- Department of Neurosurgery, Hospital Mater Dei, Belo Horizonte, Brazil
- Department of Neurosurgery, University of Washington, Seattle, Washington, USA
- Department of Neurosurgery, Benjamin Guimarães Foundation, Belo Horizonte, Brazil
- Department of Neurosurgery, University of Texas Southwestern, Dallas, Texas, USA
Correspondence Address:
Marcelo D. Vilela
Department of Neurosurgery, Hospital Mater Dei, Belo Horizonte, Brazil
Department of Neurosurgery, Benjamin Guimarães Foundation, Belo Horizonte, Brazil
DOI:10.4103/sni.sni_122_17
Copyright: © 2017 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Marcelo D. Vilela, Bruno P. Braga, Hugo A. S. Pedrosa. Long iliac screw fixation in a case of isthmic spondyloptosis. 13-Jun-2017;8:110
How to cite this URL: Marcelo D. Vilela, Bruno P. Braga, Hugo A. S. Pedrosa. Long iliac screw fixation in a case of isthmic spondyloptosis. 13-Jun-2017;8:110. Available from: http://surgicalneurologyint.com/surgicalint-articles/long-iliac-screw-fixation-in-a-case-of-isthmic-spondyloptosis/
Abstract
Background:We report the case of a patient with a spondyloptosis who presented with progressive deformity and worsening neurological deficits. The patient had two previous lumbosacral instrumented fusions.
Case Description:A salvage revision surgery was performed, in which long iliac screws along with anterior column support at L5-S1 were used to immobilize the lumbosacral junction. Two years after the procedure a solid fusion is seen along with marked neurological improvement.
Conclusions:Pelvic fixation using long iliac screws is a very useful technique that can be employed when revision surgery for high-grade spondylolisthesis is needed.
Keywords: Iliac screws, lumbosacral fusion, pelvic fixation, spondylolisthesis, spondyloptosis
INTRODUCTION
Achieving a solid fusion across the lumbosacral junction in complex deformity cases is challenging due to the unfavorable biomechanics at this level, poor sacral bone quality, and high cantilever loads. Complications include the loss of sacral fixation, sacral fractures, rod breakage, and pseudoarthrosis. The addition of iliac screws improves fusion rates and decreases the incidence of these complications.[
CASE REPORT
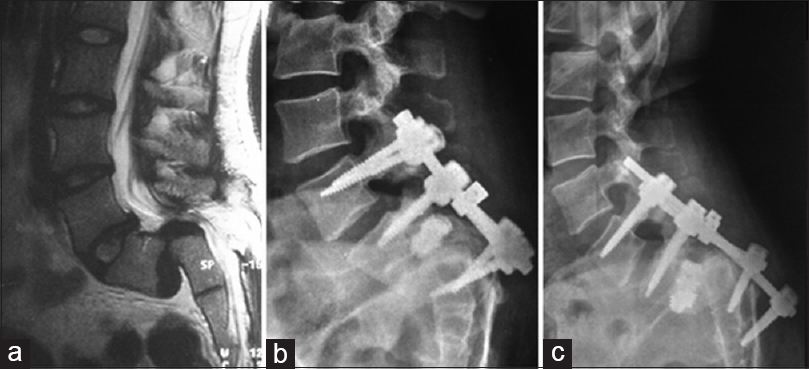
A.P.L.S, a 31-year-old female presented with progressive severe back/buttocks pain, tenesmus, urinary incontinence, nocturnal enuresis, bilateral foot drop and plantar flexion weakness (strength II out of V) related to a spondyloptosis [
Figure 1
(a) T2-weighed sagittal MRI showing a L5-S1 spondyloptosis. (b) Plain lateral X-ray demonstrating pullout of the sacral screws and cage migration into the spinal canal following the first lumbopelvic fixation. (c) Plain lateral X-ray demonstrating pullout of the S1 and S2 screws with loss of correction and spondyloptosis after the second lombopelvic fixation
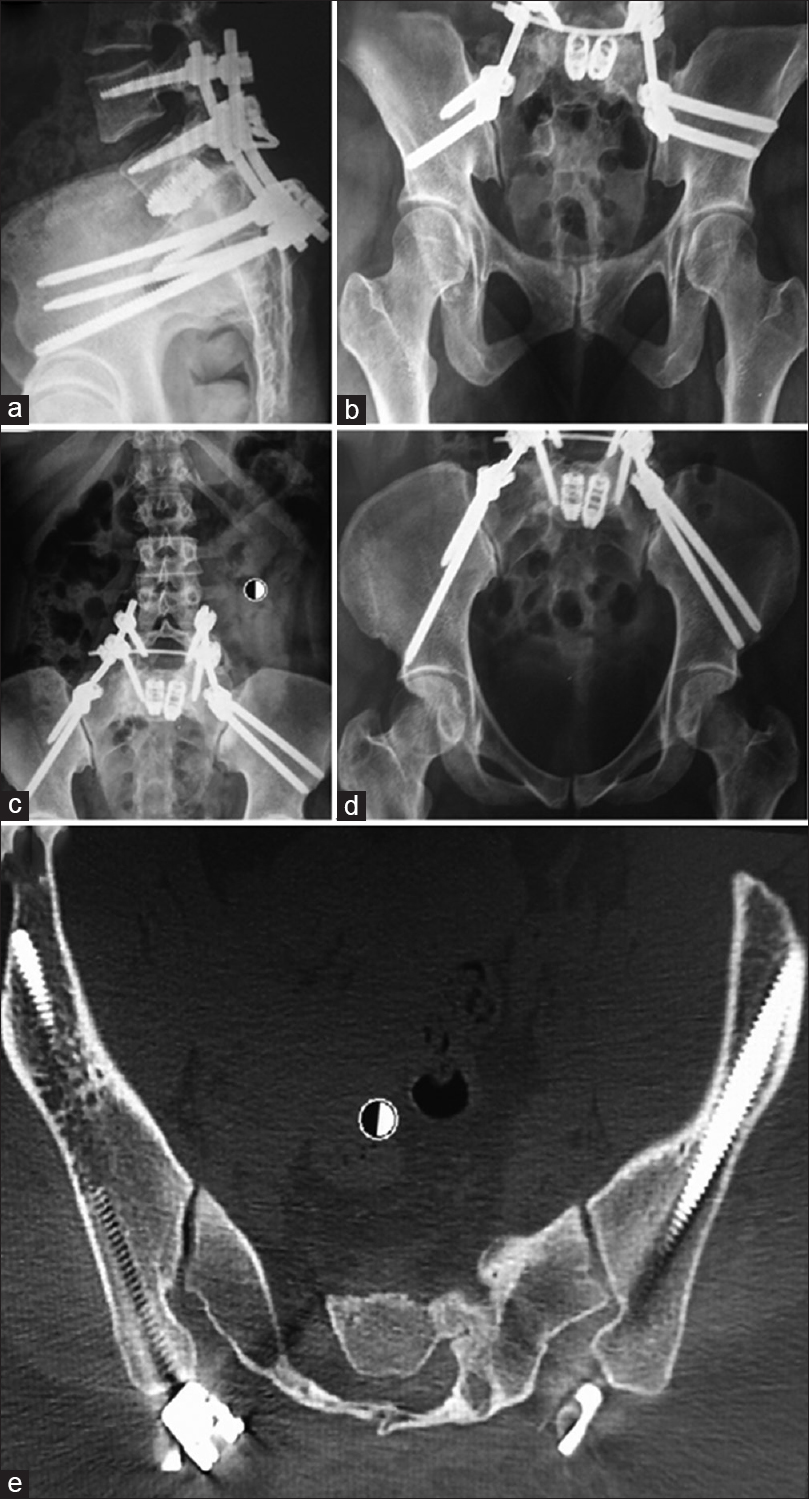
Fourth surgery
The fourth surgery included a posterior lumbopelvic instrumented fusion using bilateral long iliac screws, with the addition of BMP-2 into the disc space. Four iliac screws were placed, two on each side, three of them measuring 7 × 120 mm and the other 7 × 45 mm. Although known to be very useful in spine surgery, we did not have navigation nor neurophysiological monitoring available at that time. After iliac screw placement, anteroposterior (AP), outlet, inlet and combined obturator-oulet pelvis views were used to confirm adequate placement without sciatic notch or acetabular fossa penetration. All screws were connected directly to the rods without the use of offside connectors. This allowed a cantilever force that enabled partial reduction of the slip and indirect decompression of the spinal canal. The cages that had been previously inserted were left in place to maintain an anterior column support. The patient was allowed to ambulate immediately after surgery without any type of cast, as recommended by some authors when performing lumbopelvic fixations.[
Postoperative imaging
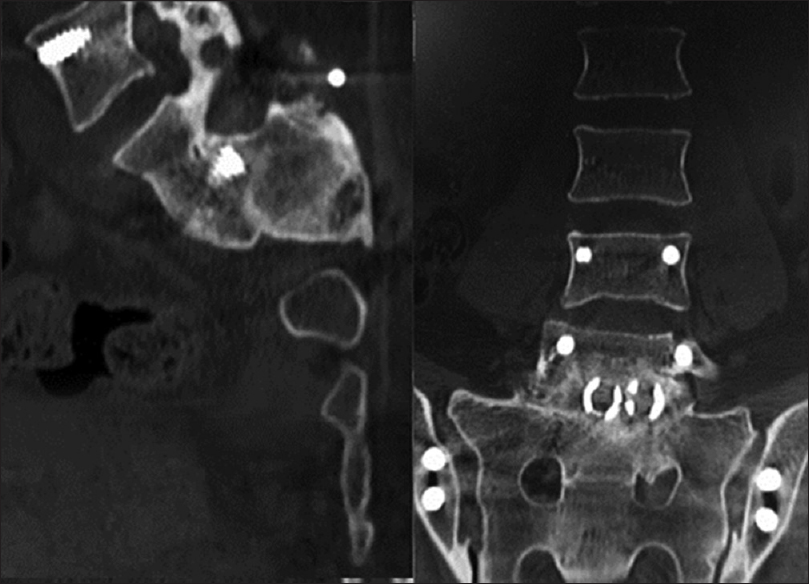
Postoperative imaging studies demonstrated reduction of the slip to a grade II and excellent placement of the iliac screws [
DISCUSSION
Achieving fusion across the lumbosacral junction can be quite challenging in deformity cases, and different techniques can be employed to immobilize the L5-S1 disc in revision cases.[
The technique of iliac fixation may or may not involve transfixation of the sacroiliac joint, depending on whether the starting point is located at S2[
One legitimate concern is that iliac fixation might immobilize the sacroiliac joint and lead to its early degeneration. Long-term studies have documented this not to be true and therefore there should not be a concern when opting for this type of fixation.[
There are not many reports on the use of salvage iliac screws to manage failed instrumented fusions for high-grade spondylolisthesis.[
The absence of sacral screws did not impair the formation of a solid fusion in the long term. While most reports detail the use of iliac fixation to provide protection of sacral screws, we decided to remove the sacral screws instead and rely on the strong iliac fixation to immobilize the L5-S1 disc, which proved to be efficacious in our patient.
CONCLUSIONS
In the presented case, salvage pelvic fixation was very effective in maintaining the lumbosacral joint immobility while fusion took place. This case highlights the usefulness of long iliac screws and L5-S1 anterior column support in cases of failed surgery for high-grade spondylolisthesis.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Bellabarba C, Schildhauer A, Vaccaro AR, Chapman JR. Complications associated with surgical stabilization of high-grade sacral fracture dislocations with spino-pelvic instability. Spine. 2006. 31: S80-S8
2. Bridwell KH. Utilization of iliac screws and structural interbody grafting for revision spondylolisthesis surgery. Spine (Phila Pa 1976). 2005. 30: S88-96
3. McCord DH, Cunningham BW, Shono Y, Myers JJ, McAfee PC. Biomechanical analysis of lumbosacral fixation. Spine (Phila Pa 1976). 1992. 17: S235-43
4. O’Brien JR, Matteini L, Yu WD, Kebaish KM. Feasibility of minimally invasive sacropelvic fixation: Percutaneous S2 alar iliac fixation. Spine (Phila Pa 1976). 2010. 35: 460-4
5. Santos ER, Sembrano JN, Mueller B, Polly DW. Optimizing iliac screw fixation: A biomechanical study on screw length, trajectory, and diameter. J Neurosurg Spine. 2011. 14: 219-25
6. Schildhauer TA, McCulloch P, Chapman JR, Mann FA. Anatomic and radiographic considerations for placement of transiliac screws in lumbopelvic fixations. J Spinal Disord Tech. 2002. 15: 199-205
7. Tsuchiya K, Bridwell KH, Kuklo TR, Lenke LG, Baldus C. Minimum 5-year analysis of L5-S1 fusion using sacropelvic fixation (bilateral S1 and iliac screws) for spinal deformity. Spine (Phila Pa 1976). 2006. 31: 303-8
8. Zheng ZM, Zhang KB, Zhang JF, Yu BS, Liu H, Zhuang XM. The effect of screw length and bone cement augmentation on the fixation strength of iliac screws: A biomechanical study. J Spinal Disord Tech. 2009. 22: 545-50