- David Geffen School of Medicine at UCLA, Los Angeles, California, USA
- Department of Neurosurgery, David Geffen School of Medicine at UCLA, Los Angeles, California, USA
- Department of Neurosurgery, Kaiser Permanente Medical Center, Los Angeles, California, USA
Correspondence Address:
Daniel Diaz-Aguilar
Department of Neurosurgery, Kaiser Permanente Medical Center, Los Angeles, California, USA
DOI:10.4103/sni.sni_225_17
Copyright: © 2017 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Daniel Diaz-Aguilar, Sergei Terterov, Rudi Scharnweber, Harsimran Brara, Alex Tucker, Catherine Merna, Stephanie Wang, Shayan Rahman. Surgical nuances of circumferential lumbar spondylectomy: A case report and short literature review. 24-Oct-2017;8:253
How to cite this URL: Daniel Diaz-Aguilar, Sergei Terterov, Rudi Scharnweber, Harsimran Brara, Alex Tucker, Catherine Merna, Stephanie Wang, Shayan Rahman. Surgical nuances of circumferential lumbar spondylectomy: A case report and short literature review. 24-Oct-2017;8:253. Available from: http://surgicalneurologyint.com/surgicalint-articles/surgical-nuances-of-circumferential-lumbar-spondylectomy-a-case-report-and-short-literature-review/
Abstract
Background:Chordomas are uncommon malignant bone tumors that are often minimally symptomatic for several years. By the time they are diagnosed, these lesions are typically large, involve major neural, bony, and vascular structures, and are no longer readily resectable. This leads to a high recurrence rate.
Case Description:In this case report, we present a 67-year-old male with nonmechanical axial back pain, neurogenic claudication, and a large mass centered at the L3 level on magnetic resonance imaging consistent with a locally invasive chordoma. The patient underwent surgical resection that required a complete lumbar spondylectomy utilizing a three-stage approach, leading to incomplete tumor excision. The patient's residual postoperative symptoms included paresthesias/numbness in the right anterior thigh and a partial (4/5) right-sided foot drop. At the time of discharge, there were plans for future proton beam therapy.
Conclusions:Because of their relative resistance to chemotherapeutic agents, the optimal surgical management of chordomas is gross total en-bloc excision. Unfortunately, this is rarely feasible.
Keywords: Adult chordoma, lumbar spondylectomy, treatment of chordoma
INTRODUCTION
Chordomas are rare, locally aggressive malignant bone tumor. Such tumors only account for only 1–4% of all primary bone tumors. Their treatment is complicated by frequent close proximity and frequent involvement of critical neurovascular structures.[
CASE DESCRIPTION
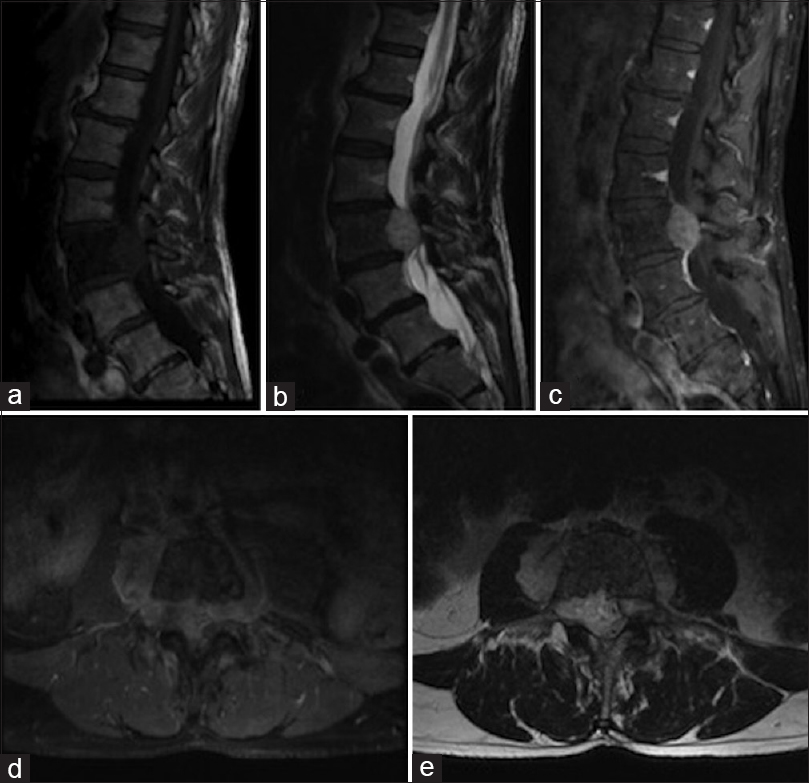
A 67-year-old male presented with nonmechanical axial back pain, neurogenic claudication, and an otherwise normal neurological exam. Established T1 (hypointense), T2 (hyperintense), and T1 enhanced magnetic resonance (MR) studies documented a large tumor centered at the L3 level with marked epidural compression and bilateral retroperitoneal extension [
Figure 1
Sagittal MR T1-weighted, T2-weighted (a) T1-fat saturated post contrast (b), axial T1-post gadolinium (c), and axial T2-weighted (d) images demonstrating a T1 hypointense, T2 hyperintense enhancing mass centered in the L3 vertebral body with significant epidural and retroperitoneal extension and decreased marrow signal in L3 vertebral body (e)
L3 spondylectomy technique
Following confirmation of a chordoma by needle biopsy, our patient underwent a three-stage operation for complete resection.
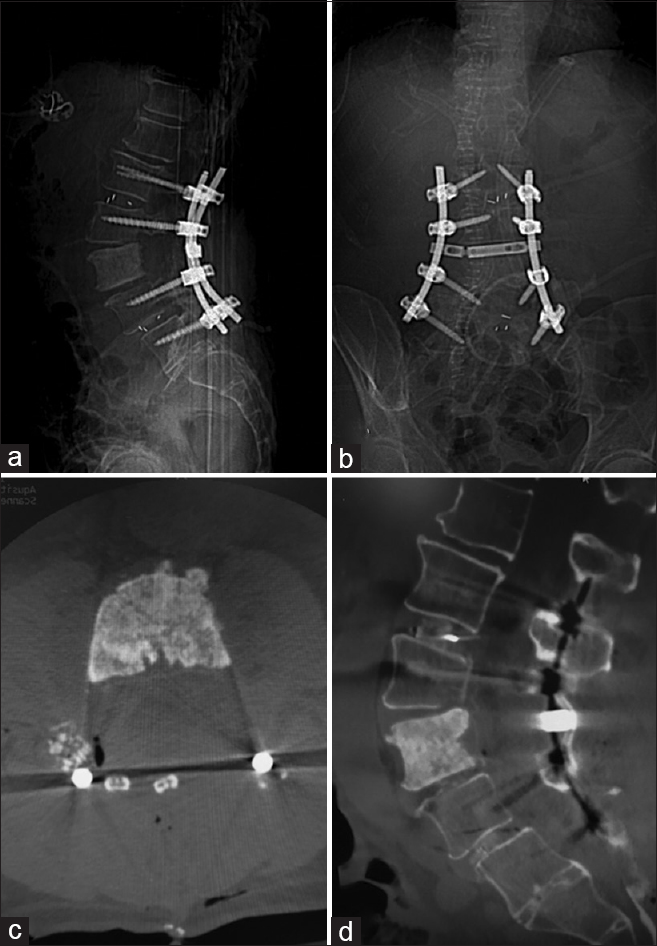
Stage I – posterior approach
Following a midline exposure from T12 to L5, the pedicles of L1, L2, L4, and L5 were instrumented bilaterally. Transforaminal interbody grafts were placed at L1/2 and L4/5. A massive en-bloc resection of the tumor required bilateral troughs in the L3 pars extending to the superior lamina, and included L2/3 bilateral facetectomies and transverse process resections. Pedicle screws were then connected with two rods and a crosslink [
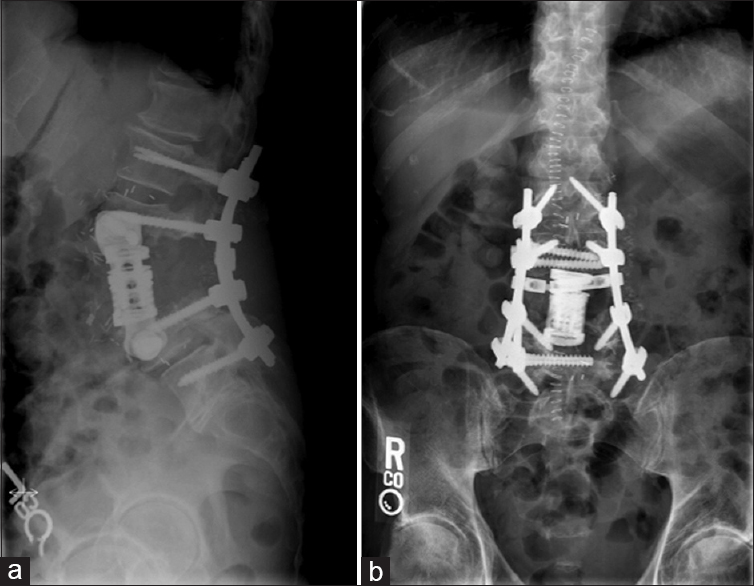
Stage II/III – anterolateral approach
The vascular surgery team performed a retroperitoneal approach to the anterolateral lumbar spine on both the right and left sides respectively. The ribs of T11 and T12 were taken, the psoas muscle was mobilized, and the anterolateral disc spaces of L2/3 and L3/4 were exposed allowing retroperitoneal tumor resection utilizing annulotomies and diskectomies [
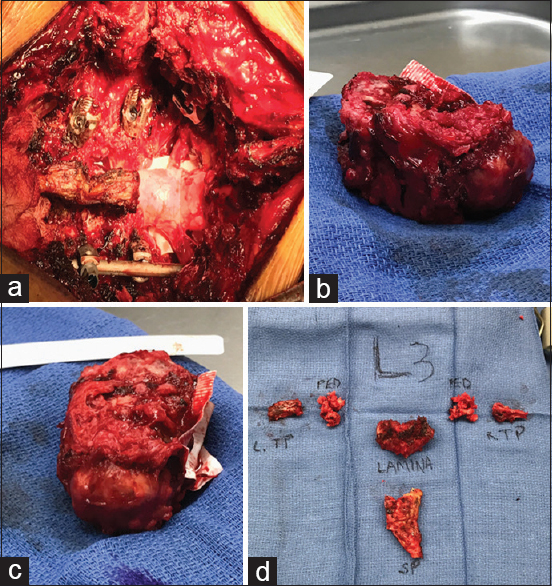
Figure 3
Surgical view after posterior element removal. Bilateral L2 and L3 nerve roots are visualized (a). Ventral epidural Gortex patch. Anterior view of the removed L3 vertebral body with attached left sided tumor (b). Lateral view of the removed L3 vertebral body with attached left sided tumor and ventral epidural gortex patch (c). Removed posterior elements (d)
Postoperative course
Postoperatively, the patient only had mild paresthesias and numbness of the right anterior thigh accompanied by a partial 4/5 dorsiflexion deficit; symptoms/signs resolved prior to transfer to a rehabilitation center. The histological examination of the en-bloc specimen confirmed tumor excision along with 1 of 3 lymph nodes that was positive for chordoma. Subsequent plans were made for future proton beam therapy.
DISCUSSION
Chordomas are slow growing but aggressive tumors that demonstrate a high incidence of local recurrence. The surgical goal for chordomas is centered on total en-bloc resection with canal decompression and spinal reconstruction as needed.[
However, en-bloc spondylectomy is often not technically feasible due to surrounding critical neural and vascular structures.[
CONCLUSION
Lumbar chordomas are locally invasive, indolent tumors, requiring aggressive surgical resection. Mortality rates are high and long-term survival correlates with early diagnosis and the extent of surgical resection.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Boriani S, Bandiera S, Donthineni R, Amendola L, Cappuccio M, De Iure F. Morbidity of en bloc resections in the spine. Eur Spine J. 2010. 19: 231-41
2. Chugh R, Tawbi H, Lucas DR, Biermann JS, Schuetze SM, Baker LH. Chordoma: The nonsarcoma primary bone tumor. Oncologist. 2007. 12: 1344-50
3. Guppy KH, Chakrabarti I, Isaacs RS, Jun JH. En bloc resection of a multilevel high-cervical chordoma involving C-2: New operative modalities: Technical note. J Neurosurg Spine. 2013. 19: 232-42
4. Hatem MA. Lumbar spine chordoma. Radiol Case Rep. 2014. 9: 940-
5. Smoll NR, Gautschi OP, Radovanovic I, Schaller K, Weber DC. Incidence and relative survival of chordomas: The standardized mortality ratio and the impact of chordomas on a population. Cancer. 2013. 119: 2029-37
6. Stephens GC, Schwartz HS. Lumbosacral chordoma resection: Image integration and surgical planning. J Surg Oncol. 1993. 54: 226-32