- Department of Neurosurgery, Walter Reed National Military Medical Center, Bethesda, United States
- Department of Vascular Neurosurgery, Piedmont Hospital, Atlanta, Georgia, United States.
- Department of Vascular Surgery, Piedmont Hospital, Atlanta, Georgia, United States.
Correspondence Address:
Jason H Boulter, Department of Neurosurgery, Walter Reed National Military Medical Center, Bethesda, United States.
DOI:10.25259/SNI_71_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Jason H Boulter1, Michael F. Stiefel2, Eyal Ben-Aire3, Albert J. Schuette2. Thrombectomy and stenting of pseudoaneurysm from transcarotid artery revascularization. 12-Apr-2024;15:127
How to cite this URL: Jason H Boulter1, Michael F. Stiefel2, Eyal Ben-Aire3, Albert J. Schuette2. Thrombectomy and stenting of pseudoaneurysm from transcarotid artery revascularization. 12-Apr-2024;15:127. Available from: https://surgicalneurologyint.com/surgicalint-articles/12855/
Abstract
Background: Transcarotid artery revascularization (TCAR) is becoming an increasingly popular treatment of carotid stenosis. Despite this rapid adoption, little in the literature describes the associated complications of this procedure.
Case Description: We report a case of a left M1 large-vessel occlusion following treatment of symptomatic, high-grade carotid stenosis with a TCAR procedure approximately three weeks earlier. The initial angiography demonstrated a pseudoaneurysm in the left common carotid artery at the site of TCAR access with a distal clot in the carotid stent. The clot within the stent was aspirated, and a mechanical thrombectomy was performed with a combination of a stent-retriever and aspiration catheter for thrombolysis in cerebral infarction 2B revascularization.
Conclusion: The TCAR procedure offers a novel method for revascularization of carotid lesions; it does include its complications. While generally safe, access site complications such as pseudoaneurysms can always occur. Knowledge of this risk allows for appropriate surveillance and management should it occur.
Keywords: Ischemic stroke, Large-vessel occlusion, Thrombectomy, Transcarotid artery revascularization
INTRODUCTION
The trans carotid artery revascularization (TCAR) procedure is becoming increasingly popular as an alternative to carotid endarterectomy (CEA) or transfemoral carotid artery stenting (TFCAS) with recent data supporting the TCAR procedure as being as safe (CEA) or safer (TFCAS) in the appropriately selected patient.[
CASE REPORT
A 64-year-old man with a medical history notable for laryngeal cancer treated by resection, chemotherapy, and radiation underwent a left-sided TCAR procedure for symptomatic, severe carotid stenosis on July 21, 2023. He was discharged on 81 mg aspirin and clopidogrel after an uncomplicated stay but discontinued the aspirin due to reflux. On August 16, 2023, the patient awoke with aphasia, right arm weakness, and altered mental status with a last known normal time of 2230 the evening before. A computed tomography angiography was performed, demonstrating distal left M1 occlusion, and the patient was subsequently taken to the endovascular suite for mechanical thrombectomy.
A diagnostic cerebral angiogram was performed through an 8F arterial sheath in the right common femoral artery. The left common carotid was selected with the guide catheter, and an injection demonstrated thrombus within the previously placed carotid stent and a distal common carotid pseudoaneurysm [
Once the microcatheter and microwire were advanced distal to the occlusion, the aspiration catheter was advanced to the face of the occlusive thrombus and the stent-retriever was deployed. After 3 min, the stent-retriever was recaptured and removed from the patient under continuous aspiration through the aspiration catheter. A final angiograph demonstrated a thrombolysis in cerebral infarction 2B revascularization [
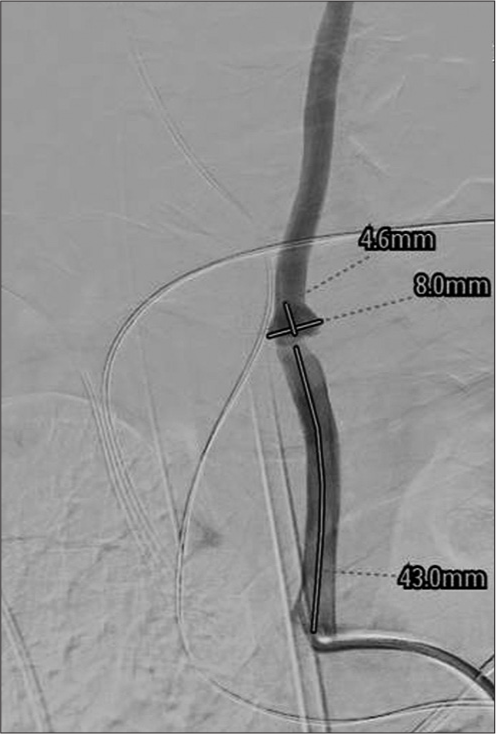
Three days later, when the patient was more stable, he was taken back to the endovascular suite for placement of a covered stent in the left common carotid [
DISCUSSION
Many practitioners have readily adopted direct carotid access with flow reversal through TCAR for its decreased risk of intraprocedural embolic injury and the ease of direct access rather than navigation through tortuous and often diseased vessels. Indeed, in the past eight years, since the Food and Drug Administration approved TCAR, the number of centers performing the procedure has increased from 29 to 606, and TCAR is utilized in approximately 1/4th of carotid stenosis cases in those institutions.[
Despite this widespread adoption, little has been reported on the complications associated with TCAR. In fact, multiple studies have demonstrated the comparable safety of TCAR to transfemoral carotid stenting or CEA in both patient outcomes and access site complications.[
Unfortunately, for those patients who experience an arterial injury that is either not recognized intraoperatively or occurs in a delayed fashion, the implications can be quite serious. Here, we present a case of TCAR-access site injury and a subsequent distal embolic LVO. While the risk of distal embolism was elevated in this patient after discontinuing the aspirin, this case emphasizes that direct carotid access carries its risks, particularly in the setting of previously irradiated vasculature with abnormal media and endothelium structure and function.[
Nevertheless, the development of and rapid increase in TCAR utilization offers an opportunity for improved patient outcomes given the previously demonstrated benefits of TCAR in properly selected patients.[
CONCLUSION
The benefits of TCAR have been demonstrated in both literature and practice as more practitioners move towards incorporating TCAR into the treatment of carotid stenosis. Despite this, there remains little data regarding the risk profile of TCAR. Here we present an LVO as a complication following a pseudoaneurysm at the carotid access site. Providers must take into consideration the risk with direct carotid access when utilizing TCAR.
Ethical approval
The research/study was approved by the Institutional Review Board at Piedmont Health, number 1953404-3, dated January 7, 2023.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Beeman BR, Kuhn BA, Recht MH, Muck PE, Schneider PA. Duplex ultrasound surveillance after transcarotid artery revascularization (TCAR) in clinical practice. Ann Vasc Surg. 2021. 72: 330-9
2. Cappellini CA, Zheng H, Lamb KM, Sooppan R, Coffey J, Luo RQ. Outcomes of transcarotid artery revascularization and carotid endarterectomy at a single institution. Ann Vasc Surg. 2021. 73: 329-35
3. Columbo JA, Stone DH, Martinez-Camblor P, Goodney PP, O’Malley AJ. Adoption and diffusion of transcarotid artery revascularization in contemporary practice. Circ Cardiovasc Interv. 2023. 16: e012805
4. Kashyap VS, King AH, Foteh MI, Janko M, Jim J, Motaganahalli RL. A multi-institutional analysis of transcarotid artery revascularization compared to carotid endarterectomy. J Vasc Surg. 2019. 70: 123-29
5. Malas MB, Dakour-Aridi H, Wang GJ, Kashyap VS, Motaganahalli RL, Eldrup-Jorgensen J. Transcarotid artery revascularization versus transfemoral carotid artery stenting in the Society for Vascular Surgery Vascular Quality Initiative. J Vasc Surg. 2019. 69: 92-103.e2
6. Meredith JS, Kuhn B, Muck P, Recht M, Kulwicki A, Broering M. Management of ruptured common carotid pseudoaneurysm following trans-carotid arterial revascularization in a patient with type III aortic arch. Ann Vasc Surg Brief Rep Innov. 2023. 3: 100174
7. Nardone R, Venturi A, Wieser A, Tezzon F, Carducci F, Windegger M. Vertebral artery dissection after radiation therapy: A case report. Eur Neurol. 2007. 57: 54-6
8. Suh D, Ma Y, Newton DH, Amendola MF, Lavingia KS. Carotid artery dissections from transcarotid artery revascularization as reported by the Food and Drug Administration. Vascular. 2023. p. 17085381231194410