- Division of Neurosurgery, Banner University Medical Center, Tucson, Arizona, USA
- Maine Medical Partners, Neurosurgery and Spine, Scarborough, Maine, USA
Correspondence Address:
Sheri K. Palejwala
Division of Neurosurgery, Banner University Medical Center, Tucson, Arizona, USA
DOI:10.4103/sni.sni_471_16
Copyright: © 2017 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Sheri K. Palejwala, Anand I. Rughani, G. Michael Lemole, Travis M. Dumont. Socioeconomic and regional differences in the treatment of cervical spondylotic myelopathy. 26-May-2017;8:92
How to cite this URL: Sheri K. Palejwala, Anand I. Rughani, G. Michael Lemole, Travis M. Dumont. Socioeconomic and regional differences in the treatment of cervical spondylotic myelopathy. 26-May-2017;8:92. Available from: http://surgicalneurologyint.com/surgicalint-articles/socioeconomic-and-regional-differences-in-the-treatment-of-cervical-spondylotic-myelopathy/
Abstract
Background:Cervical spondylotic myelopathy (CSM) is the leading cause of spinal cord dysfunction in the world. Surgical treatment is both medically and economically advantageous, and can be achieved through multiple approaches, with or without fusion. We used the Nationwide Inpatient Sample (NIS) database to better elucidate regional and socioeconomic variances in the treatment of CSM.
Methods:The NIS database was queried for elective admissions with a primary diagnosis of CSM (ICD-9 721.1). This was evaluated for patients who also carried a diagnosis of anterior (ICD-9 81.02) or posterior cervical fusion (ICD-9 81.03), posterior cervical laminectomy (ICD 03.09), or a combination. We then investigated variances including regional trends and disparities according to hospital and insurance types.
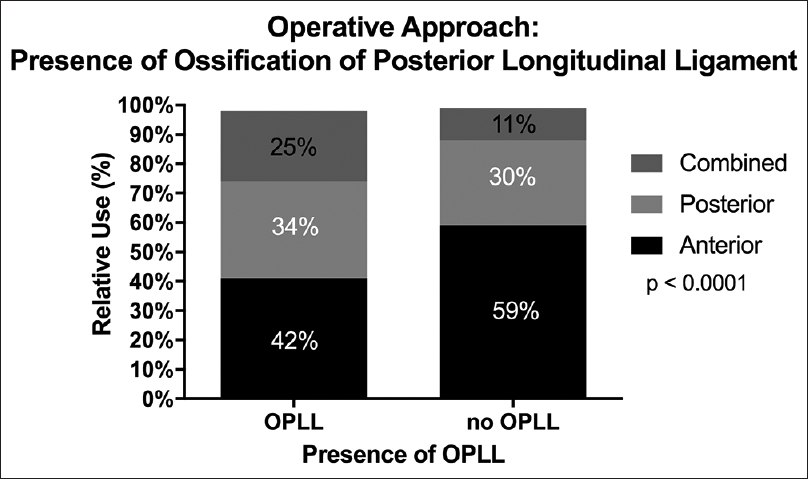
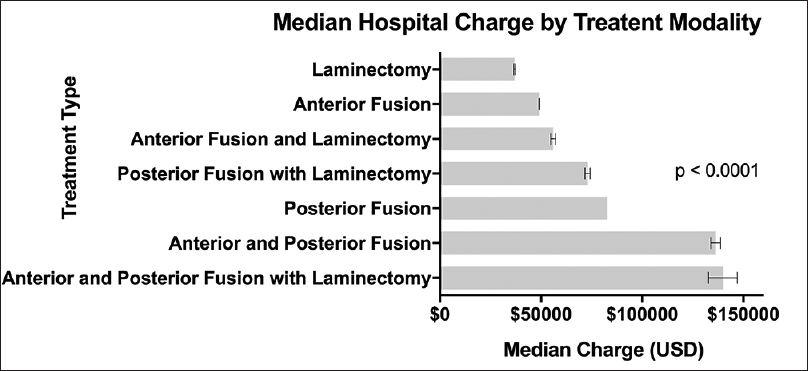
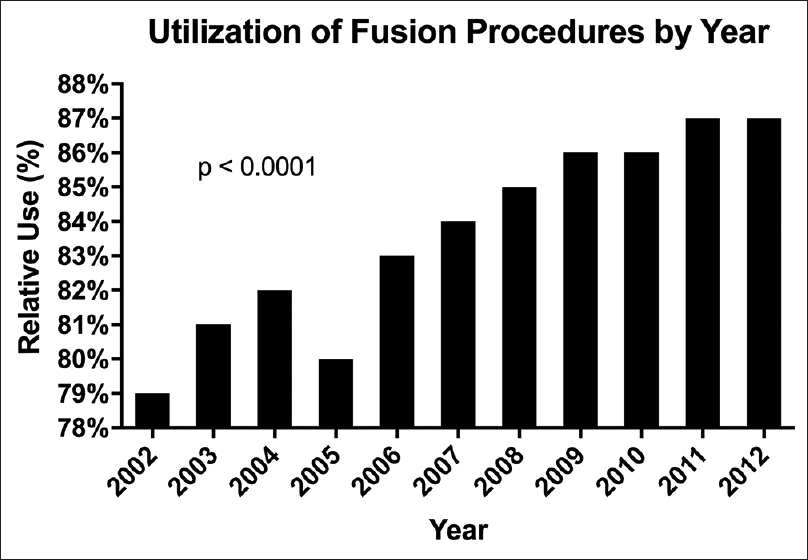
Results:During 2002–2012, 50605 patients were electively admitted with a diagnosis of CSM. Anterior fusions were more common in Midwestern states and in nonteaching hospitals. Fusion procedures were used more frequently than other treatments in private hospitals and with private insurance. Median hospital charges were also expectedly higher for fusion procedures and combined surgical approaches. Combined approaches were found to be significantly greater in patients with concurrent diagnoses of ossification of the posterior longitudinal ligament (OPLL) and CSM. Ultimately, there has been an increased utilization of fusion procedures versus nonfusion treatments, over the past decade, for patients with cervical myelopathy.
Conclusions:Fusion surgery is being increasingly used for the treatment of CSM. Expensive procedures are being performed more frequently in both private hospitals and for those with private insurance, whereas the most economical procedure, posterior cervical laminectomy, was underutilized.
Keywords: Cervical spondylotic myelopathy, disparity, nationwide inpatient sample, regional, spine fusion, socioeconomic
INTRODUCTION
Cervical spondylotic myelopathy (CSM) is the leading cause of spinal cord dysfunction worldwide.[
The surgical treatment options are centered around decompression with or without stability augmentation through fusion. There are multiple surgical approaches for the disease including anterior (anterior cervical discectomy and fusion or corpectomy), posterior (laminectomy, laminectomy and fusion, or laminoplasty), and combined approaches.[
We used the Nationwide Inpatient Sample (NIS), a large, nationwide, multihospital, inpatient database, to evaluate for trends in the surgical techniques used in the treatment of CSM and to elucidate regional or socioeconomic disparities.
MATERIALS AND METHODS
The NIS was queried for elective admissions with a primary diagnosis of CSM (721.1) based on the WHO International Classification of Diseases, Ninth Revision (ICD-9). The years 2002–2012 were assessed because elective admission is a variable which first appeared during this period. A total of 50605 cases were identified. A subset of patients (n = 182, <0.4%) with ossification of the posterior longitudinal ligament (OPLL, ICD-9 723.7) as a secondary diagnosis were separately compared to patients without OPLL. Treatment was stratified based on the type of surgery performed, anterior fusion (ICD-9 81.02), posterior fusion (ICD-9 81.03), laminectomy (ICD 03.09), or combinations of anterior and posterior approaches. Cases with upper cervical fusions and thoracolumbar fusions were eliminated (n = 374, <0.8%). Revision surgeries were not included in the analysis (n = 398, <0.8%). Vague codes such as 80.50-80.51 (discectomy), 80.99 (excision of joint), 81.00 (spinal fusion NOS), 84.51 (insert interbody fusion device), 84.59 (insert spinal device) were excluded from the analysis (n = 445, <0.9%). Cases without procedures performed during admission were eliminated (n = 1302, 2.5%). Because of the infrequent use of disk replacement for this pathology (70 cases, <0.2%), these cases were also eliminated from the analysis. In total, 48016 (95%) of all CSM cases identified were included for the analysis.
The treatment strategy was then compared between different hospital types, primary insurer type, and region were compared with Chi-square statistics and are presented as a percentage of the total cases. Mean hospital charges for each treatment strategy were compared with analysis of variance (ANOVA) and presented in US dollars ± SEM. Statistical analyses were performed using Graphpad Prism (GraphPad Prism version 6.00 for Windows, GraphPad Software, La Jolla California USA,
RESULTS
During 2002–2012, 50605 patients were electively admitted with a primary diagnosis of CSM, and 48016 cases were included for analysis (see above for details). Of these, 7851 (16%) patients had surgery without fusion and 40535 (84%) underwent fusions. In addition, 28465 (59%) had anterior fusions, 14197 (30%) posterior approaches, and 5354 (11%) patients had combined anterior/posterior approaches.
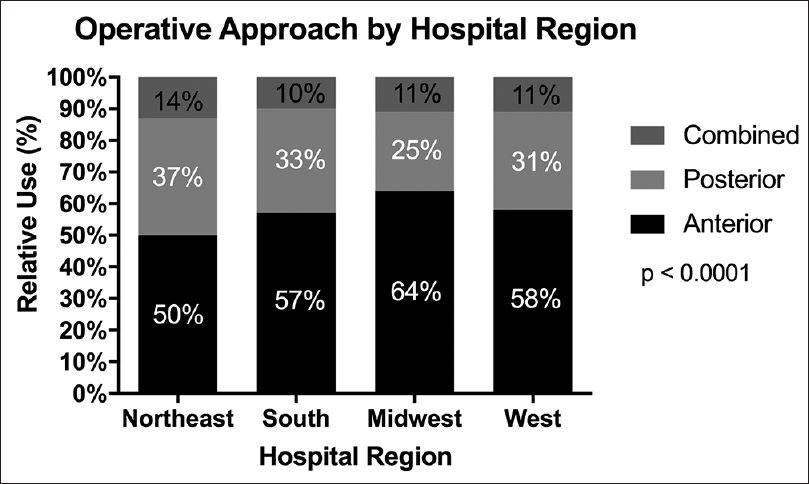
We found that in the Midwest, anterior fusions (64%) were used with relatively greater frequency (P < 0.0001) for the treatment of CSM than that in other regions [
Not surprisingly, hospital charges were greater for posterior fusion surgeries than anterior or nonfusion procedures but were over two and a half times greater for combined anterior-posterior approaches. Fusion procedures were also expectedly associated with higher hospital charges than nonfusion surgeries [
DISCUSSION
CSM is the leading case of spinal cord impairment in the world.[
The natural history of CSM is such that degeneration will progress both over time and exponentially with age. Those with radiographically diagnosed asymptomatic CSM were found to progress to clinical myelopathy at a rate of 8% at 1-year and 23% at 4-year follow-up.[
The efficacy of decompressive surgery for cervical degenerative myelopathy, in terms of both neurologic functional recovery and long-term health-related outcomes, is well established and widely accepted. The ideal approach, though it is doubtful that such a procedure exists, is the subject of much debate.[
Surgery for CSM has increased up to 90% in the United States during 1990–2000 based on a survey of the NIS.[
Consistent with other studies, we found that anterior fusions were the most common cervical surgery performed; however, in our analysis were found to be more frequent in the Midwest as opposed to the South, which was reported in previous studies.[
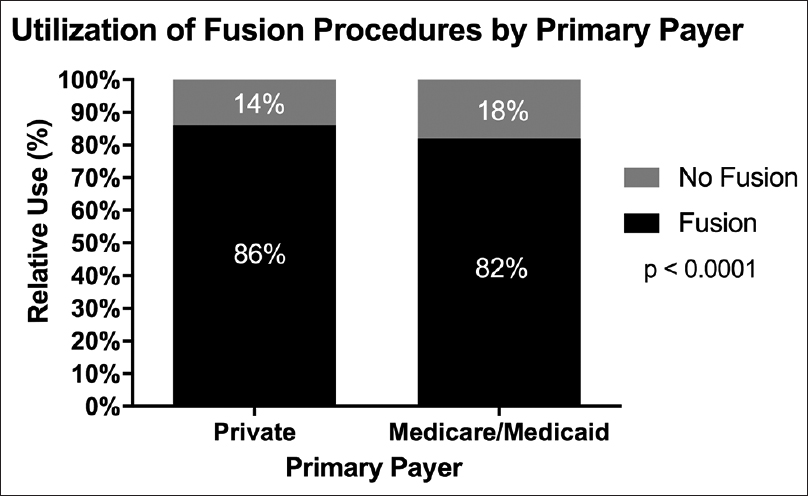
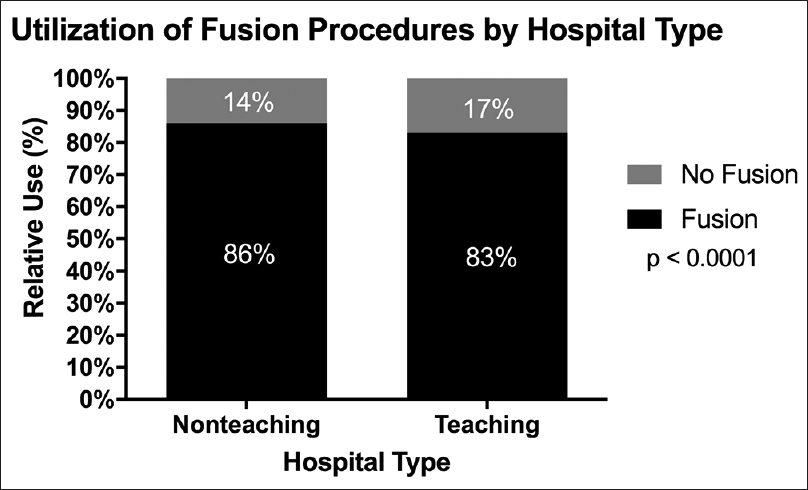
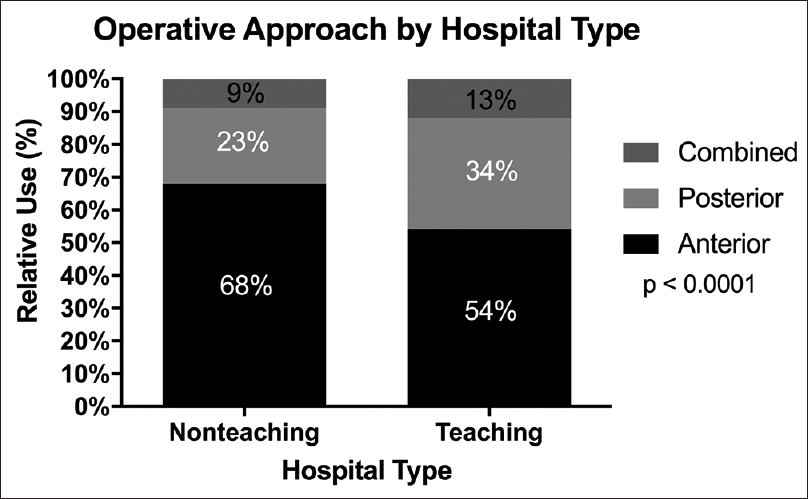
Furthermore, we found that fusion procedures have significantly higher median hospital charges and are more common in nonteaching urban hospitals and in those with private payer insurance. Fusions are costlier procedures that were performed at a greater frequency in private hospitals (86%) than in teaching institutions (83%). Spine fusions are a consistent and leading source of revenue for hospitals, provided patients are adequately insured and hospital charges can be collected. Hospital reimbursement declines, however, with increased complications and readmissions. Of these fusions procedures, anterior fusions were the most commonly performed subtype. Anterior approaches are widely accepted as efficient and well-reimbursed, and in our study were found to be significantly more common in nonteaching institutions than teaching hospitals.[
Fusions were also more common in those with private payer insurance as compared to Medicare or Medicaid. One recent study found that patients with private insurance were 19% more likely to receive an anterior fusion and 17% less likely to receive a posterior-only approach than CMS beneficiaries.[
We also found that posterior cervical laminectomy, the most economical treatment modality for CSM, is underused compared to fusion surgeries, irrespective of the approach. This may be, in part, related to studies showing up to a 21% incidence of post-laminectomy kyphosis within 4 years of posterior cervical laminectomy performed for CSM.[
The benefit of using the NIS database is the ability to examine large volumes of patients across the United States over a large period. Some of the limitations of this study include those inherent to the NIS, including the potential exclusion of those patients who had ambulatory or outpatient surgery. Moreover, additional radiographic and clinical information about individual patients and cases is not available. Based on an administrative database, our findings are dependent on the accurate coding of both diagnoses and procedures.
CONCLUSION
Overall, there is clinical equipoise regarding the surgical approach when treating CSM. There are regional and socioeconomic differences in the utilization of anterior and posterior approaches for the surgical treatment of CSM. The most common approach is an anterior fusion surgery whereas the most economical approach is posterior laminectomy alone, which is also the least used surgical treatment modality.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Alvin MD, Lubelski D, Abdullah KG, Whitmore RG, Benzel EC, Mroz TE. Cost-utility analysis of anterior cervical discectomy and fusion with plating (ACDFP) versus posterior cervical foraminotomy (PCF) for patients with single-level cervical radiculopathy. Spine J. 2013. 13: 120S-1
2. Baptiste DC, Fehlings MG. Pathophysiology of cervical myelopathy. Spine J. 2006. 6: 190S-7
3. Boogaarts HD, Bartels RHM. Prevalence of cervical spondylotic myelopathy. Eur Spine J. 2013. 24: 139-41
4. David Kaye I, Marascalchi BJ, Macagno AE, Lafage VA, Bendo JA, Passias PG. Predictors of morbidity and mortality among patients with cervical spondylotic myelopathy treated surgically. Eur Spine J. 2015. 24: 2910-7
5. Fehlings MG, Jha NK, Hewson SM, Massicotte EM, Kopjar B, Kalsi-Ryan S. Is surgery for cervical spondylotic myelopathy cost-effective? A cost-utility analysis based on data from the AOSpine North America prospective CSM study. J Neurosurg Spine. 2012. 17: 89-93
6. Fehlings MG, Tetreault L, Wilson JR, Skelly AC. Cervical spondylotic myelopathy: Current state of the art and future directions. Spine. 2013. 38: S1-8
7. Fehlings MG, Wilson JR, Kopjar B, Yoon ST, Arnold PM, Massicotte EM. Efficacy and Safety of Surgical Decompression in Patients with Cervical Spondylotic Myelopathy. J bone Jt Surg Am. 2013. 95: 1651-
8. Fehlings MG, Wilson JR, Yoon ST, Rhee JM, Shamji MF, Lawrence BD. Symptomatic progression of cervical myelopathy and the role of nonsurgical management: A consensus statement. Spine. 2013. 38: S19-20
9. Fineberg SJ, Oglesby M, Patel A, Pelton M, Singh K. Outcomes of cervical spine surgery in teaching and non-teaching hospitals. Spine. 2013. 38: 1089-96
10. Ghogawala Z, Benzel EC, Heary RF, Riew KD, Albert TJ, Butler WE. Cervical spondylotic myelopathy surgical trial: Randomized, controlled trial design and rationale. Neurosurgery. 2014. 75: 334-46
11. Kalsi-Ryan S, Singh A, Massicotte EM, Arnold PM, Brodke DS, Norvell DC. Ancillary outcome measures for assessment of individuals with cervical spondylotic myelopathy. Spine. 2013. 38: S111-22
12. Kaptain GJ, Simmons NE, Replogle RE, Pobereskin L. Incidence and outcome of kyphotic deformity following laminectomy for cervical spondylotic myelopathy. J Neurosurg. 2000. 93: 199-204
13. Karadimas SK, Erwin WM, Ely CG, Dettori JR, Fehlings MG. Pathophysiology and natural history of cervical spondylotic myelopathy. Spine. 2013. 38: S21-36
14. Lawrence BD, Jacobs WB, Norvell DC, Hermsmeyer JT, Chapman JR, Brodke DS. Anterior versus posterior approach for treatment of cervical spondylotic myelopathy: A systematic review. Spine. 2013. 38: S173-82
15. Lawrence BD, Shamji MF, Traynelis VC, Yoon ST, Rhee JM, Chapman JR. Surgical management of degenerative cervical myelopathy: A consensus statement. Spine. 2013. 38: S171-2
16. McClelland III S, Marascalchi BJ, Passias PG, Protopsaltis TS, Frempong-Boadu AK, Errico TJ. Impact of Race and Insurance Status on Surgical Approach for Cervical Spondylotic Myelopathy in the United States: A Population-Based Analysis. Spine. 2016. p.
17. Menger RP, Wolf ME, Kukreja S, Sin A, Nanda A. Medicare payment data for spine reimbursement; important but flawed data for evaluating utilization of resources. Surg Neurol Int. 2015. 6: S391-7
18. Molina CA, Zadnik PL, Gokaslan ZL, Witham TF, Bydon A, Wolinsky JP. A cohort cost analysis of lumbar laminectomy - Current trends in surgeon and hospital fees distribution. Spine J. 2013. 13: 1434-7
19. Patil PG, Turner D, Pietrobon R. National trends in surgical procedures for degenerative cervical spine disease: 1990-2000. Neurosurgery. 2005. 57: 753-8
20. Rao R. Neck pain, cervical radiculopathy, and cervical myelopathy: Pathophysiology, natural history, and clinical evaluation. Instr Course Lect. 2002. 52: 479-88
21. Shamji MF, Cook C, Pietrobon R, Tackett S, Brown C, Isaacs RE. Impact of surgical approach on complications and resource utilization of cervical spine fusion: A nationwide perspective to the surgical treatment of diffuse cervical spondylosis. Spine J. 2009. 9: 31-8
22. Shamji MF, Cook C, Tackett S, Brown C, Isaacs RE. Impact of preoperative neurological status on perioperative morbidity associated with anterior and posterior cervical fusion. J Neurosurg Spine. 2008. 9: 10-6
23. Shamji MF, Massicotte EM, Traynelis VC, Norvell DC, Hermsmeyer JT, Fehlings MG. Comparison of anterior surgical options for the treatment of multilevel cervical spondylotic myelopathy: A systematic review. Spine. 2013. 38: S195-209
24. Wang MC, Kreuter W, Wolfla CE, Maiman DJ, Deyo R. Trends and variations in cervical spine surgery in the United States: Medicare beneficiaries, 1992 to 2005. Spine. 2009. 34: 955-61