- Department of Neurosurgery, Hospital Alemão Oswaldo Cruz, São Paulo-Brazil
- Department of Neurosurgery, DFV Neuro, São Paulo-Brazil
- Department of Neurosurgery, Hospital Sírio Libanês, São Paulo-Brazil
Correspondence Address:
Matheus Fernandes de Oliveira
Department of Neurosurgery, Hospital Alemão Oswaldo Cruz, São Paulo-Brazil
Department of Neurosurgery, DFV Neuro, São Paulo-Brazil
Department of Neurosurgery, Hospital Sírio Libanês, São Paulo-Brazil
DOI:10.25259/SNI-127-2019
Copyright: © 2019 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Henrique Oliveira Martins, Roger Schmidt Brock, Mario Augusto Taricco, José Francisco Pereira Júnior, Matheus Fernandes de Oliveira. Sporadic hemangioblastoma of cauda equina: An atypical case report. 24-Apr-2019;10:60
How to cite this URL: Henrique Oliveira Martins, Roger Schmidt Brock, Mario Augusto Taricco, José Francisco Pereira Júnior, Matheus Fernandes de Oliveira. Sporadic hemangioblastoma of cauda equina: An atypical case report. 24-Apr-2019;10:60. Available from: http://surgicalneurologyint.com/surgicalint-articles/9294/
Abstract
Background:Hemangioblastomas account for about 1%–3% of all central nervous system tumors. They are usually associated with the Von Hippel–Lindau syndrome and typically occur in the posterior fossa, or throughout the spinal neuraxis. Here, we report the unusual case of a sporadic cauda equina hemangioblastoma.
Case Description:A 28-year-old Caucasian female patient presented with progressive low back pain of 2 months duration. The magnetic resonance (MR) revealed a heterogeneous intradural and extramedullary lesion at the L2 level; with intravenous contrast, there were vascular flow voids and surrounding vasogenic edema (i.e., measuring 4.1 cm × 3.5 cm). The patient underwent an L2 right hemilaminectomy under intraoperative neurophysiological monitoring. She was discharged the 4th postoperative day, neurologically intact. Literature describes 21 previous reports of sporadic isolated spinal hemangioblastomas.
Conclusion:Although rare, sporadic, and isolated hemangioblastomas of the cauda equina should be included among the differential diagnoses of intradural spinal lesions, particularly when enhanced MR studies document serpentine flow voids.
Keywords: Cauda equina, pathology, spinal cord neoplasm, treatment
INTRODUCTION
Hemangioblastomas account for about 1%–3% of all central nervous system tumors.[
CASE DESCRIPTION
A 28-year-old Caucasian female presented with progressive low back pain of 2 months duration. She had no significant medical history and exhibited no focal neurological deficits. The magnetic resonance imaging (MRI) of the lumbar spine revealed a heterogeneous intradural/extramedullary lesion at the L2 level (measuring 4.1 cm × 3.5 cm) that enhanced with contrast. Flow voids were also demonstrated along with surrounding vasogenic edema [
Surgery
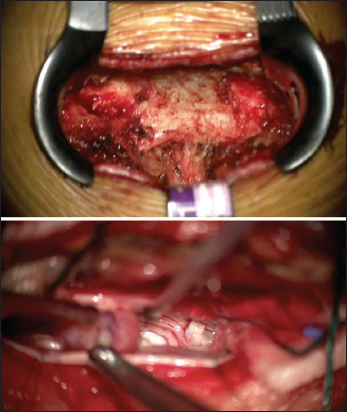
An L2 right hemilaminectomy was performed utilizing intraoperative neuromonitoring [
Pathology
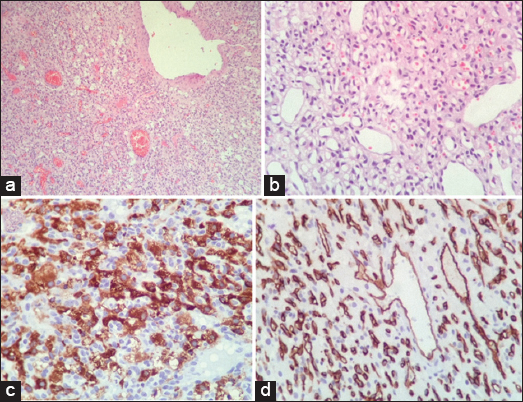
Hematoxylin and eosin stains revealed a highly vascular and cellular tumor [
DISCUSSION
Isolated tumors of the cauda equina represent 10% of all spinal canal lesions and typically include schwannomas, meningiomas, or ependymomas. Hemangioblastomas appear isointense on T1 and hyperintense on T2 MRI scans and/or heterogeneous hyperintensity on T2 studies secondary to flow voids attributed to their high vascularity (e.g., serpentine/tortuous/convoluted vessels).[
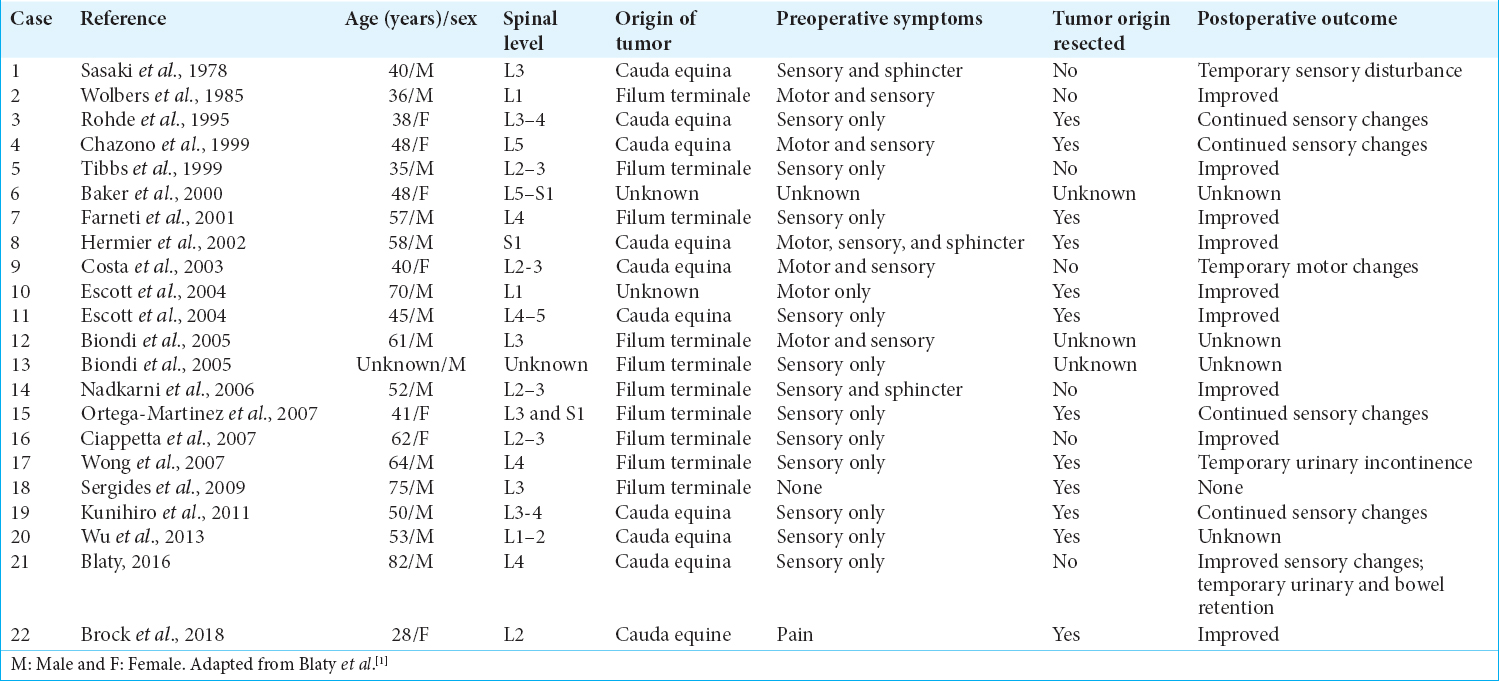
For the total of 22 cases of filum terminal hemangioblastomas (e.g., including this case), patients averaged 51 years of age [
Surgical resection of these lesions is considered safe and effective with low accompanying complication/morbidity rates (e.g., few significant postoperative neurological deficits).
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient has given her consent for her images and other clinical information to be reported in the journal.
Financial support and sponsorship
Nil.
Conflicts of interest
The authors declare no conflicts of interest.
References
1. Blaty D, Malos M, Palmrose T, McGirr S. Sporadic intradural extramedullary hemangioblastoma of the cauda equina:Case report and literature review. World Neurosurg. 2018. 109: 436-41
2. Kunihiro N, Takami T, Yamagata T, Tsuyuguchi N, Ohata K. Spinal hemangioblastoma of cauda equina origin not associated with von hippel-lindau syndrome case report. Neurol Med Chir (Tokyo). 2011. 51: 732-5
3. Lonser RR, Butman JA, Huntoon K, Asthagiri AR, Wu T, Bakhtian KD. Prospective natural history study of central nervous system hemangioblastomas in von hippel-lindau disease. J Neurosurg. 2014. 120: 1055-62
4. Mehta GU, Montgomery BK, Maggio DM, Chittiboina P, Oldfield EH, Lonser RR. Functional outcome after resection of von hippel-lindau disease-associated cauda equina hemangioblastomas:An observational cohort study. Oper Neurosurg (Hagerstown). 2017. 13: 435-40
5. Wu L, Yang T, Deng X, Xu Y. Intra-extradural dumbbell-shaped hemangioblastoma of the cauda equina mimicking schwannoma. Neurol India. 2013. 61: 338-9