- Department of Neurological Surgery, Chicago Medical School At Rosalind Franklin University of Medicine and Science, North Chicago, IL, USA
- Department of Orthopedic Surgery, Northwestern University Feinberg School of Medicine, Chicago, IL, USA
- Department of Neurological Surgery, Northwestern University Feinberg School of Medicine, Chicago, IL, USA
- Department of Neurological Surgery and Pathology, Northwestern University Feinberg School of Medicine, Chicago, IL, USA
Correspondence Address:
Zachary A. Smith
Department of Neurological Surgery, Northwestern University Feinberg School of Medicine, Chicago, IL, USA
DOI:10.4103/sni.sni_156_18
Copyright: © 2018 Surgical Neurology International This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.How to cite this article: Maia Winkel, Cort D. Lawton, Olabisi R. Sanusi, Craig M. Horbinski, Nader S. Dahdaleh, Zachary A. Smith. Neuro-surgical considerations for treating IgG4-related disease with rare spinal epidural compression. 17-Oct-2018;9:209
How to cite this URL: Maia Winkel, Cort D. Lawton, Olabisi R. Sanusi, Craig M. Horbinski, Nader S. Dahdaleh, Zachary A. Smith. Neuro-surgical considerations for treating IgG4-related disease with rare spinal epidural compression. 17-Oct-2018;9:209. Available from: http://surgicalneurologyint.com/surgicalint-articles/9041/
Abstract
Background:Immunoglobulin G4-related disease (IgG4-RD) is a group of distinct autoimmune disorders affecting nearly every organ system in the body. Although central nervous system involvement is quite rare, it may present as hypertrophic pachymeningitis more frequently affecting the brain than the spine. In this study, we provide a case of spinal IgG4-RD pseudotumor resulting in cord compression, and a comprehensive review of the literature.
Case Description:A patient presented with an extradural mass causing spinal cord compression at the L2-L3 level. Pathologically this proved to be an IgG4-RD pseudotumor. The patient was treated with thecal sac decompression and post-operative steroids that resulted in complete resolution of his symptoms.
Conclusion:IgG4-RD is typically under-recognized and under-reported in the spinal literature. The clinical spinal presentation and non-surgical vs. surgical treatment are relatively straightforward. Although most cases can be managed with a course of steroids, surgical decompression may be required in patients presenting with spinal cord and/or nerve root compression. The differential diagnoses for these spinal tumors or pseudotumors should include IgG4-RD. Early detection and appropriate treatment can lead to satisfactory outcomes.
Keywords: Hypertrophic pachymeningitis, IgG4-RD, IgG4-RD pseudotumor, IgG4-related disease, pachymeningitis
INTRODUCTION
Immunoglobulin G4-related disease (IgG4-RD) is a family of orphan, autoimmune diseases, which share key features affecting nearly all systems throughout the body.[
In this study, we summarized 15 cases of spinal IgG4-RD found in the literature and added our case of IgG4-related spinal pachymeningitis contributing to spinal cord compression. The patient presented responded well to surgical decompression and post-operative steroid administration. This highlights how important it is for spine surgeons to consider this disease, as early detection and treatment result in improved outcomes.
CASE REPORT
Clinical background
A 48 year-old female presented with 8 weeks of lower back pain, neurogenic claudication, and right lower extremity radiculopathy. On examination, she was neurologically intact.
Imaging
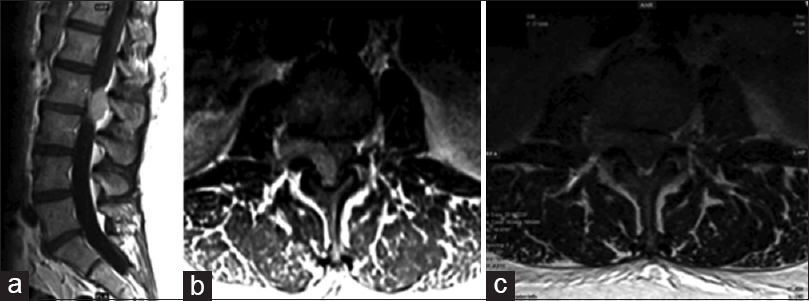
The MRI of her lumbar spine with and without contrast showed an enhancing extradural mass at the L2-L3 level extending into the right neural foramen, contributing to severe central and right L2-L3 foraminal stenosis [
Surgical technique
The patient underwent central and right neural foraminal decompression at the L2-L3 level. The tumor capsule was clearly defined. Tumor originated from the right lateral recess-L2-L3 neural foramen. An excisional biopsy provided the histopathological diagnosis on frozen section of a lymphoproliferative tumor. According to the intra-operative frozen section, the tumor was debulked allowing for decompression of the thecal sac. Additional samples were subsequently sent for a lymphoma panel evaluation.
Postoperative course
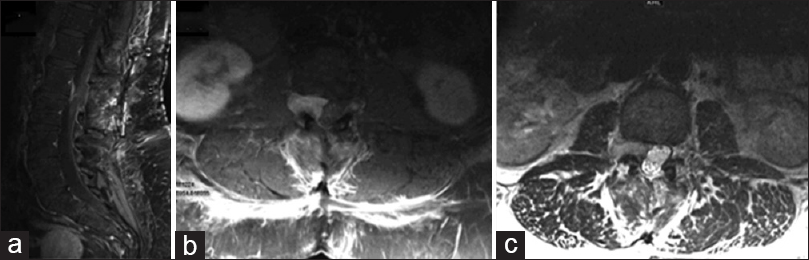
Postoperatively, she was started on 4 mg of intravenous dexamethasone every 6 h. The postoperative lumbar MRI showed the thecal sac, and neural elements at the L2-L3 level was adequately decompressed [
Histopathological diagnosis
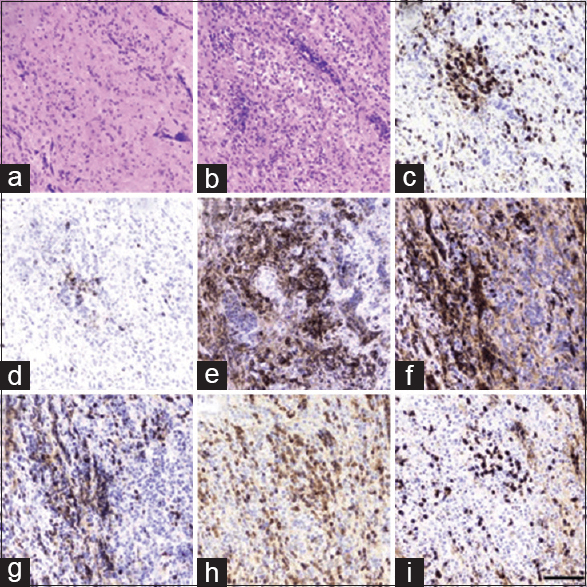
The patient's lymphoma panel was negative. Rather, the final pathology report showed dense mixed lymphoplasmacytic and histiocytic inflammatory infiltrate with marked stromal fibrosis and a large number of IgG4+ plasma cells with an IgG4/IgG ratio of 27% [
Figure 3
Histopathology slides. (a) Hematoxylin and eosin showing mixture of inflammation and fibrosis. (b) Hematoxylin and eosin showing areas of more extensive mononuclear inflammation. (c) CD3, numerous T-cells. (d) CD20, relatively fewer B-cells. (e) CD138, heavy plasma cells. (f) Kappa light chain. (g) Lambda light chain. (h) IgG. (i) Scale bar = 50 microns; IgG4
One-year follow-up
The patient continued to improve clinically. At her 1-year follow-up, she remained clinically asymptomatic without evidence of recurrent disease. Her treatment plan is for continued conservative management. Should her symptoms recur, she would be a candidate for the re-initiation of steroids.
DISCUSSION
Clinical presentation of IgG4-RD
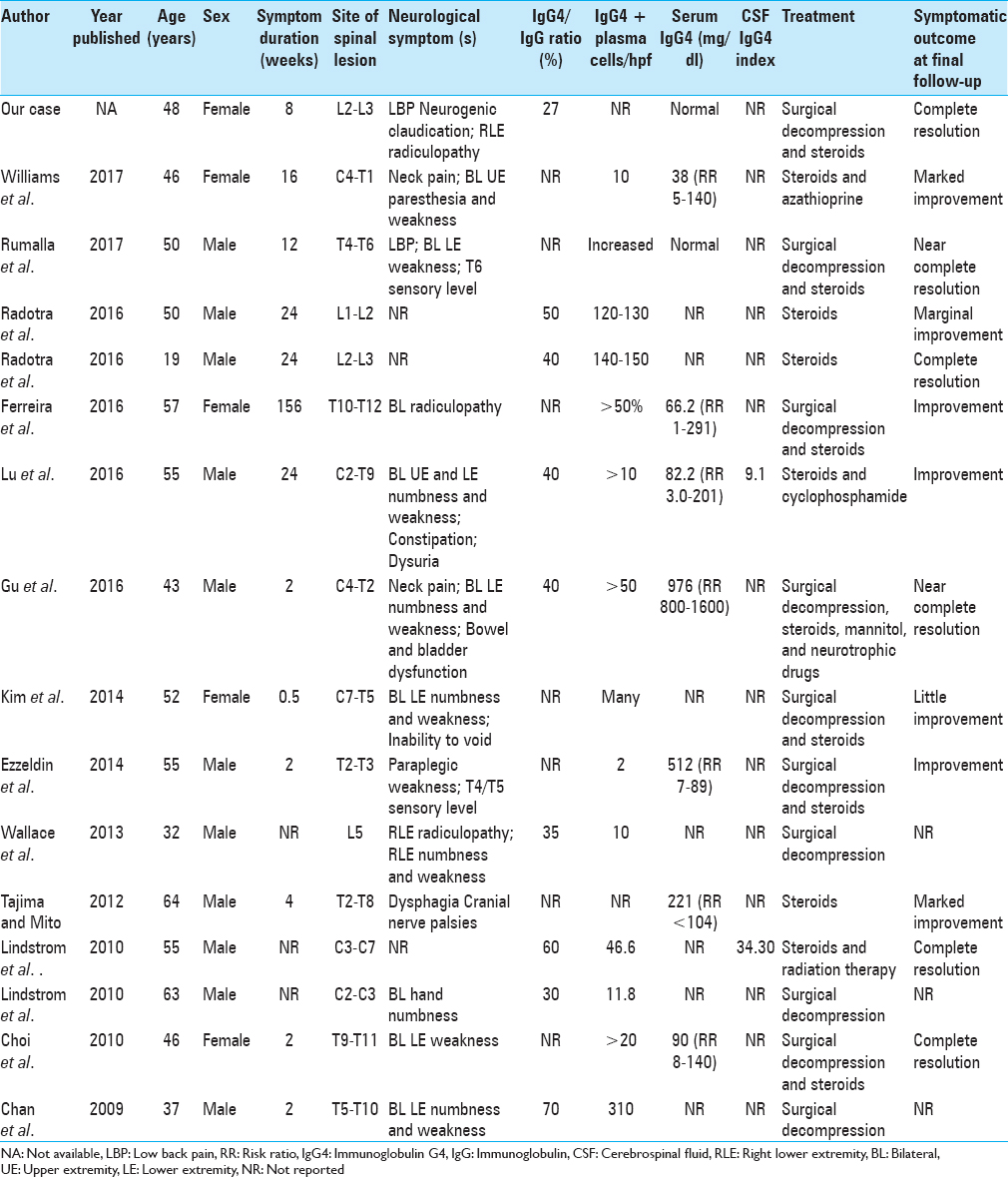
The PubMed database was utilized to identify 15 cases in 13 publications (2000–2017) of IgG4-RD causing spinal cord and/or nerve root compression [
Ratio of IgG4-RD, symptoms, and treatment options
The IgG4/IgG ratio was greater than 40% in 3 of 9 cases (33.3%). Serum IgG4 was elevated in 2 of 9 cases (22.2%). Only 2 cases reported an elevated CSF IgG4 index. Treatment options varied; these included surgical decompression, application of glucocorticoids, and use of immunosuppression therapy. All cases reported improvement in symptoms, with 4 cases reporting complete resolution of symptoms at final follow-up.
Autoimmune IgG4-RD
IgG4-RD is a collection of autoimmune disorders, which have recently been grouped together because of their unique manifestations. IgG4-RD presents in nearly all organ systems but remains rare in the central nervous system.[
Presentation of IgG4-RD in the central nervous system
In the central nervous system, IgG4-RD manifests primarily as hypertrophic pachymeningitis, and may be misdiagnosed as lymphoma given its pseudotumor appearance.[
CSF IgG4 index
Della-Torre et al. utilized a CSF IgG4 index for diagnosing and monitoring patients with IgG4-related pachymeningitis.[
Histopathology and immunohistochemistry of IgG4-RD
Histopathological and immunohistochemical staining from a biopsied specimen showing a lymphoplasmacytic inflammatory infiltrate, fibrosis, and IgG4+ plasma cells remains the gold standard for diagnosing IgG4-RD. Similar to patients with IgG4-RD in other organs, patients with IgG4-related spinal pachymeningitis respond favorably to glucocorticoid treatment, which typically reduces the IgG4-RD pseudotumor mass and controls the inflammatory processes.[
CONCLUSION
Prompt diagnosis and early administration of glucocorticoid treatment may result in the avoidance of surgical decompression in the very rare patients with IgG4-RD spinal tumors.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Brito-Zerón P, Ramos-Casals M, Bosch X, Stone JH. The clinical spectrum of IgG4-related disease. Autoimmun Rev. 2014. 13: 1203-10
2. Chan SK, Cheuk W, Chan KT, Chan JK. IgG4-related sclerosing pachymeningitis: A previously unrecognized form of central nervous system involvement in IgG4-related sclerosing disease. Am J Surg Pathol. 2009. 33: 1249-52
3. Choi SH, Lee SH, Khang SK, Jeon SR. IgG4-related sclerosing pachymeningitis causing spinal cord compression. Neurology. 2010. 75: 1388-90
4. De Virgilio A, de Vincentiis M, Inghilleri M, Fabrini G, Conte M, Gallo A. Idiopathic hypertrophic pachymeningitis: An autoimmune IgG4-related disease. Immunol Res. 2017. 65: 386-94
5. Della-Torre E, Passerini G, Furlan R, Roveri L, Chieffo R, Anzalone N. Cerebrospinal fluid analysis in immunoglobulin G4-related hypertrophic pachymeningitis. J Rheumatol. 2013. 40: 1927-9
6. Deshpande V. IgG4-related disease of the gastrointestinal tract: A 21st century chameleon. Arch Pathol Lab Med. 2015. 139: 742-9
7. Deshpande V, Zen Y, Chan JK, Yi EE, Sato Y, Yoshino T. Consensus statement on the pathology of IgG4-related disease. Mod Pathol. 2012. 25: 1181-92
8. Ezzeldin M, Shawagfeh A, Schnadig V, Smith RG, Fang X. Hypertrophic spinal pachymeningitis: Idiopathic vs. IgG4-related. J Neurol Sci. 2014. 347: 398-400
9. Ferreira NR, Vaz R, Carmona S, Mateus S, Pereira P, Fernandes L. IgG4-related disease presenting with an epidural inflammatory pseudotumor: A case report. J Med Case Rep. 2016. 10: 61-
10. Gu R, Hao PY, Liu JB, Wang ZH, Zhu QS. Cervicothoracic spinal cord compression caused by IgG4-related sclerosing pachymeningitis: A case report and literature review. Eur Spine J. 2016. 25: 147-51
11. Khosroshahi A, Wallace ZS, Crowe JL, Akamizu T, Azumi A, Carruthers MN. International consensus guidance statement on the management and treatment of IgG4-related disease. Arthritis Rheumatol. 2015. 67: 1688-99
12. Kim SH, Kang Y, Oh SH, Paik S, Kim JS. Paraplegia in a patient with IgG4-related sclerosing disease: A case report. Ann Rehabil Med. 2014. 38: 856-60
13. Kosakai A, Ito D, Yamada S, Ideta S, Ota Y, Suzuki N. A case of definite IgG4-related pachymeningitis. Neurology. 2010. 75: 1390-2
14. Lin W, Lu S, Chen H, Wu Q, Fei Y, Li M. Clinical characteristics of immunoglobulin G4-related disease: A prospective study of 118 Chinese patients. Rheumatology (Oxford). 2015. 54: 1982-90
15. Lindstrom KM, Cousar JB, Lopes MB. IgG4-related meningeal disease: Clinico-pathological features and proposal for diagnostic criteria. Acta Neuropathol. 2010. 120: 765-76
16. Lu Z, Tongxi L, Jie L, Yujuan J, Wei J, Xia L. IgG4-related spinal pachymeningitis. Clin Rheumatol. 2016. 35: 1549-53
17. Radotra BD, Aggarwal A, Kapoor A, Singla N, Chatterjee D. An orphan disease: IgG4-related spinal pachymeningitis: Report of 2 cases. J Neurosurg Spine. 2016. 25: 790-4
18. Rumalla K, Smith KA, Arnold PM. Immunoglobulin G4-related epidural inflammatory pseudotumor presenting with pulmonary complications and spinal cord compression: Case report. J Neurosurg Spine. 2017. 26: 688-93
19. Stone JH, Brito-Zerón P, Bosch X, Ramos-Casals M. Diagnostic approach to the complexity of IgG4-related disease. Mayo Clin Proc. 2015. 90: 927-39
20. Stone JH, Zen Y, Deshpande V. IgG4-related disease. N Engl J Med. 2012. 366: 539-51
21. Tajima Y, Mito Y. Cranial neuropathy because of IgG4-related pachymeningitis; intracranial and spinal mass lesions. BMJ Case Rep 2012. 2012. p.
22. Varrassi M, Gianneramo C, Arrigoni F, Cerrone P, Sucapane P, Marini C. Neurological involvement of IgG4-related disease: Description of a case and review of the literature. Neuroradiol J. 2018. 31: 196-202
23. Wallace ZS, Carruthers MN, Khosroshahi A, Carruthers R, Shinagare S, Stemmer-Rachamimov A. IgG4-related disease and hypertrophic pachymeningitis. Medicine (Baltimore). 2013. 92: 206-16
24. Wallace ZS, Deshpande V, Mattoo H, Mahajan VS, Kulikova M, Pillai S. IgG4-related disease: Clinical and laboratory features in one hundred twenty-five patients. Arthritis Rheumatol. 2015. 67: 2466-75
25. Williams MM, Mashaly H, Puduvalli VK, Jin M, Mendel E. Immunoglobulin G4-related disease mimicking an epidural spinal cord tumor: Case report. J Neurosurg Spine. 2017. 26: 76-80