- Section of Neurosurgery, Dartmouth-Hitchcock Medical Center, Lebanon, NH, USA
Correspondence Address:
Joon-Hyung Kim
Section of Neurosurgery, Dartmouth-Hitchcock Medical Center, Lebanon, NH, USA
DOI:10.4103/2152-7806.161408
Copyright: © 2015 Kim JH. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.How to cite this article: Kim J, Roberts DW, Bauer DF. CSF hydrothorax without intrathoracic catheter migration in children with ventriculoperitoneal shunt. Surg Neurol Int 23-Jul-2015;6:
How to cite this URL: Kim J, Roberts DW, Bauer DF. CSF hydrothorax without intrathoracic catheter migration in children with ventriculoperitoneal shunt. Surg Neurol Int 23-Jul-2015;6:. Available from: http://surgicalneurologyint.com/surgicalint_articles/csf-hydrothorax-without-intrathoracic-catheter-migration-in-children-with-ventriculoperitoneal-shunt/
Abstract
Background:Thoracic complications of ventriculoperitoneal (VP) shunts have been extensively reported in the literature. Cerebrospinal fluid (CSF) hydrothorax without catheter migration, however, has been rarely described and poorly understood.
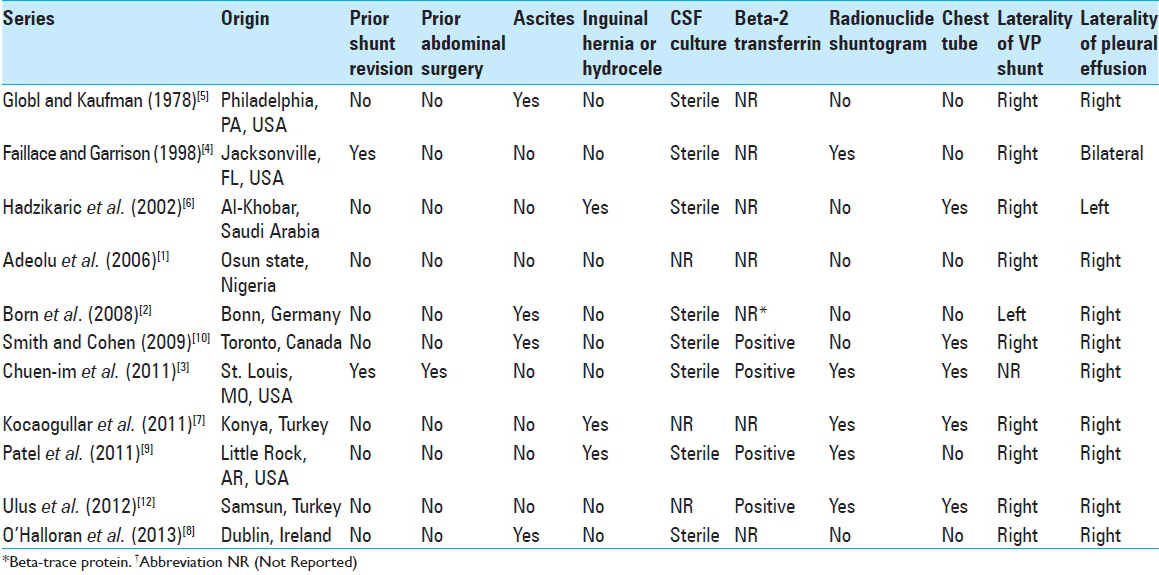
Case Description:We describe development of pleural effusion and respiratory distress in a 3-year-old boy with no evidence of VP shunt catheter displacement on plain radiograph and stable ventricle size on rapid sequence magnetic resonance imaging (MRI) brain. Chest X-ray revealed complete opacity of right hemithorax. Pleural effusion was consistent with transudate. Beta-2 transferrin returned positive. The patient underwent externalization of VP shunt, and upon resolution of effusion, re-internalization with new distal shunt catheter. A literature review of CSF hydrothorax in children without intrathoracic shunt migration was performed. Eleven cases were identified in the English literature. Age at VP shunt placement ranged from birth to 8 years of age. Interval from VP shunt placement to CSF hydrothorax ranged from 1.5 months to 5 years. History of shunt revision was reported in two cases. Presenting symptoms also included ascites and inguinal hernia or hydrocele. Reported diagnostic studies consist of CSF culture, radionuclide shuntogram, beta-2 transferrin, and beta-trace protein. Laterality of the VP shunt and development of pleural effusion were predominantly right sided. Definitive surgical treatment included VA shunt, repositioning of the peritoneal catheter, and endoscopic choroid plexus coagulation.
Conclusion:CSF hydrothorax is a rare thoracic complication of VP shunt placement with no radiographic evidence of shunt migration or malfunction. Postulated mechanisms include limited peritoneal capacity to resorb CSF in children and microscopic communications present in congenital diaphragmatic hiatuses.
Keywords: Cerebrospinal fluid hydrothorax, shunt malfunction, ventriculoperitoneal shunt
INTRODUCTION
Complications of ventriculoperitoneal (VP) shunt have been reported extensively in the literature. Thoracic manifestations include pleural effusion, bronchial perforation, pneumothorax, and pneumonia. Cerebrospinal fluid (CSF) pleural effusion in the absence of migration of distal VP shunt catheter in children, however, has been rarely described and poorly understood.[
CASE HISTORY
History and Examination
The patient is a 3-year-old boy born at 40 weeks by Cesarean section who initially presented with congenital hydrocephalus. He had right VP shunt placement at birth, with subsequent revisions at 13 and 23 months of age. He became symptomatic 10 days prior to presentation with progressive viral-like upper respiratory symptoms, including poor oral intake, intermittent fever, cough, irritability, and an ill appearance. Patient's co-morbidities include intractable epilepsy and craniosynostosis.
On examination, he was somnolent, but he would open his eyes spontaneously. He had full strength in all extremities. His shunt incisions and shunt track were nonerythematous and nontender. No swelling was seen along the track. He demonstrated intermittent cough with mild desaturations to 89%. Laboratory studies were within normal limits aside from mild thrombocytopenia (79 × 103/mcL) and elevated valproic acid level (183 mg/L; reference therapeutic range 50–100 mg/L).
Imaging
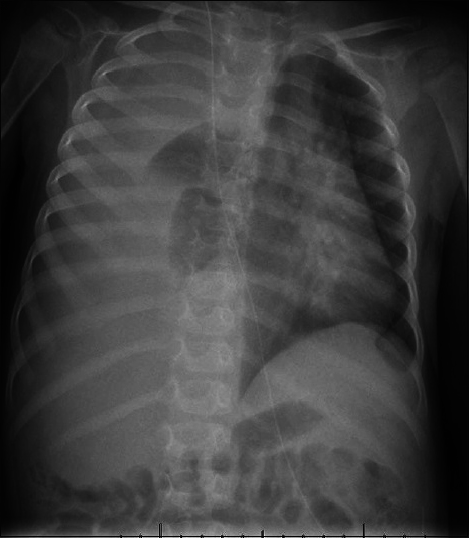
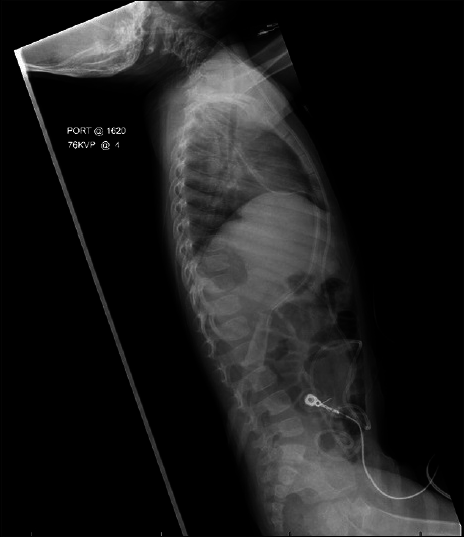
Chest radiograph revealed complete opacification of the right hemithorax with mediastinal displacement [
Hospital course
A chest tube was inserted on the right side with drainage of 800 ml of straw colored fluid under pressure. The fluid profile was that of a transudate without infection. The patient's mental status immediately improved. Chest tube output was brisk with 500 ml over the initial 24 h, and increasing to an output of approximately 50 ml/h. The valproic acid dose was decreased given the supratherapeutic level.
Beta-2 transferrin was sent from the chest tube drainage, resulting in a positive study. The final CSF culture was negative for infection. A decision was made to externalize the VP shunt at the abdomen, following which the chest tube output decreased considerably. The chest tube was placed to water seal with no re-accumulation of pleural fluid. The patient returned to the operating room for replacement and internalization of distal peritoneal tubing.
Postoperatively, the chest tube was maintained on water seal for 48 h without an increase in output. Serial ultrasound exam demonstrated no re-accumulation of pleural fluid, and the chest tube was subsequently removed. At 1 year follow-up, he has no re-accumulation of pleural fluid, and no signs or symptoms of shunt malfunction.
DISCUSSION
Upon initial presentation, the right chest opacity on chest radiograph was initially thought to be related to valproate toxicity resulting in an eosinophilic effusion. Consistent with this diagnosis was the patient's depressed mental state and thrombocytopenia. When the chest tube was inserted, however, pleural fluid analysis was negative for eosinophils. Pleural fluid was transudative with mostly macrophage predominant cellularity and no evidence of malignant cells. The patient did not have symptoms of common etiologies for transudative effusions, such as congestive heart failure (no cardiomegaly on chest X-ray, no S3 on auscultation, no hepatomegaly, normal pulses and blood pressure), nephrotic syndrome (normal urine output, normal serum albumin, no peripheral edema), and liver failure (normal hepatic function tests, normal coagulation tests). Despite improved respiratory status following pleural drainage, the patient continued to have persistent clear fluid drainage from his chest tube at approximately 50 ml/h. Beta-2 transferrin was sent, and its positive result confirmed the diagnosis of CSF hydrothorax.
Thoracic complications of VP shunts have been previously outlined into three categories:[
The mechanism of CSF hydrothorax in children without VP shunt catheter displacement remains less clear. Migration of CSF from the peritoneal to the pleural cavity depends on two factors: Malabsorption of CSF in the peritoneal cavity and open communication between the peritoneal and the pleural cavities to enable intraperitoneal CSF to pass into the pleural cavity.[
Conduits for intrathoracic catheter migration traditionally have been suggested to involve congenital diaphragmatic hiatuses, such as the anterior foramen of Morgagni and the posterior foramen of Bochdalek.[
In view of these mechanistic factors, a literature review of CSF hydrothorax in children without intrathoracic catheter migration was performed. A total of 11 pediatric cases of CSF hydrothorax without intrathoracic catheter migration were identified in the English literature [
Common presenting symptoms included ascites (N = 4) and inguinal hernia or hydrocele (N = 3). None of the patients with these symptoms had a history of shunt revision. It is widely accepted that very young children with poor abdominal re-absorptive capacity are susceptible to development of hydrocele or inguinal hernia following placement of VP shunt. While relatively little is known whether these presenting abdominal symptoms have any relation to CSF hydrothorax development, ascites appeared to occur mutually independent from inguinal hernia or hydrocele [
As reported in
A chest tube was placed in 5 of 11 cases (45%) for management of pleural effusion. Laterality of VP shunt was right-sided (82%), left-sided (9%), and not reported (9%). Pleural effusion developed in the right lung (82%), left lung (9%), and bilateral lungs (9%). While most VP shunts and resultant hydrothorax were right-sided, laterality of VP shunt did not overlap with concomitant hydrothorax when it occurred in the left.[
Final surgical treatment modalities ranged from ventriculo-atrial (VA) shunt placement (73%), reposition of peritoneal catheter (18%), and endoscopic choroid plexus coagulation (9%). Of eight patients in whom VA shunt was eventually placed, the catheter was externalized prior to VA shunt placement in two cases, and the peritoneal catheter was repositioned prior to VA shunt placement in one case. Externalization of a distal catheter may guide subsequent strategy for treatment, whether it is conversion to a VA shunt or replacement of the distal VP shunt catheter. Ventriculo-pleural shunt was attempted in one patient but subsequently had to be revised to a VA shunt. Further follow-up data may be useful for determination of long-term efficacy of various surgical revision modalities.
CONCLUSION
CSF hydrothorax is a rare but important complication of VP shunt placement in children without evidence of shunt migration or malfunction. Postulated mechanisms include limited peritoneal capacity to resorb CSF in children and microscopic communications present in congenital diaphragmatic hiatuses. In suspected cases, beta-2 transferrin assay and radionuclide tracer shunt series are useful diagnostic studies. CSF culture is commonly obtained to exclude infection. Thoracocentesis of pleural fluid or chest tube placement facilitates management of persistent pleural effusion. Externalization of the distal shunt catheter may resolve the hydrothorax and may guide subsequent treatment strategy.
References
1. Adeolu AA, Komolafe EO, Abiodun AA, Adetiloye VA. Symptomatic pleural effusion without intrathoracic migration of ventriculoperitoneal shunt catheter. Childs Nerv Syst. 2006. 22: 186-8
2. Born M, Reichling S, Schirrmeister J. Pleural effusion: Beta-trace protein in diagnosing ventriculoperitoneal shunt complications. J Child Neurol. 2008. 23: 810-2
3. Chuen-im P, Smyth MD, Segura B, Ferkol T, Rivera-Spoljaric K. Recurrent pleural effusion without intrathoracic migration of ventriculoperitoneal shunt catheter: A case report. Pediatr Pulmonol. 2012. 47: 91-5
4. Faillace WJ, Garrison RD. Hydrothorax after ventriculoperitoneal shunt placement in a premature infant: An iatrogenic postoperative complication. Case report. J Neurosurg. 1998. 88: 594-7
5. Glöbl HJ, Kaufmann HJ. Shunts and complications. Prog Pediatr Radiol. 1978. 6: 231-71
6. Hadzikaric N, Nasser M, Mashani A, Ammar A. CSF hydrothorax-VP shunt complication without displacement of a peritoneal catheter. Childs Nerv Syst. 2002. 18: 179-82
7. Kocaogullar Y, Guney O, Kaya B, Erdi F. CSF hydrothorax after ventriculoperitoneal shunt without catheter migration: A case report. Neurol Sci. 2011. 32: 949-52
8. O’Halloran PJ, Kaliaperumal C, Caird J. Chemotherapy-induced cerebrospinal fluid malabsorption in a shunted child: Case report and review of the literature. BMJ Case Rep. 2013. 2013: pii: bcr2012008255-
9. Patel AP, Dorantes-Argandar A, Raja AI. Cerebrospinal fluid hydrothorax without ventriculoperitoneal shunt migration in an infant. Pediatr Neurosurg. 2011. 47: 74-7
10. Smith JC, Cohen E. Beta-2-transferrin to detect cerebrospinal fluid pleural effusion: A case report. J Med Case Rep. 2009. 3: 6495-
11. Taub E, Lavyne MH. Thoracic complications of ventriculoperitoneal shunts: Case report and review of the literature. Neurosurgery. 1994. 34: 181-3
12. Ulus A, Kuruoglu E, Ozdemir SM, Yapici O, Sensoy G, Yarar E. CSF hydrothorax: Neither migration of peritoneal catheter into the chest nor ascites. Case report and review of the literature. Childs Nerv Syst. 2012. 28: 1843-8