- Department of Nuclear Medicine, St. Vincent's Hospital, Darlinghurst, Australia
- Faculty of Medicine, University of Sydney, Camperdown, New South Wales, Australia
Correspondence Address:
Bi Yi Chen
Faculty of Medicine, University of Sydney, Camperdown, New South Wales, Australia
DOI:10.4103/sni.sni_91_18
Copyright: © 2018 Surgical Neurology International This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.How to cite this article: Charlotte Yin, Bi Yi Chen. Tension pneumocephalus from skull base surgery: A case report and review of the literature. 04-Jul-2018;9:128
How to cite this URL: Charlotte Yin, Bi Yi Chen. Tension pneumocephalus from skull base surgery: A case report and review of the literature. 04-Jul-2018;9:128. Available from: http://surgicalneurologyint.com/surgicalint-articles/tension-pneumocephalus-from-skull-base-surgery-a-case-report-and-review-of-the-literature/
Abstract
Background:Tension pneumocephalus from skull base surgery is a rare occurrence that mandates urgent neurosurgical attention.
Case Description:We describe a case of tension pneumocephalus secondary to an endoscopic endonasal resection of an adamantinomatous craniopharyngioma and how it was successfully managed at our institution.
Conclusion:Our experience reflects that definitive treatment of tension pneumocephalus is required with multilayered dural repair, but temporising measures should be used immediately to prevent neurological deterioration prior to the definitive repair.
Keywords: Dural repair, skull base surgery, tension pneumocephalus
BACKGROUND
Tension pneumocephalus (TP) is a rare complication of skull base surgery and can lead to rapid neurological deterioration. Significant amounts of intracranial air can compress and displace the intracranial structures, necessitating urgent decompression. While options exist for the management of TP, the treatments are only described in case reports or case series. We report here a case of TP secondary to an endoscopic endonasal resection of an adamantinomatous craniopharyngioma, and how it was managed successfully at our institution. We hope to use the information learnt from this case, in combination with a review of the literature, to create a guide for the management of TP secondary to skull base surgery.
CASE REPORT
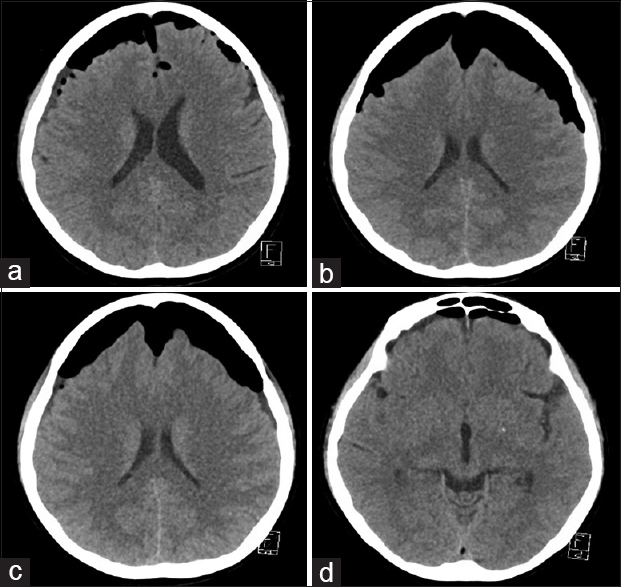
The patient is a 57-year-old female who presented with 5 months of progressively worsening visual acuity and diabetes insipidus. Magnetic resonance imaging (MRI) showed a heterogeneous rim-enhancing 17 × 13 × 25 mm suprasellar lesion. The patient has no significant medical comorbidities. An endoscopic endonasal resection of the lesion was performed. DURAFOAM dural graft implant was used to close the dura and a nasoseptal flap was placed over the defect. The lesion was confirmed on pathology to be an adamantinomatous craniopharyngioma. Day 1 postoperative computed tomography of the brain (CTB) showed a small bifrontal pneumocephalus [
A transnasal transphenoidal repair of the dural defect was performed. Dural substitute was removed and a fascia lata graft inlay was used to repair the defect. However, the negative intracranial pressure drew the fascia lata graft intradurally. A fascia lata onlay graft with autologous blood patch was then used and the nasoseptal flap was replaced and secured with a TISSEEL fibrin sealant. Ten hours after the operation, the patient's GCS dropped to 11 (M6V1E4) and CTB again showed re-accumulation of the pneumocephalus. Percutaneous aspiration was performed and the patient returned to her neurological baseline.
Three days after the last percutaneous aspiration, rhinorrhoea was again observed. This was followed 2 days later by another episode of GCS reduction to 13 (M6V3E4) with diplegia. CTB showed an expanding anterior pneumocephalus with mass effect. Percutaneous aspiration was performed with GCS recovery. The following day, GCS dropped to 9 (M6V2E1), and percutaneous aspiration was again performed for improvement in GCS. An endoscopic repair of the CSF leak was performed. During the operation, a leak was found between the leaflets of the previous fascia lata repair. A fat bath plug was placed over the defect with a large single piece of fascia overlaid. The repair was then tested with Valsalva three times. The nasoseptal flap was overlaid and augmented with a left inferior turbinate free mucosal graft. Postoperative CTB showed a significant reduction in the size of the pneumocephalus [
DISCUSSION
Pneumocephalus is the presence of air or gas within the cranial vault usually as a result of a breach in the craniodural barrier. It is thus a common entity following neurosurgical intervention with a predominantly clinically benign course and expectant management.[
There are two proposed mechanisms for the development of TP. The first is a “ball-valve” mechanism that allows air to enter but not exit the cranial vault through a defect during a cough or sneeze. The second is the “inverted pop bottle” mechanism whereby the air enters the intracranial compartment to equalize the pressure differential as cerebrospinal fluid (CSF) exits through the defect.[
A wide range of temporising measures for TP have been described. Conservative approaches include bed rest, raising the bed head, hyperosmolar therapy, and abstaining from Valsalva or similar manoeuvres.[
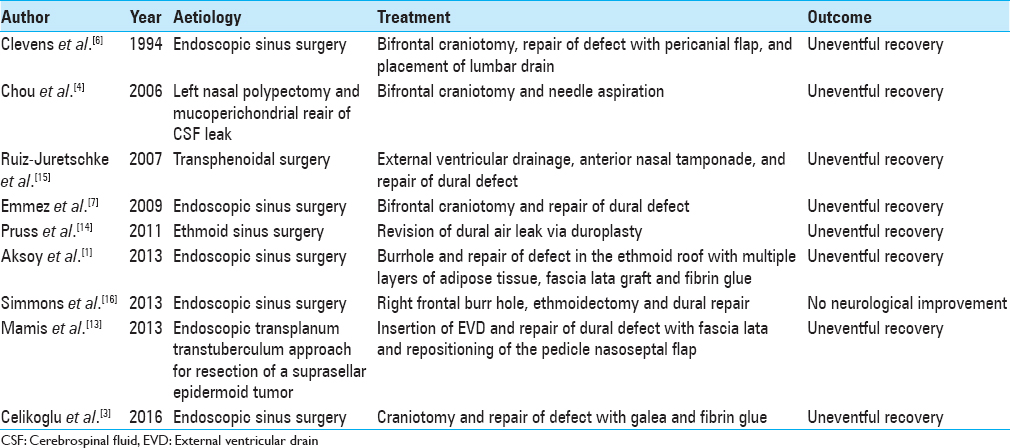
From the results of the literature review shown in
Another learning point from our case was the use of the Valsalva manoeuvre intraoperatively following closure of the dural defect to check for CSF leakage. This was not performed during the first operation which was unsuccessful in treating the pneumocephalus, but was performed in the second operation during which the dural defect was successfully closed. Theoretically, Valsalva expels intrathoracic blood to cause an increase in intracerebral pressure (ICP) which promotes spillage of CSF from the intracranial compartment if a dural defect exists.[
TP secondary to skull base surgery is a rare complication that can be accompanied by acute neurological deterioration. The definitive treatment of TP is dural repair, but temporising measures should be used to prevent neurological deterioration prior to the definitive repair. Dural repair should be performed using a multilayered approach with consolidation from fibrin glue, and the Valsalva manoeuvrer should be performed at the end of the repair to assess its integrity.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Funding
No funding was received for this research.
Compliance with ethical standards
Conflicts of interest
There are no conflicts of interest to disclose.
Informed consent Informed consent was obtained from the patient.
References
1. Aksoy F, Dogan R, Ozturan O, Tugrul S, Yildirim YS. Tension pneumocephalus: an extremely small defect leading to an extremely serious problem. Am J Otolaryngol. 2013. 34: 749-52
2. Babl FE, Arnett AM, Barnett E, Brancato JC, Kharasch SJ, Janecka IP. Atraumatic pneumocephalus: A case report and review of the literature. Pediatr Emerg Care. 1999. 15: 106-9
3. Celikoglu E, Hazneci J, Ramazanoglu AF. Tension pneumocephalus causing brain herniation after endoscopic sinus surgery. Asian J Neurosurg. 2016. 11: 309-10
4. Chou S, Ning M, Buonanno F. Focal intraparenchymal tension pneumocephalus. Neurology. 2006. 67: 1485-
5. Church CA, Chiu AG, Vaughan WC. Endoscopic repair of large skull base defects after powered sinus surgery. Otolaryngol Head Neck Surg. 2003. 129: 204-9
6. Clevens RA, Bradford CR, Wolf GT. Tension pneumocephalus after endoscopic sinus surgery. Ann Otol Rhinol Laryngol. 1994. 103: 235-7
7. Emmez H, Durdag E, Uslu S, Pasaoglu A, Ceviker N. Intracerebral tension pneumocephalus complicating endoscopic sinus surgery: Case report. Acta Neurochir (Wien). 2009. 151: 1001-2
8. Goldmann RW. Pneumocephalus as a consequence of barotrauma. JAMA. 1986. 255: 3154-6
9. Haldar R, Khandelwal A, Gupta D, Srivastava S, Rastogi A, Singh PK. Valsalva maneuver: Its implications in clinical neurosurgery. Neurol India. 2016. 64: 1276-80
10. Hong B, Biertz F, Raab P, Scheinichen D, Ertl P, Grosshennig A. Normobaric hyperoxia for treatment of pneumocephalus after posterior fossa surgery in the semisitting position: A prospective randomized controlled trial. PLoS One. 2015. 10: e0125710-
11. Horowitz M. Intracranial Pneumocoele. An Unusual Complication Following Mastoid Surgery. J Laryngol Otol. 1964. 78: 128-34
12. Klein J. Normobaric pulmonary oxygen toxicity. Anesth Analg. 1990. 70: 195-207
13. Mammis A, Agarwal N, Eloy JA, Liu JK. Intraventricular tension pneumocephalus after endoscopic skull base surgery. J Neurol Surg A Cent Eur Neurosurg. 2013. 74: e96-99
14. Pruss H, Klingebiel R, Endres M. Tension pneumocephalus with diplegia and deterioration of consciousness. Case Rep Neurol. 2011. 3: 48-9
15. Ruiz-Juretschke F, Mateo-Sierra O, Iza-Vallejo B, Carrillo-Yague R. Intraventricular tension pneumocephalus after transsphenoidal surgery: A case report and literature review. Neurocirugia (Astur). 2007. 18: 134-7
16. Simmons J, Luks AM. Tension pneumocephalus: An uncommon cause of altered mental status. J Emerg Med. 2013. 44: 340-3
17. Sweni S, Senthilkumaran S, Balamurugan N, Thirumalaikolundusubramanian P. Tension pneumocephalus: A case report with review of literature. Emerg Radiol. 2013. 20: 573-8