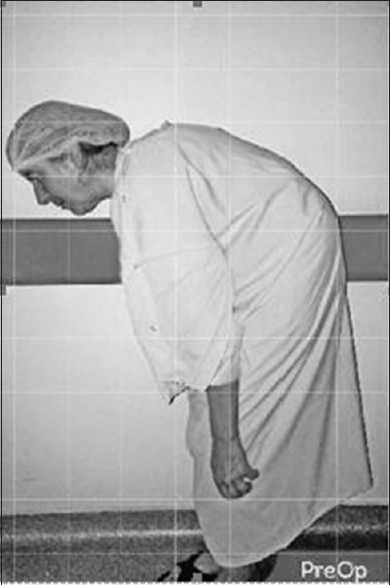
A 51-year-old woman followed with PD for the 10 years. Her chief complaints were bradykinesia mainly over the right side and slight resting tremor with moderate and sometimes severe low back pain (LBP). The pain was more pronounced while standing and walking. There was obvious and exaggerated bending posture in erection and moving [
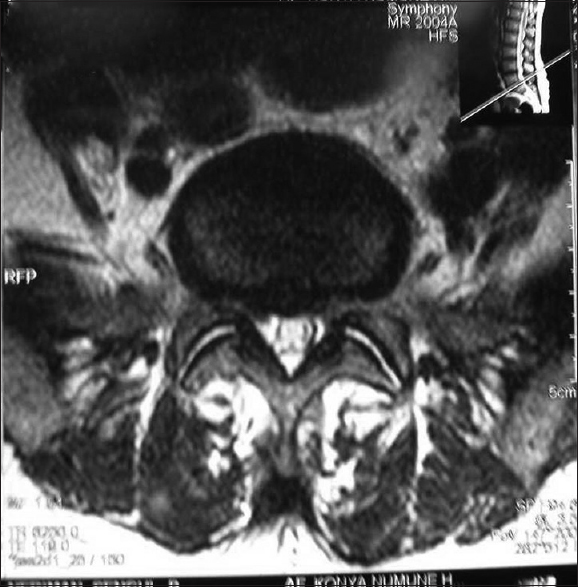
Seven years ago, the unbearable LBP came impaired her daily living time. She was diagnosed with L5–S1 disc disease with diffuse bulging and posterior central extruded herniation [
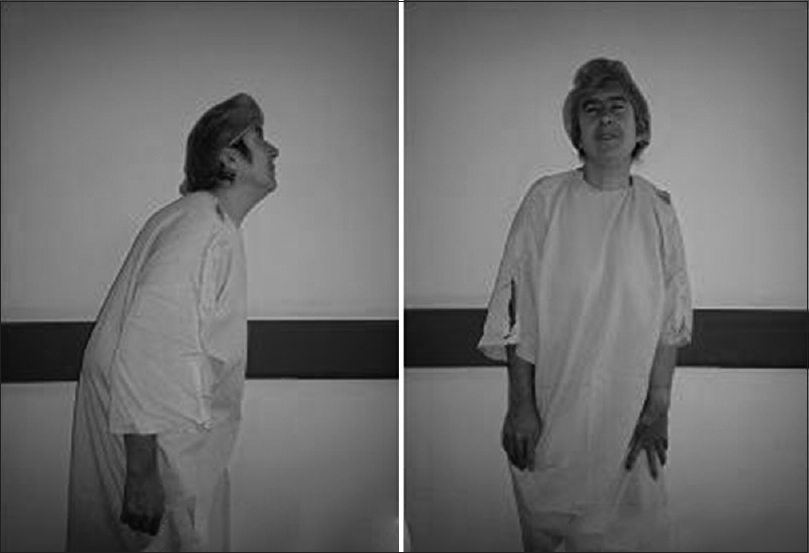
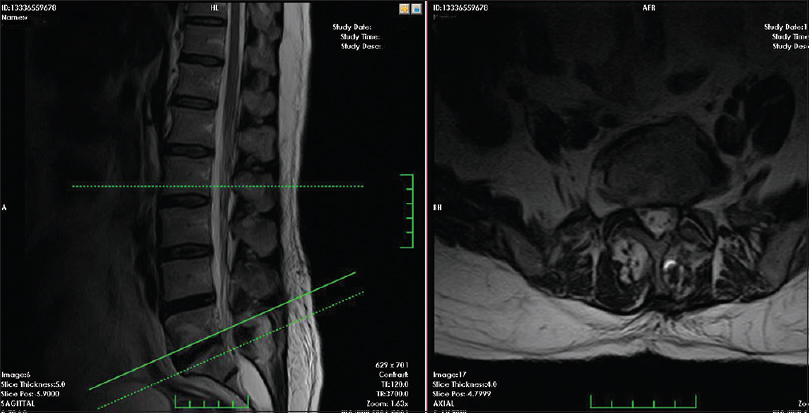
The vital respiratory capacity, parkin gene analysis, neuroimaging of spine, vertebral structures, and brain were all evaluated. She was ranked 8 for BFM-RS mainly with extreme bending of trunk, preventing standing, and walking in dystonia in many actions as provoking factors before the DBS attempt. The BFM score went down to 2 six months after the DBS installation; MED ON-MED OFF UPDRS scores were 14 and 20 at postoperative period, the dystonic truncal bending became insignificant clinically, the provoking factor was minimal dystonia in particular action, and bending was <10° [Figures
DISCUSSION
For the last 15 years, PD has linked to camptocormia and carefully studied. In the majority of the patient with camptocormia due to PD, it is unresponsive to levodopa. Most of the times, the severity of bent spine is often unalterable under the best medication through the PD course and does not change during the ON-OFF phases. The best-known correlation is between severity of PD and camptocormia. Our patient responded well to levodopa for PD, but the camptocormia was unresponsive. While PD worsened, camptocormia also became more severe. However, some other authors pointed out that there were no differences in PD with or without camptocormia on behalf of clinical and demographical characteristics. The prevalence of camptocormia with PD patients is highly fitful; as being 3–17%. May be, this wide range of percentage is due to unclear definition of camptocormia, or the differentiation of thresholds for diagnosis of camptocormia, or extensive patient groups. If we constrict camptocormia in PD, again there is a wide spectrum of PD-related abnormal postures ranging from striatal hand or foot deformity on one end of spectrum to scoliosis and camptocormia on the other end of spectrum.[
Most of the camptocormic PD patients exhibit initially bradykinesia, rigidity, and less frequently tremor. As the general rule for PD, apparent symptoms start asymmetric. Our case's symptoms started asymmetric, and the dominant feature of PD was bradykinesia. Unusual finding was the overlapping and prominence of back pain. While a small number of patients with camptocormic PD are painless, the majority of them are associated with lower back pain. Our case suffered a pronounced pain just leading and accompanying the camptocormia. In literature, some patients report a feeling of being pulled forward or sometimes a sensation of tightening in their abdomen. Our patient is a woman, and the initial bending problem was accompanied of a squeeze in her abdomen. All pulmonary function tests were within normal limit. Being a female may have a role on breathing with abdominal function wherein camptocormia interferes with pulmonary function. These patients may suffer that the paraspinal muscles can have a wooden consistency and the rectus abdominis often feels tense. In our case, especially rectus abdominus and the other abdominal muscles did not show any palpable contractions. However, in such cases, “botulinum type A” therapy may be a safe and effective treatment approach for camptocormia. We did not make any injections because there were no prominent abdominal contractions.[
Another etiological factor for camptocormia is myopathy of paravertebral muscles that may bring out a consequence of pathologic changes in the antigravity muscles involved in trunk extension. In our case, EMGs inclosing paravertebral and abdominal muscles were consistent with nonspecific extensors and overactive flexors and with dystonic discharges. The latter did not implicate any myopathic activity. Patient's blood level of creatine kinase was in normal range. Therefore, a localized muscle biopsy was not carried out. Some camptocormic patients may be mixed with a “dropped head syndrome,” since patients may try to compensate the flexion of body with an abnormal posture of neck.[
As aforementioned, the pathophysiology of axial postural abnormalities in PD is not well understood. Previously, it is related with psychiatric basics. In our case, a possibility of disorders attributed to hysteria, malingering, or other psychiatric diagnosis were all excluded. Since psychogenic movement disorders disrupt truncal flexion and complicated psychogenic dystonia may develop; in our case, “the criteria for psychogenic dystonia” were also excluded.
The ideal therapy for camptocormia in PD is a dilemma. Spinal surgery has been tried to solve the postural abnormalities for the patient with camptocormia, since it has significant complications and often requires revision surgery. Our presented patient has a paradoxical situation since yet the camptocormia was not manifested, she was operated at right L5 radiculopathy for severe pain. Spinal surgery was carried out at the 7th year of PD. In postoperative period, pain disappeared lightly, but camptocormic state was quickened and BFM-RS was increased from 4 to 8 in 1 year. The pain reemerged more severe. In this case, the camptocormia became more prominent within 7–8 years. Idiopathic PD with camptocormia was accelerated by surgery for the radiculopathy iatrogenically.[
The result of pharmacological treatment of camptocormia is correlated with PD treatment. Surprisingly, with cohort studies, up to 20% of PD patients with camptocormia benefit from L-Dopa treatment. Dopamine agonist agents are supposed to deteriorate the camptocormic course.[
We applied bilateral DBS-STN in our cases and followed her monthly for 6 months. Later, we extended control examinations. From the beginning of the 1st month, postural abnormality showed serious improvement. However, the best improvement was achieved in LBP with ≥7/10 in S-LANNS pain scale. Another surprise outcome is minimal improvement in blunt personality and moderate gain in MMSE by 2 score at the 1st year follow-up. Since she is at the age of early 50s and a homemaker, she has restarted to work at home and garden. Daily L-Dopa intake has been decreased by 40% in amount.
The affectivity and role of DBS-STN in camptocormia in PD is not clear in mechanism. Probably, beside the improvement in PD symptoms and motor fluctuations, there should be a positive additive by effects on the dystonia. But with this hypothesis – if camptocormia would be a dystonia primarily – GPi-DBS should be the preferred treatment. In reality, this is not the case. In accordance with STN, the GPi-DBS for PD with camptocormia in literature is very less in number. Tani et al. observed that the dystonic posture improved slightly in long-term instead of early period.[
Another important point is that camptocormia increases with action. In other words, it ceases with sitting and lying back. There may be a different mechanism involving spinal pathway so that in these patients there should be dystonic pulsation with motion coordinated with different mechanism involving in PD not only limited in brain, but also with spinal cord. This idea may sound that there is a different pathway just like “Restless Leg Syndrome” where there is a totally different mechanism from PD, but responsive to L-Dopa. Therefore, there may be a spinal mechanism both making a connection with spinal bending and with PD.
In the light of this knowledge, preferences for treatment of PD patients with camptocormia should be in favor of STN-DBS. This case was operated for LBP; then not only PD, but also these surgical attempts have an effect on camptocormia. This should be acceptable that surgery at lumbar area could be a peripheral, inductive core role in camptocormia. This doubled favorability was managed very well with stereotactic neurosurgery as bilateral STN-DBS. The diagnosis and treatment of camptocormia will continue to require expert knowledge in movement and neuromuscular disorders. Etiology and curative approach for camptocormia are crucial. Since, the clinical evaluation and etiological approach are really hard, neurological and neurosurgical insights should be carried out carefully; therefore, both groups work on with a precise multidisciplinary manner. This case is unique since camptocormia is developed with overlapping of both ongoing features of PD and spinal surgical intervention at the same time.[
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Abe K, Uchida Y, Notani M. Camptocormia in Parkinson's disease. Parkinsons Dis 2010. 2010. p.
2. Azher SN, Jankovic J. Camptocormia: Pathogenesis, classification, and response to therapy. Neurology. 2005. 65: 355-9
3. Gdynia HJ, Sperfeld AD, Unrath A, Ludolph AC, Sabolek M, Storch A. Histopathological analysis of skeletal muscle in patients with Parkinson's disease and ‘dropped head’/’bent spine’ syndrome. Parkinsonism Relat Disord. 2009. 15: 633-9
4. Koller H, Acosta F, Zenner J, Ferraris L, Hitzl W, Meier O. Spinal surgery in patients with Parkinson's disease: Experiences with the challenges posed by sagittal imbalance and the Parkinson's spine. Eur Spine J. 2010. 19: 1785-94
5. Lepoutre AC, Devos D, Blanchard-Dauphin A, Pardessus V, Maurage CA, Ferriby D. A specific clinical pattern of camptocormia in Parkinson's disease. J Neurol Neurosurg Psychiatry. 2006. 77: 1229-34
6. Ma H, McEvoy KM, Milone M. Sporadic inclusion body myositis presenting with severe camptocormia. J Clin Neurosci. 2013. 20: 1628-9
7. Margraf NG, Wrede A, Rohr A, Schulz-Schaeffer WJ, Raethjen J, Eymess A. Camptocormia in idiopathic Parkinson's disease: A focal myopathy of the paravertebral muscles. Mov Disord. 2010. 25: 542-51
8. Sako W, Nishio M, Maruo T, Shimazu H, Matsuzaki K, Tamura T. Subthalamic nucleus deep brain stimulation for camptocormia associated with Parkinson's disease. Mov Disord. 2009. 24: 1076-9
9. Tani NKaji RGoto SPublished: 2014 Mar 26. DOI: 10.5772/57103. Available from: http://www.intechopen.com/books/a-synopsis-of-parkinson-sdisease/deep-brain-stimulation-for-camptocormia-associated-with-parkinsons-disease .
10. Thani NB, Bala A, Kimber TE, Lind CR. High-frequency pallidal stimulation for camptocormia in Parkinson disease: Case report. Neurosurgery. 2011. 68: E1501-5