- Department of Neurosurgery, Complejo Hospitalario de Navarra, Calle Irunlarrea 3, CP 31008, Pamplona
- Department of Neurosurgery, Hospital Universitario Central de Asturias, Avda Roma s/n, Oviedo, Spain
DOI:10.25259/SNI-87-2019
Copyright: © 2019 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Sayoa Alvarez de Eulate-Beramendi, Kelvin Manuel Piña-Batista, Juan Carlos Rial-Basalo. Extradural en-plaque spinal lipomatous meningioma: A case report and literature review. 26-Mar-2019;10:49
How to cite this URL: Sayoa Alvarez de Eulate-Beramendi, Kelvin Manuel Piña-Batista, Juan Carlos Rial-Basalo. Extradural en-plaque spinal lipomatous meningioma: A case report and literature review. 26-Mar-2019;10:49. Available from: http://surgicalneurologyint.com/surgicalint-articles/9234/
Abstract
Background: Extradural spinal meningiomas are rare, and few appear as lipomatous meningiomas in an “en-plaque” form. The transitional fibroblastic subtype, with lipid accumulation within the tumoral cells, is typically more aggressive and surgically challenging to resect.
Case Description: A 42-year-old male presented with neck pain and progressive paresthesias in both upper extremities. Based on the radiological findings, the tentative preoperative diagnosis was lymphoma. However, the biopsy confirmed a meningioma. The patient underwent a combined extradural anterior and posterior approach, resulting in full tumor resection. Histopathologically, the final report documented a lipomatous meningioma.
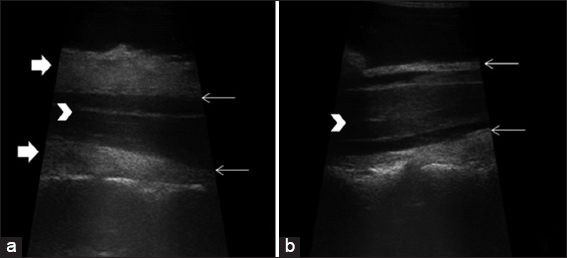
Conclusion: Extradural spinal lipomatous meningiomas (i.e., “en-plaque”) are rare and typically result in rapid clinical deterioration. The radiological diagnosis may be difficult, while ultrasonography helps to define their extradural location facilitating planning for gross total anterior/posterior excision where indicated.
Keywords: Lipomatous meningioma, meningioma en-plaque, spinal meningioma
INTRODUCTION
Spinal meningiomas account for approximately 25% of primary spinal cord tumors.[
CASE REPORT
Clinical and radiographic presentation
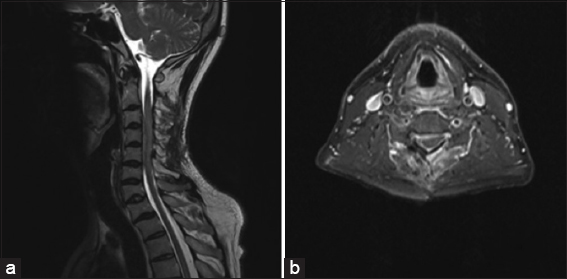
A 42-year-old male presented with neck pain, progressive paresthesias, tightness in both upper extremities, and 6 months of numbness involving the fourth and fifth digits of the left hand. His only neurological deficit was decreased pin appreciation in the left 4th and 5th digits. The magnetic resonance image (MRI) showed a circumferential tumor extending from C2 to C7 levels, resulting in maximal cord compression between C3 and C5. The lesion was isointense on both T1- and T2-weighted images and intensely homogeneously enhanced with gadolinium [
Biopsy and surgery
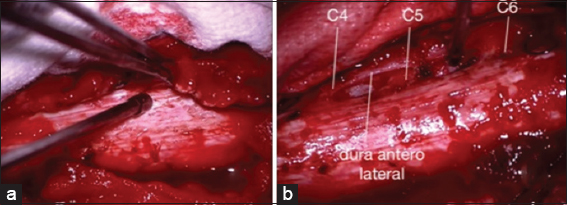
After an open biopsy revealed a meningioma, the patient initially underwent a C3–C7 laminoplasty, with theremoval of posterior tumor, and decompression of the dural sac. At surgery, the extradural tumor was grayish, white, non-suckable, and fibrous; it was carefully peeled off the dura [
When the postoperative MRI documented residual anterior tumor, the patient underwent a C4 and C5 anterior corpectomy/fusion to achieve gross total tumor resection.
Histopathology
Histopathological analysis revealed meningothelial uniform cells accompanied by mature adipocyte-like cells with peripherally displaced nuclei (e.g., ovoid nuclei with stippled chromatin and eosinophilic cytoplasm with fat vacuoles in their cytoplasm). There was no necrosis, mitotic activity, or hemorrhage. These findings confirmed the diagnosis of a transitional lipomatous meningioma [
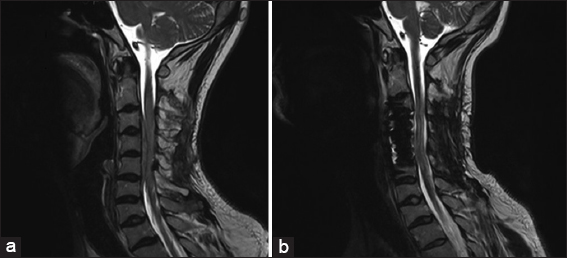
For 3 postoperative years, the patient has remained asymptomatic and follow-up MR studies showed no residual/recurrent disease [
DISCUSSION
Frequency of extradural spinal meningiomas (ESMs)
Meningiomas make up 25% of primary spinal tumors.[
MR findings consistent with ESM
The diagnosis of ESM is established utilizing MR scans, for example, isointense on T1-weighted, isointense/slightly hyperintense on T2-weighted images with “en-plaque” encirclement of the thecal sac, with or without calcification (1%–4.6%), but with homogeneous contrast enhancement.[
Histopathology of ESM
Histopathologically, most meningiomas are meningothelial, followed by the fibroblastic types. Lipomatous meningiomas are a rare variant of the latter subtype and are characterized by lipid accumulation inside the tumoral cells (i.e., metaplastic change called lipomatous or lipoblastic).[
Recommended surgical management of ESM
Gross total excision is the procedure of choice for managing ESM. In addition, there are various adjuvant therapies that may be utilized (e.g., so as to treat atypical or malignant meningiomas).[
Recurrence rate of ESM
Over a 5-year period, lipomatous ESMs typically show rapid clinical progression and are 4 times more likely to recur versus typical intradural meningiomas; recurrences are much more frequent following initial subtotal resection.[
CONCLUSIONS
En-plaque lipomatous ESMs are rare extradural lesions that often demonstrate rapid clinical and radiographic progression. As they are thick, fibrous, tenacious, often calcified, and may encircle the dura, gross total surgical excision may warrant combined anterior/posterior approaches.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Alafaci C, Grasso G, Granata F, Salpietro FM, Tomasello F. Ossified spinal meningiomas: Clinical and surgical features. Clin Neurol Neurosurg. 2016. 142: 93-7
2. Colnat-Coulbois S, Kremer S, Weinbreck N, Pinelli C, Auque J. Lipomatous meningioma: Report of 2 cases and review of the literature. Surg Neurol. 2008. 69: 398-402
3. D'Amico A, Napoli M, Cirillo M, D'Arco F, D'Anna G, Caranci F. Imaging of cervical extradural en-plaque meningioma. A case report. Neuroradiol J. 2012. 25: 598-603
4. Frank BL, Harrop JS, Hanna A, Ratliff J. Cervical extradural meningioma: Case report and literature review. J Spinal Cord Med. 2008. 31: 302-5
5. Levy WJ, Bay J, Dohn D. Spinal cord meningioma. J Neurosurg. 1982. 57: 804-12
6. Pant I, Gautam VKS, Kumari R, Chaturvedi S. Spinal tumour: Primary cervical extradural meningioma at an unusual location. J Spine Surg. 2017. 3: 509-13
7. Sivaraju L, Thakar S, Ghosal N, Hegde AS. Cervical en-plaque extradural meningioma involving brachial plexus. World Neurosurg. 2017. 108: 994.e7-000
8. Tuli J, Drzymalski DM, Lidov H, Tuli S. Extradural en-plaque spinal meningioma with intraneural invasion. World Neurosurg. 2012. 77: 202.e5-13
9. Yamada S, Kawai S, Yonezawa T, Masui K, Nishi N, Fujiwara K. Cervical extradural en-plaque meningioma. Neurol Med Chir (Tokyo). 2007. 47: 36-9
10. Yüksel MO, Gürbüz MS, Tanrıverdi O, Özmen SA. Lipomatous meningioma: A rare subtype of benign metaplastic meningiomas. J Neurosci Rural Pract. 2017. 8: 140-2